FOLIC ACID DEFICIENCY I N CLINICAL PRACTICEpptx
Download as PPTX, PDF0 likes55 views
FOLIC ACID DEFICIENCY, CAUSES , EVALUATION AND ITS MANAGEMENT
1 of 17
Download to read offline













Recommended
folicaciddeficiency-230725062219-7281efe9.pdf



folicaciddeficiency-230725062219-7281efe9.pdfUmairFirdous
╠²
This document summarizes folic acid deficiency, including its physiologic roles, clinical presentation, investigations, treatment, and prevention. It notes that folic acid is important for DNA and RNA synthesis and hematopoiesis. Deficiency can cause macrocytic anemia and megaloblastic changes in the bone marrow. It is investigated through CBC, serum and RBC folate levels, and metabolic testing. Treatment involves oral folic acid supplementation.FOLIC ACID DEFICIENCY.pptx



FOLIC ACID DEFICIENCY.pptxDR Venkata Ramana
╠²
This document summarizes folic acid deficiency, including its physiologic roles, clinical presentation, investigations, treatment, and prevention. It notes that folic acid is important for DNA and RNA synthesis and hematopoiesis. Deficiency can cause macrocytic anemia and megaloblastic changes in the bone marrow. It is investigated through CBC, serum and red blood cell folate levels, and metabolites. Treatment involves oral folic acid supplementation.FOLIC ACID DEFICIENCY.pptx



FOLIC ACID DEFICIENCY.pptxDR Venkata Ramana
╠²
Folic acid deficiency can cause megaloblastic anemia due to its critical role in DNA synthesis. Clinical presentations include macrocytic anemia, gastrointestinal symptoms, and neurological changes. Diagnosis involves blood tests showing anemia, macrocytes, hypersegmented neutrophils, and low serum and red blood cell folate levels. Treatment is oral folic acid supplementation, while prevention involves folic acid fortification and supplementation for at-risk groups like pregnant women.Megaloblastic Anemia by Dr. Sookun Rajeev Kumar



Megaloblastic Anemia by Dr. Sookun Rajeev KumarDr. Sookun Rajeev Kumar
╠²
Megaloblastic anemia is caused by a defect in DNA synthesis due to deficiencies in vitamin B12 or folate. It is characterized by abnormal bone marrow erythroblasts with delayed nuclear development. Causes include dietary deficiencies, malabsorption, increased cell turnover, and drugs. Treatment involves transfusion, vitamin B12 injections or oral folic acid supplementation depending on the underlying deficiency.1479713317-hypocalcemia.ppt



1479713317-hypocalcemia.pptDanielLuka2
╠²
This document discusses hypocalcemia (low calcium levels in the blood). It defines hypocalcemia and describes its clinical manifestations such as muscle cramps and seizures. It lists various causes of hypocalcemia including parathyroid hormone deficiency, pseudohypoparathyroidism, and vitamin D deficiency. The document provides details on evaluating the etiology of hypocalcemia and its treatment including calcium supplementation. It also discusses related conditions like rickets, which is the lack of bone mineralization in children.vitamin b12 deficiency in clinical practicepptx



vitamin b12 deficiency in clinical practicepptxDR Venkata Ramana
╠²
vitamin b12 deficiency causes, evaluation and managementMegaloblastic anaemia (lecture for v year mbbs)



Megaloblastic anaemia (lecture for v year mbbs)mona aziz
╠²
Megaloblastic anemia results from vitamin B12 or folic acid deficiency. It causes impaired DNA synthesis and nucleocytoplasmic asynchrony in proliferating cells. Deficiencies in vitamin B12 or folic acid lead to elevated homocysteine and impaired conversion of uracil to thymidine, arresting cell development. This causes megaloblastic changes notably in the bone marrow and gastrointestinal tract. Neurological changes in B12 deficiency are due to demyelination. Investigations show macrocytic anemia and megaloblastic bone marrow changes. Treatment involves vitamin B12 injections and oral folic acid supplementation.Approach to Anemic Child [Autosaved].pptx![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
Approach to Anemic Child [Autosaved].pptxAbenezerLemma5
╠²
it's about hematologic diseases in pediatrics ANEMIA



ANEMIAbera_rajarshi
╠²
Anemia is defined as a reduction in red blood cells or hemoglobin levels below normal. It can be caused by nutritional deficiencies like iron deficiency, impaired red blood cell production like in megaloblastic anemia, or genetic disorders such as sickle cell anemia, thalassemia, and hereditary spherocytosis. Treatment depends on the underlying cause but may include oral or intravenous iron supplementation, vitamin B12 or folate, blood transfusions, or managing symptoms during sickle cell crises.Anemia



AnemiaTagore medical College
╠²
This document discusses anemia, including its definition, classification, causes, symptoms, diagnostic tests, and treatment. It defines anemia as a reduction in red blood cells or hemoglobin. Anemia is classified morphologically based on cell size and shape or etiologically based on cause. Common causes include iron deficiency, megaloblastic anemia related to B12 or folate deficiency, sickle cell anemia, thalassemia, and anemia of chronic disease. Diagnostic tests include complete blood count, blood smear, and iron/B12/folate levels. Treatment depends on the underlying cause but may include oral/IV iron, B12/folate supplements, blood transfusions, or splen10 anemia



10 anemiaGyanendra Raj Joshi
╠²
This document discusses various types of anemia. It defines anemia as a reduction in hemoglobin levels and describes the most common causes as iron deficiency and nutritional deficiencies. Specific types discussed in detail include iron deficiency anemia, megaloblastic anemia caused by vitamin B12 and folate deficiencies, sickle cell anemia caused by an abnormal hemoglobin gene, thalassemias caused by genetic defects in hemoglobin production, and G6PD deficiency which affects the ability to prevent oxidative damage to red blood cells. The document covers epidemiology, pathophysiology, clinical manifestations, investigations, and treatments for each type.Megaloblastic anaemia



