Femoral Fracture in an Alpaca
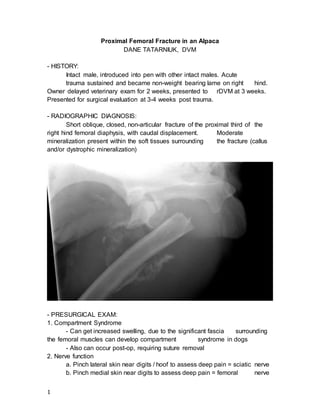
- 1. 1 Proximal Femoral Fracture in an Alpaca DANE TATARNIUK, DVM - HISTORY: Intact male, introduced into pen with other intact males. Acute trauma sustained and became non-weight bearing lame on right hind. Owner delayed veterinary exam for 2 weeks, presented to rDVM at 3 weeks. Presented for surgical evaluation at 3-4 weeks post trauma. - RADIOGRAPHIC DIAGNOSIS: Short oblique, closed, non-articular fracture of the proximal third of the right hind femoral diaphysis, with caudal displacement. Moderate mineralization present within the soft tissues surrounding the fracture (callus and/or dystrophic mineralization) - PRESURGICAL EXAM: 1. Compartment Syndrome - Can get increased swelling, due to the significant fascia surrounding the femoral muscles can develop compartment syndrome in dogs - Also can occur post-op, requiring suture removal 2. Nerve function a. Pinch lateral skin near digits / hoof to assess deep pain = sciatic nerve b. Pinch medial skin near digits to assess deep pain = femoral nerve
- 2. 2 - Partial deficits are OK, usually improve with fracture repair - Can get increased swelling, due to the significant fascia surrounding the femoral muscles can develop compartment syndrome in dogs - EXTERNAL STABILIZATION: 1. None - No external coaptation (ie, cast, bandage to stifle) is usually indicated. Cast or bandage up to stifle can act as pendulum weight that creates a fulcrum effect on the fracture site. 2. Spica Spint - Can use a spica splint in dogs but not practical in large animals - ANATOMY: 1. Greater trochanter: - insertion for middle gluteal, deep gluteal, piriform muscles 2. Lesser trochanter: - iliopsoas muscle 3. Third trochanter: - superficial gluteal muscle 4. Trochanteric fossa: - caudal on femoral neck, insertion for internal obturator, external obturator, gemelli muscles 5. Sciatic nerve: - courses over dorsal border of ischium, passes over caudal aspect of acetabulum - SURGICAL APPROACH: 1. Cranial-lateral - Most common. - Incise fascia lata along cranial border of biceps femoris muscle. -
- 3. Retract vastus lateral cranial and retract biceps formis caudally. - Exposes most of the diaphysis of the femur. - SURGICAL REPAIR THEORY: (Specific to transverse and short oblique fractures) 3 1. IM pins alone - Rotational and axial instability. - Can lead to nonunion - Predispose to osteomyelitis 2. Dynamic Compression Plates: - Create intrafragmentary compression - Proximal fractures, greater trochanter makes it difficult to contour plate appropriately to maximize bone to plate interface - Femur is unique, during weight bearing, medial cortex is subject to compression, lateral cortex subject to tension - Bone plates are applied to the lateral aspect
- 4. 4 3. Interlocking Nails - Useful, but no intrafragmentary compression - SURGICAL REPAIR ACTUALITY: - Routine cranial-lateral approach - Had to incise part of vastus lateralis transversely, as anatomy would not retract cranially far enough to facilitate visualization - Visualized sciatic nerve coursing from the caudal aspect of the greater trochanter, distally along the biceps femoris (caudal to the fracture) - Significant mineralization and fibrosis tissue present - Removed with rongeurs - Created significant bleeding = constant suction - Isolated both proximal and distal fracture - Reduced the fracture using Hohmann retractors - Significant remodeling of the fracture ends, no longer clearly congruent. Large, sharp fragment off of distal fracture not clearly compatible with proximal fracture margins. - Attempt to rotate the fracture planes