Megaloblastic anaemiaABHIJIT BHOYAR
╠²
This document provides information about megaloblastic anemia in children through a seminar presentation. It begins with an overview of hematology and the components of blood. It then discusses the causes of megaloblastic anemia as deficiencies in vitamins B12 and folic acid. The pathophysiology is described as impaired cell division leading to enlarged red blood cells called megaloblasts. Clinical manifestations include weakness, pale skin, and neurological issues. Diagnostic tests include blood counts and smears to examine red blood cells. Management involves vitamin B12 or folic acid supplementation through oral or injectable routes. Nursing care focuses on risks of ineffective tissue perfusion and activity intolerance due to anemia.Serum albumin



Serum albuminjamali gm
╠²
This document discusses serum albumin and nephrotic syndrome. It provides details on serum albumin such as its abundance in plasma, synthesis in the liver, and role as a carrier of various substances. It then describes nephrotic syndrome as a clinical condition characterized by proteinuria, hypoalbuminemia, hypercoagulability, and hypertension. The document outlines primary and secondary causes of nephrotic syndrome including minimal change disease, focal segmental glomerulosclerosis, and diabetic nephropathy. It also discusses renal tubular acidosis and its classification into four types based on the tubular site of dysfunction.Anemia in renal disease3



Anemia in renal disease3Pediatric Nephrology
╠²
Renal disease may produce disturbances in red blood cells, white blood cells, platelets, and coagulation factors
the abnormalities do not parallel the status of renal function but rather reflect the activity of the disease process that results in renal dysfunction.
vitamin b12 deficiency.pptx



vitamin b12 deficiency.pptxDR Venkata Ramana
╠²
Vitamin B12 deficiency is a potentially serious condition that can affect multiple body systems. It presents as macrocytic anemia but can also cause neurological abnormalities and gastrointestinal issues. Vitamin B12 is essential for DNA synthesis and hematopoiesis. It is absorbed in the ileum with the help of intrinsic factor. Causes of deficiency include pernicious anemia, gastrointestinal disorders, vegetarian diets, and certain medications. Deficiency is diagnosed based on low B12 levels and hematological and neurological examination findings.Approach to anemia



Approach to anemiaFerhad Shakir
╠²
This document discusses the approach to diagnosing and classifying anemia. It defines anemia and notes that normal hemoglobin levels vary by age, gender, and race. A thorough history and physical exam can reveal potential causes like diet, blood loss, infections, or medications. Laboratory tests including a CBC, smear, and reticulocyte count help classify anemias as microcytic, normocytic, or macrocytic based on red blood cell size. Iron deficiency is a common cause of anemia in children. Hemolytic disorders cause shortened red blood cell survival.Folic Acid and B12.pptx



Folic Acid and B12.pptxNarendra Sharma
╠²
Folic acid and vitamin B12 are water soluble vitamins that play important roles in DNA synthesis and methylation reactions. Folic acid helps form red blood cells and genetic material, while vitamin B12 is involved in myelin production for nerve cells. Deficiencies can cause megaloblastic anemia and neurological issues. Dietary sources include leafy greens, liver, and fortified foods. Absorption involves conjugation and binding proteins, with metabolism intertwined between the vitamins. Testing of blood levels aids diagnosis of deficiency diseases.Thalassemia Unveiled: Insights into Diagnosis, Treatment, and Care.pptx



Thalassemia Unveiled: Insights into Diagnosis, Treatment, and Care.pptxNoorulainMehmood1
╠²
Thalassemia, a group of inherited blood disorders, presents a complex interplay of genetic mutations and clinical manifestations. This presentation delves into the intricacies of thalassemia, exploring its genetic underpinnings, clinical spectrum, diagnostic modalities, and therapeutic approaches. Through comprehensive analysis and case studies, attendees will gain a deeper understanding of thalassemia's impact on patients' lives and the latest advancements in management strategies.
Keywords:
Thalassemia
Genetic Disorders
Hemoglobinopathies
Blood Disorders
Anemia
Genetic Mutations
Clinical Spectrum
Diagnosis
Treatment Modalities
Transfusion Therapy
Iron Chelation Therapy
Genetic Counseling
Patient Care
Hematological Disorders
Research AdvancementsLipid disorders 



Lipid disorders DR. JITHIN GEORGE
╠²
This document discusses lipid disorders and their causes and treatment. It covers apolipoproteins, dyslipidemia caused by excessive VLDL secretion or impaired lipolysis of triglyceride-rich lipoproteins, and dyslipidemia caused by impaired hepatic uptake of apoB-containing lipoproteins. Specific genetic disorders discussed include familial hypercholesterolemia, familial hypertriglyceridemia, sitosterolemia, and others. Lifestyle modifications and pharmacological treatments are provided for each condition.Anemia



AnemiaDr Muhammad Mustansar
╠²
This document discusses anemia, including its definition, classification, causes, symptoms, diagnosis, and treatment. It covers iron deficiency anemia in depth and discusses its stages, signs, and tests. It also covers other nutritional anemias like megaloblastic anemia caused by vitamin B12 or folate deficiencies, copper deficiency anemia, and sideroblastic anemia. Non-nutritional anemias discussed include anemia of chronic disease, sickle cell anemia, thalassemia, and sports anemia. Proper diagnosis is important before providing nutritional or medical management of anemia.Anemia in Child



Anemia in ChildShaliniShal11
╠²
This document discusses the evaluation and management of a child with anemia. It begins by defining anemia and describing common causes including nutritional deficiencies, blood loss, and blood cell destruction. Assessment involves patient history, physical exam, and hematological lab tests to identify the underlying cause. Different types of anemia are classified based on red blood cell size and morphology. Specific conditions like iron deficiency anemia, B12/folate deficiency, hereditary spherocytosis, glucose-6-phosphate dehydrogenase deficiency, and sickle cell anemia are then discussed in detail regarding their presentation, evaluation, and treatment.SICKLE CELL DISEASE.pptx



SICKLE CELL DISEASE.pptxDR Venkata Ramana
╠²
Sickle cell disease is caused by mutations in the beta-globin gene resulting in abnormal hemoglobin S. This leads to polymerization of deoxygenated hemoglobin S and distortion of red blood cells into a sickle shape. Chronic hemolysis and vaso-occlusive crises cause significant morbidity. Diagnosis is made through hemoglobin electrophoresis showing elevated HbS. Treatment involves prophylactic antibiotics, hydration, pain management, hydroxyurea and blood transfusions to reduce complications. Chronic organ damage remains a major cause of mortality in patients with sickle cell disease.Anemia 2011



Anemia 2011Patrick Carter
╠²
This document discusses various types of anemia, including their definitions, pathophysiology, clinical presentations, diagnostic evaluations, and treatments. It covers iron deficiency anemia, vitamin B12 and folate deficiency anemias, thalassemias, sickle cell disease, and other hereditary and acquired anemias. Evaluation includes complete blood count, peripheral smear, iron studies, and other tests depending on suspected etiology. Management involves treating the underlying cause, such as iron or vitamin supplementation.Thalasemia.pptx



Thalasemia.pptxsaifurrahmanSapai
╠²
Thalassemia is a hereditary blood disorder caused by reduced or absent globin chain synthesis. There are two main types - alpha and beta thalassemia. Beta thalassemia results from mutations in the beta globin genes and causes a reduction in or absence of beta chain production. This leads to imbalanced alpha/beta chain ratios, hemolysis of red blood cells, and anemia. Patients are classified by disease severity into thalassemia minor, intermedia, or major. Treatment involves regular blood transfusions coupled with iron chelation therapy to prevent iron overload, as well as splenectomy and stem cell transplantation or gene therapy in severe cases. Complications arise from chronic anemia, transf anemia- oral health



anemia- oral healthBala Vidyadhar
╠²
This document provides an overview of anemia, including its classification, diagnosis, clinically significant variants, and treatment with drug therapy. It discusses the morphological, etiological, and quantitative classification of anemia. The clinically significant variants covered are iron deficiency anemia, pernicious anemia, megaloblastic anemia, sickle cell anemia, thalassemia, and aplastic anemia. It also outlines the diagnosis of anemia through laboratory tests and symptoms. The treatment section focuses on drug therapy for iron deficiency anemia, including oral and parenteral iron supplementation, and managing iron overload and B12/folate deficiencies.blood and blood components in medicine.pptx



blood and blood components in medicine.pptxDR Venkata Ramana
╠²
components of blood, blood transfusion reactions and its managementApproach to macrocytic anemia.......pptx



Approach to macrocytic anemia.......pptxDR Venkata Ramana
╠²
Macrocytic anemia causes and its evaluationMore Related Content
Similar to FOLIC ACID DEFICIENCY I N CLINICAL PRACTICEpptx (20)
Approach to Anemic Child [Autosaved].pptx![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
![Approach to Anemic Child [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/approachtoanemicchildautosaved-240427131658-64d6d32d-thumbnail.jpg?width=560&fit=bounds)
Approach to Anemic Child [Autosaved].pptxAbenezerLemma5
╠²
it's about hematologic diseases in pediatrics ANEMIA



ANEMIAbera_rajarshi
╠²
Anemia is defined as a reduction in red blood cells or hemoglobin levels below normal. It can be caused by nutritional deficiencies like iron deficiency, impaired red blood cell production like in megaloblastic anemia, or genetic disorders such as sickle cell anemia, thalassemia, and hereditary spherocytosis. Treatment depends on the underlying cause but may include oral or intravenous iron supplementation, vitamin B12 or folate, blood transfusions, or managing symptoms during sickle cell crises.Anemia



AnemiaTagore medical College
╠²
This document discusses anemia, including its definition, classification, causes, symptoms, diagnostic tests, and treatment. It defines anemia as a reduction in red blood cells or hemoglobin. Anemia is classified morphologically based on cell size and shape or etiologically based on cause. Common causes include iron deficiency, megaloblastic anemia related to B12 or folate deficiency, sickle cell anemia, thalassemia, and anemia of chronic disease. Diagnostic tests include complete blood count, blood smear, and iron/B12/folate levels. Treatment depends on the underlying cause but may include oral/IV iron, B12/folate supplements, blood transfusions, or splen10 anemia



10 anemiaGyanendra Raj Joshi
╠²
This document discusses various types of anemia. It defines anemia as a reduction in hemoglobin levels and describes the most common causes as iron deficiency and nutritional deficiencies. Specific types discussed in detail include iron deficiency anemia, megaloblastic anemia caused by vitamin B12 and folate deficiencies, sickle cell anemia caused by an abnormal hemoglobin gene, thalassemias caused by genetic defects in hemoglobin production, and G6PD deficiency which affects the ability to prevent oxidative damage to red blood cells. The document covers epidemiology, pathophysiology, clinical manifestations, investigations, and treatments for each type.Megaloblastic anaemia