to accompany the sharp fragment of the distal fracture, but results in significant lateralization (toe-ing out) of the limb. - Suspect some muscle contracture influencing malrotation of the proximal fracture (still connected to the Coxofemoral joint) - Decide to perform ostectomy of both the proximal and distal ends of the femur fracture. Approximately 1cm of length of bone removed. - Ostectomy facilitated adequate congruency of the femur for fracture fixation. - Placed pin retrograde through proximal fracture site, exiting through trochanteric fossa. Then aligned the proximal and distal fractured bones and drove IM pin normograde until it reached the metaphysis of the distal femur (used C-arm to ensure not in stifle joint) - Very important to be aware of where the sciatic nerve is located when doing IM pin placement (increased risk with retrograde placement vs. normograde) - In theory, IM pin should fill 30 to 40% of medullary cavity - Aware that we would be applying bone plate to lateral aspect of fracture. Used smaller IM pin to increase ability to place bicorticol screws (otherwise would have to place monocorticol screws) - Following IM pin placement, then placed hook plate (pre-bent) such that the hook of the plate is situated on the greater trochanter of the
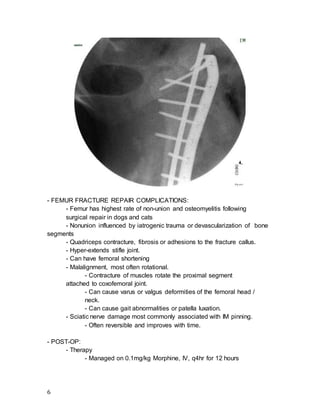
- 5. 5 femur. - Hook Plate: 3.5 narrow dynamic compression plate, 8 holes - Two prongs count as AO sites of fixation - Hook plate set comes with a specific grill guide that allows you to situate the two drill holes on the greater trochanter of the femur, at an exact distance from each other - Fixate the plate by making two 2.5mm drill holes for the prongs of the plate (using the drill guide) and then taping the plate in place with a mallot (such that the prongs are now in the drilled guide holes) and plate is aligned on the femur. - Then, placed remainder of screws in neutral fashion - Screws placed bicorticol, one screw clearly had some interaction with IM pin with tightening (threads of screw touching IM pin) - Confirm that screws in proximal aspect of the femur follow into the femoral neck but do not engage Coxofemoral joint using C-arm - Fibrous callus on medial aspect of femur made using depth gauge difficult (some screws too long) - After application of hook bone plate, copious lavage - Sutured various muscle and fasial layers, #0 PDS - Sutured skin, interrupted cruciates, #0 Ethilon - Ioban for recovery - FLUROSCOPIC IMAGE, POST OP:
- 6. - FEMUR FRACTURE REPAIR COMPLICATIONS: 6 - Femur has highest rate of non-union and osteomyelitis following surgical repair in dogs and cats - Nonunion influenced by iatrogenic trauma or devascularization of bone segments - Quadriceps contracture, fibrosis or adhesions to the fracture callus. - Hyper-extends stifle joint. - Can have femoral shortening - Malalignment, most often rotational. - Contracture of muscles rotate the proximal segment attached to coxofemoral joint. - Can cause varus or valgus deformities of the femoral head / neck. - Can cause gait abnormalities or patella luxation. - Sciatic nerve damage most commonly associated with IM pinning. - Often reversible and improves with time. - POST-OP: - Therapy - Managed on 0.1mg/kg Morphine, IV, q4hr for 12 hours
- 7. 7 - Managed on 1.1mg/kg Flunixin meglumine, q12hr for 72 hours - Managed on 2.2mg/kg Ceftiofur, q12hr for 5 days - Anemia - Decreased from PCV 32% pre-op, down to 15% post-op - Part due to blood loss intra-op - Part due to Mycoplasma hemolamae infection - Organism active in times of stress = hemolysis - Administered 20mg/kg Oxytetracycline, every 3rd day, for 3 doses