Megaloblastic anaemiaABHIJIT BHOYAR
╠²
This document provides information about megaloblastic anemia in children through a seminar presentation. It begins with an overview of hematology and the components of blood. It then discusses the causes of megaloblastic anemia as deficiencies in vitamins B12 and folic acid. The pathophysiology is described as impaired cell division leading to enlarged red blood cells called megaloblasts. Clinical manifestations include weakness, pale skin, and neurological issues. Diagnostic tests include blood counts and smears to examine red blood cells. Management involves vitamin B12 or folic acid supplementation through oral or injectable routes. Nursing care focuses on risks of ineffective tissue perfusion and activity intolerance due to anemia.Serum albumin



Serum albuminjamali gm
╠²
This document discusses serum albumin and nephrotic syndrome. It provides details on serum albumin such as its abundance in plasma, synthesis in the liver, and role as a carrier of various substances. It then describes nephrotic syndrome as a clinical condition characterized by proteinuria, hypoalbuminemia, hypercoagulability, and hypertension. The document outlines primary and secondary causes of nephrotic syndrome including minimal change disease, focal segmental glomerulosclerosis, and diabetic nephropathy. It also discusses renal tubular acidosis and its classification into four types based on the tubular site of dysfunction.Anemia in renal disease3



Anemia in renal disease3Pediatric Nephrology
╠²
Renal disease may produce disturbances in red blood cells, white blood cells, platelets, and coagulation factors
the abnormalities do not parallel the status of renal function but rather reflect the activity of the disease process that results in renal dysfunction.
vitamin b12 deficiency.pptx



vitamin b12 deficiency.pptxDR Venkata Ramana
╠²
Vitamin B12 deficiency is a potentially serious condition that can affect multiple body systems. It presents as macrocytic anemia but can also cause neurological abnormalities and gastrointestinal issues. Vitamin B12 is essential for DNA synthesis and hematopoiesis. It is absorbed in the ileum with the help of intrinsic factor. Causes of deficiency include pernicious anemia, gastrointestinal disorders, vegetarian diets, and certain medications. Deficiency is diagnosed based on low B12 levels and hematological and neurological examination findings.Approach to anemia



Approach to anemiaFerhad Shakir
╠²
This document discusses the approach to diagnosing and classifying anemia. It defines anemia and notes that normal hemoglobin levels vary by age, gender, and race. A thorough history and physical exam can reveal potential causes like diet, blood loss, infections, or medications. Laboratory tests including a CBC, smear, and reticulocyte count help classify anemias as microcytic, normocytic, or macrocytic based on red blood cell size. Iron deficiency is a common cause of anemia in children. Hemolytic disorders cause shortened red blood cell survival.Folic Acid and B12.pptx



Folic Acid and B12.pptxNarendra Sharma
╠²
Folic acid and vitamin B12 are water soluble vitamins that play important roles in DNA synthesis and methylation reactions. Folic acid helps form red blood cells and genetic material, while vitamin B12 is involved in myelin production for nerve cells. Deficiencies can cause megaloblastic anemia and neurological issues. Dietary sources include leafy greens, liver, and fortified foods. Absorption involves conjugation and binding proteins, with metabolism intertwined between the vitamins. Testing of blood levels aids diagnosis of deficiency diseases.Thalassemia Unveiled: Insights into Diagnosis, Treatment, and Care.pptx



Thalassemia Unveiled: Insights into Diagnosis, Treatment, and Care.pptxNoorulainMehmood1
╠²
Thalassemia, a group of inherited blood disorders, presents a complex interplay of genetic mutations and clinical manifestations. This presentation delves into the intricacies of thalassemia, exploring its genetic underpinnings, clinical spectrum, diagnostic modalities, and therapeutic approaches. Through comprehensive analysis and case studies, attendees will gain a deeper understanding of thalassemia's impact on patients' lives and the latest advancements in management strategies.
Keywords:
Thalassemia
Genetic Disorders
Hemoglobinopathies
Blood Disorders
Anemia
Genetic Mutations
Clinical Spectrum
Diagnosis
Treatment Modalities
Transfusion Therapy
Iron Chelation Therapy
Genetic Counseling
Patient Care
Hematological Disorders
Research AdvancementsLipid disorders 



Lipid disorders DR. JITHIN GEORGE
╠²
This document discusses lipid disorders and their causes and treatment. It covers apolipoproteins, dyslipidemia caused by excessive VLDL secretion or impaired lipolysis of triglyceride-rich lipoproteins, and dyslipidemia caused by impaired hepatic uptake of apoB-containing lipoproteins. Specific genetic disorders discussed include familial hypercholesterolemia, familial hypertriglyceridemia, sitosterolemia, and others. Lifestyle modifications and pharmacological treatments are provided for each condition.Anemia



AnemiaDr Muhammad Mustansar
╠²
This document discusses anemia, including its definition, classification, causes, symptoms, diagnosis, and treatment. It covers iron deficiency anemia in depth and discusses its stages, signs, and tests. It also covers other nutritional anemias like megaloblastic anemia caused by vitamin B12 or folate deficiencies, copper deficiency anemia, and sideroblastic anemia. Non-nutritional anemias discussed include anemia of chronic disease, sickle cell anemia, thalassemia, and sports anemia. Proper diagnosis is important before providing nutritional or medical management of anemia.Anemia in Child



Anemia in ChildShaliniShal11
╠²
This document discusses the evaluation and management of a child with anemia. It begins by defining anemia and describing common causes including nutritional deficiencies, blood loss, and blood cell destruction. Assessment involves patient history, physical exam, and hematological lab tests to identify the underlying cause. Different types of anemia are classified based on red blood cell size and morphology. Specific conditions like iron deficiency anemia, B12/folate deficiency, hereditary spherocytosis, glucose-6-phosphate dehydrogenase deficiency, and sickle cell anemia are then discussed in detail regarding their presentation, evaluation, and treatment.SICKLE CELL DISEASE.pptx



SICKLE CELL DISEASE.pptxDR Venkata Ramana
╠²
Sickle cell disease is caused by mutations in the beta-globin gene resulting in abnormal hemoglobin S. This leads to polymerization of deoxygenated hemoglobin S and distortion of red blood cells into a sickle shape. Chronic hemolysis and vaso-occlusive crises cause significant morbidity. Diagnosis is made through hemoglobin electrophoresis showing elevated HbS. Treatment involves prophylactic antibiotics, hydration, pain management, hydroxyurea and blood transfusions to reduce complications. Chronic organ damage remains a major cause of mortality in patients with sickle cell disease.Anemia 2011



Anemia 2011Patrick Carter
╠²
This document discusses various types of anemia, including their definitions, pathophysiology, clinical presentations, diagnostic evaluations, and treatments. It covers iron deficiency anemia, vitamin B12 and folate deficiency anemias, thalassemias, sickle cell disease, and other hereditary and acquired anemias. Evaluation includes complete blood count, peripheral smear, iron studies, and other tests depending on suspected etiology. Management involves treating the underlying cause, such as iron or vitamin supplementation.Thalasemia.pptx



Thalasemia.pptxsaifurrahmanSapai
╠²
Thalassemia is a hereditary blood disorder caused by reduced or absent globin chain synthesis. There are two main types - alpha and beta thalassemia. Beta thalassemia results from mutations in the beta globin genes and causes a reduction in or absence of beta chain production. This leads to imbalanced alpha/beta chain ratios, hemolysis of red blood cells, and anemia. Patients are classified by disease severity into thalassemia minor, intermedia, or major. Treatment involves regular blood transfusions coupled with iron chelation therapy to prevent iron overload, as well as splenectomy and stem cell transplantation or gene therapy in severe cases. Complications arise from chronic anemia, transf anemia- oral health



anemia- oral healthBala Vidyadhar
╠²
This document provides an overview of anemia, including its classification, diagnosis, clinically significant variants, and treatment with drug therapy. It discusses the morphological, etiological, and quantitative classification of anemia. The clinically significant variants covered are iron deficiency anemia, pernicious anemia, megaloblastic anemia, sickle cell anemia, thalassemia, and aplastic anemia. It also outlines the diagnosis of anemia through laboratory tests and symptoms. The treatment section focuses on drug therapy for iron deficiency anemia, including oral and parenteral iron supplementation, and managing iron overload and B12/folate deficiencies.More from DR Venkata Ramana (20)
blood and blood components in medicine.pptx



blood and blood components in medicine.pptxDR Venkata Ramana
╠²
components of blood, blood transfusion reactions and its managementApproach to macrocytic anemia.......pptx



Approach to macrocytic anemia.......pptxDR Venkata Ramana
╠²
Macrocytic anemia causes and its evaluationApproach to edema in clinical practice..



Approach to edema in clinical practice..DR Venkata Ramana
╠²
Edema causes, pathophysiology, investigations and management of edemakidney function tests and its interpretation



kidney function tests and its interpretationDR Venkata Ramana
╠²
assessment of kidney function by kidney function testsIRON DEFICIENCY ANEMIA IN PREGNANCY pptx



IRON DEFICIENCY ANEMIA IN PREGNANCY pptxDR Venkata Ramana
╠²
ANEMIA IN PREGNANCY CAUSES, AND MANAGEMENT OF IRON DEFICIENCYSPLEEN ANATOMY,FUNCTIONS,EXAMINATION & APPROACH TO SPLENOMEGALY



SPLEEN ANATOMY,FUNCTIONS,EXAMINATION & APPROACH TO SPLENOMEGALYDR Venkata Ramana
╠²
APPROACH TO SPLENOMEGALYIron deficiency anemia in pregnancy.pptx



Iron deficiency anemia in pregnancy.pptxDR Venkata Ramana
╠²
iron deficiency anemia in pregnancy and its managementchronic diarrhea causes and evaluation pptx



chronic diarrhea causes and evaluation pptxDR Venkata Ramana
╠²
chronic diarrhea causes and evaluation of chronic diarrheaACUTE DIARRHEA IN CHILDREN AND ADULTS.pptx



ACUTE DIARRHEA IN CHILDREN AND ADULTS.pptxDR Venkata Ramana
╠²
ACUTE DIARRHEA ETIOLOGY,CLINICAL FEATURES AND MANAGEMENT OF DIARRHEA1.MITRAL STENOSIS AND ITS MANAGEMENT....



1.MITRAL STENOSIS AND ITS MANAGEMENT....DR Venkata Ramana
╠²
MITRAL STENOSIS,CAUSES,PATHOGENESIS,CLINICAL FEATURES,DIAGNOSIS AND MANAGEMENTRecently uploaded (20)
Local Anesthetic Use in the Vulnerable Patients



Local Anesthetic Use in the Vulnerable PatientsReza Aminnejad
╠²
Local anesthetics are a cornerstone of pain management, but their use requires special consideration in vulnerable groups such as pediatric, elderly, diabetic, or obese patients. In this presentation, weŌĆÖll explore how factors like age and physiology influence local anesthetics' selection, dosing, and safety. By understanding these differences, we can optimize patient care and minimize risks.
BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptx



BIOMECHANICS OF THE MOVEMENT OF THE SHOULDER COMPLEX.pptxdrnidhimnd
╠²
The shoulder complex acts as in coordinated fashion to provide the smoothest and greatest range of motion possible of the upper limb.
Combined motion of GH and ST joint of shoulder complex helps in:
Distribution of motion between other two joints.
Maintenance of glenoid fossa in optimal position.
Maintenance of good length tension
Although some amount of glenohumeral motion may occur while the other shoulder articulations remain stabilized, movement of the humerus more commonly involves some movement at all three shoulder joints.
CreatineŌĆÖs Untold Story and How 30-Year-Old Lessons Can Shape the Future



CreatineŌĆÖs Untold Story and How 30-Year-Old Lessons Can Shape the FutureSteve Jennings
╠²
Creatine burst into the public consciousness in 1992 when an investigative reporter inside the Olympic Village in Barcelona caught wind of British athletes using a product called Ergomax C150. This led to an explosion of interest in ŌĆō and questions about ŌĆō the ingredient after high-profile British athletes won multiple gold medals.
I developed Ergomax C150, working closely with the late and great Dr. Roger Harris (1944 ŌĆö 2024), and Prof. Erik Hultman (1925 ŌĆö 2011), the pioneering scientists behind the landmark studies of creatine and athletic performance in the early 1990s.
Thirty years on, these are the slides I used at the Sports & Active Nutrition Summit 2025 to share the story, the lessons from that time, and how and why creatine will play a pivotal role in tomorrowŌĆÖs high-growth active nutrition and healthspan categories.Diabetic Ketoacidosis (DKA) & Its Management Protocol



Diabetic Ketoacidosis (DKA) & Its Management ProtocolDr Anik Roy Chowdhury
╠²
Dr. Anik Roy Chowdhury
MBBS, BCS(Health), DA, MD (Resident)
Department of Anesthesiology, ICU & Pain Medicine
Shaheed Suhrawardy Medical College Hospital (ShSMCH)HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLE



HUMAN SEXUALITY AND SEXUAL RESPONCE CYCLEdaminipatel37
╠²
It is all about topic of obg for new semester students physiology 1 T3T4 & Jaundice & capillary circulation ž│žżž¦┘ä.pptx



physiology 1 T3T4 & Jaundice & capillary circulation ž│žżž¦┘ä.pptxamralmohammady27
╠²
┘ä┘ł ž╣┘åž»┘ā ┘䞦ž© ž¬┘łž© žŻ┘ł ž¬ž¦ž©┘䞬 ┘üž¦┘ä
power point show
┘ć┘Ŗ┘å┘üž╣┘ā ž¼ž»ž¦ ┘ü┘Ŗ ┘ģž▒ž¦ž¼ž╣ž® ž│ž▒┘Ŗž╣ž® ┘ä┘Ŗ┘äž® ž¦┘䞦┘ģž¬žŁž¦┘å
┘łž¦┘ä┘ä┘Ŗ ┘Ŗ┘éž»ž▒ ┘Ŗž╣┘ģ┘ä žŁž¦ž¼ž® ┘Ŗž╣┘ģ┘ä┘枦
┘łž┤┘āž▒ž¦ ┘ä┘äž»┘āž¬┘łž▒ž® ┘å┘łž¦┘ä ž╣┘ä┘ē ž¬ž¼┘ģ┘Ŗž╣ž® žŻž│ž”┘äž® ž¦┘äž©┘Ŗ┘łHER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...



HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...PVI, PeerView Institute for Medical Education
╠²
Chair and Presenters Sara A. Hurvitz, MD, FACP, Carey K. Anders, MD, FASCO, and Vyshak Venur, MD, discuss metastatic HER2-positive breast cancer in this CME/NCPD/CPE/AAPA/IPCE activity titled ŌĆ£Fine-Tuning the Selection and Sequencing of HER2-Targeting Therapies in HER2-Positive MBC With and Without CNS Metastases: Expert Guidance on How to Individualize Therapy Based on Latest Evidence, Disease Features, Treatment Characteristics, and Patient Needs and Preferences.ŌĆØ For the full presentation, downloadable Practice Aids, and complete CME/NCPD/CPE/AAPA/IPCE information, and to apply for credit, please visit us at https://bit.ly/4f8sUs7. CME/NCPD/CPE/AAPA/IPCE credit will be available until March 2, 2026.Sudurpaschim logsewa aayog Medical Officer 8th Level Curriculum



Sudurpaschim logsewa aayog Medical Officer 8th Level CurriculumDr Ovels
╠²
Sudurpaschim province psc ( lok sewa aayog) medical officer 8th level syllabusMORPHOLOGICAL FEATURES OF PNEUMONIA.....



MORPHOLOGICAL FEATURES OF PNEUMONIA.....maheenmazhar021
╠²
This presentation provides a detailed exploration of the morphological and microscopic features of pneumonia, covering its histopathology, classification, and clinical significance. Designed for medical students, pathologists, and healthcare professionals, this lecture differentiates bacterial vs. viral pneumonia, explains lobar, bronchopneumonia, and interstitial pneumonia, and discusses diagnostic imaging patterns.
¤ÆĪ Key Topics Covered:
Ō£ģ Normal lung histology vs. pneumonia-affected lung
Ō£ģ Morphological changes in lobar, bronchopneumonia, and interstitial pneumonia
Ō£ģ Microscopic features: Fibroblastic plugs, alveolar septal thickening, inflammatory cell infiltration
Ō£ģ Stages of lobar pneumonia: Congestion, Red hepatization, Gray hepatization, Resolution
Ō£ģ Common causative pathogens (Streptococcus pneumoniae, Klebsiella pneumoniae, Mycoplasma, etc.)
Ō£ģ Clinical case study with diagnostic approach and differentials
¤ö¼ Who Should Watch?
This is an essential resource for medical students, pathology trainees, and respiratory health professionals looking to enhance their understanding of pneumoniaŌĆÖs morphological aspects.Presentaci├│ "Projecte Benestar". MWC 2025



Presentaci├│ "Projecte Benestar". MWC 2025Badalona Serveis Assistencials
╠²
Presentaci├│ que va acompanyar la demostraci├│ pr├Āctica de metge d'Innovaci├│ Jos├® Ferrer sobre el projecte Benestar de BSA, nom d'IDIAP Pere Gol, el 5 de mar├¦ de 2025 a l'estand de XarSMART al Mobible Word Congress. IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINE



IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINERelianceNwosu
╠²
This presentation emphasizes the role of immunodiagnostics and Immunotherapy. MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
╠²
The course covers the steps undertaken from tissue collection, reception, fixation,
sectioning, tissue processing and staining. It covers all the general and special
techniques in histo/cytology laboratory. This course will provide the student with the
basic knowledge of the theory and practical aspect in the diagnosis of tumour cells
and non-malignant conditions in body tissues and for cytology focusing on
gynaecological and non-gynaecological samples.ISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...



ISPE Baseline PEG Volumen 7 Risk-Based Manufacture Pharmaceutical Products 2n...alokksharma18
╠²
guidelines for pharma productsBiography of Dr. Vincenzo Giordano



Biography of Dr. Vincenzo GiordanoDr. Vincenzo Giordano
╠²
Dr. Vincenzo Giordano began his medical career 2011 at Aberdeen Royal Infirmary in the Department of Cardiothoracic Surgery. Here, he performed complex adult cardiothoracic surgical procedures, significantly enhancing his proficiency in patient critical care, as evidenced by his FCCS certification.Non-Invasive ICP Monitoring for Neurosurgeons



Non-Invasive ICP Monitoring for NeurosurgeonsDhaval Shukla
╠²
This presentation delves into the latest advancements in non-invasive intracranial pressure (ICP) monitoring techniques, specifically tailored for neurosurgeons. It covers the importance of ICP monitoring in clinical practice, explores various non-invasive methods, and discusses their accuracy, reliability, and clinical applications. Attendees will gain insights into the benefits of non-invasive approaches over traditional invasive methods, including reduced risk of complications and improved patient outcomes. This comprehensive overview is designed to enhance the knowledge and skills of neurosurgeons in managing patients with neurological conditions.
Invasive systems are commonly used for monitoring intracranial pressure (ICP) in traumatic brain injury (TBI) and are considered the gold standard. The availability of invasive ICP monitoring is heterogeneous, and in low- and middle-income settings, these systems are not routinely employed due to high cost or limited accessibility. The aim of this presentation is to develop recommendations to guide monitoring and ICP-driven therapies in TBI using non-invasive ICP (nICP) systems.
HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...



HER2-Targeting Therapy in HER2+ MBC With and Without CNS Metastases: Selectio...PVI, PeerView Institute for Medical Education
╠²
MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdf



MLS 208 - UNIT 4 A - Tissue Processing - ETANDO AYUK - SANU 1 - Secured.pdfEswatini Medical Christian University - EMCU / Southern Nazarene University - SANU
╠²
FOLIC ACID DEFICIENCY I N CLINICAL PRACTICEpptx
- 1. FOLIC ACID DEFICIENCY Dr G VENKATA RAMANA MBBS DNB FAMILY MEDICINE
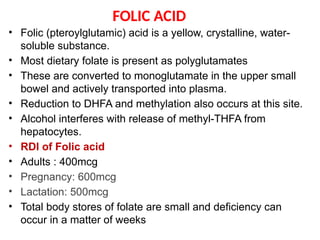
- 2. FOLIC ACID ŌĆó Folic (pteroylglutamic) acid is a yellow, crystalline, water- soluble substance. ŌĆó Most dietary folate is present as polyglutamates ŌĆó These are converted to monoglutamate in the upper small bowel and actively transported into plasma. ŌĆó Reduction to DHFA and methylation also occurs at this site. ŌĆó Alcohol interferes with release of methyl-THFA from hepatocytes. ŌĆó RDI of Folic acid ŌĆó Adults : 400mcg ŌĆó Pregnancy: 600mcg ŌĆó Lactation: 500mcg ŌĆó Total body stores of folate are small and deficiency can occur in a matter of weeks
- 5. Physiologic roles of folic acid ŌĆó DNA synthesis, RNA synthesis, DNA methylation ŌĆó Folic acid play a critical role in DNA and RNA synthesis ŌĆó Folic acid deficiency can therefore impair DNA synthesis, which in turn can cause a cell to arrest in the DNA synthesis (S) phase of the cell cycle, make DNA replication errors, and/or undergo apoptotic death ŌĆó Hematopoiesis ŌĆó Hematopoietic precursor cells are among the most rapidly dividing cells in the body and hence are one of the cell types most sensitive to abnormal DNA synthesis
- 6. ŌĆó Two major effects of the deficiency on hematopoiesis ŌĆó Megaloblastic changes ŌĆó caused by slowing of the nuclear division cycle relative to the cytoplasmic maturation cycle (ie, nuclear- cytoplasmic dyssynchrony). ŌĆó Ineffective erythropoiesis ŌĆó occurs when there is premature death (eg, phagocytosis or apoptosis) of the developing erythropoietic precursor cells in the bone marrow . ŌĆó There may be hypercellularity of the bone marrow ŌĆó laboratory findings of hemolysis, including elevated serum iron, indirect bilirubin, and lactate dehydrogenase (LDH), and low haptoglobin. ŌĆó The reticulocyte count is typically low
- 11. Clinical presentation ŌĆó Macrocytic anemia ŌĆó Symptoms of anemia-fatigue, irritability, cognitive decline,chest pain, shortness of breath,palpitations,light- headedness ŌĆó Yellowed skin ŌĆó Gastrointestinal symptoms ŌĆó Oral ulcers ŌĆó Glossitis ŌĆó Neuropsychiatric changes ŌĆó Depression, irritability, or forgetfulness ŌĆó Neural tube defects ŌĆó Spina bifida
- 12. lnvestigations ŌĆó CBC and blood smear ŌĆó Anemia ŌĆó Macrocytic red blood cells (MCV >100 fL) or macro- ovalocytosis ŌĆó An MCV value >115 fL is more specific to vitamin B12 or folate deficiency ŌĆó Mild leukopenia and/or thrombocytopenia ŌĆó Low reticulocyte count ŌĆó Hypersegmented neutrophils on the peripheral blood smear (ie, >5 percent of neutrophils with Ōēź5 lobes or Ōēź1 percent of neutrophils with Ōēź6 lobes) ŌĆó Increased lactate dehydrogenase ŌĆó Increased bilirubin
- 13. Peripheral smear and Bone marrow Peripheral blood smear showing a hypersegmented neutrophil (seven lobes) and macroovalocytes, a pattern that can be seen with vitamin B12 (cobalamin) or folate deficiency Erythroid precursors in the bone marrow (Left panel) Normal erythropoiesis. (Right panel) Megaloblastic erythropoiesis
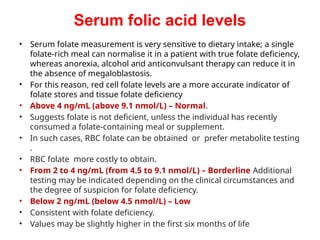
- 14. Serum folic acid levels ŌĆó Serum folate measurement is very sensitive to dietary intake; a single folate-rich meal can normalise it in a patient with true folate deficiency, whereas anorexia, alcohol and anticonvulsant therapy can reduce it in the absence of megaloblastosis. ŌĆó For this reason, red cell folate levels are a more accurate indicator of folate stores and tissue folate deficiency ŌĆó Above 4 ng/mL (above 9.1 nmol/L) ŌĆō Normal. ŌĆó Suggests folate is not deficient, unless the individual has recently consumed a folate-containing meal or supplement. ŌĆó In such cases, RBC folate can be obtained or prefer metabolite testing . ŌĆó RBC folate more costly to obtain. ŌĆó From 2 to 4 ng/mL (from 4.5 to 9.1 nmol/L) ŌĆō Borderline Additional testing may be indicated depending on the clinical circumstances and the degree of suspicion for folate deficiency. ŌĆó Below 2 ng/mL (below 4.5 nmol/L) ŌĆō Low ŌĆó Consistent with folate deficiency. ŌĆó Values may be slightly higher in the first six months of life
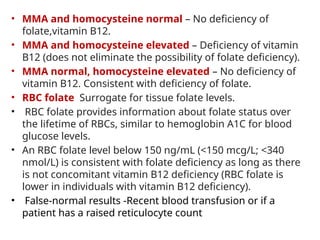
- 15. ŌĆó MMA and homocysteine normal ŌĆō No deficiency of folate,vitamin B12. ŌĆó MMA and homocysteine elevated ŌĆō Deficiency of vitamin B12 (does not eliminate the possibility of folate deficiency). ŌĆó MMA normal, homocysteine elevated ŌĆō No deficiency of vitamin B12. Consistent with deficiency of folate. ŌĆó RBC folate Surrogate for tissue folate levels. ŌĆó RBC folate provides information about folate status over the lifetime of RBCs, similar to hemoglobin A1C for blood glucose levels. ŌĆó An RBC folate level below 150 ng/mL (<150 mcg/L; <340 nmol/L) is consistent with folate deficiency as long as there is not concomitant vitamin B12 deficiency (RBC folate is lower in individuals with vitamin B12 deficiency). ŌĆó False-normal results -Recent blood transfusion or if a patient has a raised reticulocyte count
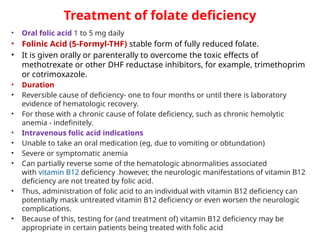
- 16. Treatment of folate deficiency ŌĆó Oral folic acid 1 to 5 mg daily ŌĆó Folinic Acid (5-Formyl-THF) stable form of fully reduced folate. ŌĆó It is given orally or parenterally to overcome the toxic effects of methotrexate or other DHF reductase inhibitors, for example, trimethoprim or cotrimoxazole. ŌĆó Duration ŌĆó Reversible cause of deficiency- one to four months or until there is laboratory evidence of hematologic recovery. ŌĆó For those with a chronic cause of folate deficiency, such as chronic hemolytic anemia - indefinitely. ŌĆó Intravenous folic acid indications ŌĆó Unable to take an oral medication (eg, due to vomiting or obtundation) ŌĆó Severe or symptomatic anemia ŌĆó Can partially reverse some of the hematologic abnormalities associated with vitamin B12 deficiency .however, the neurologic manifestations of vitamin B12 deficiency are not treated by folic acid. ŌĆó Thus, administration of folic acid to an individual with vitamin B12 deficiency can potentially mask untreated vitamin B12 deficiency or even worsen the neurologic complications. ŌĆó Because of this, testing for (and treatment of) vitamin B12 deficiency may be appropriate in certain patients being treated with folic acid
- 17. ŌĆó Adverse effects ŌĆó Oral folic acid is entirely nontoxic ŌĆó Injections rarely cause sensitivity reactions ŌĆó Prevention of folate deficiency ŌĆó Enrich cereals and grain products with folic acid to reduce the risk of neural tube defects ŌĆó Folic acid prophylaxis ŌĆó Typical dose, 1 mg orally per day ŌĆó All women,from the moment they begin trying to conceive until 12 weeks of gestation to prevent neural tube defects ŌĆó Hemolytic anemias/hyperproliferative hematologic states ŌĆó Patients with rheumatoid arthritis or psoriasis on methotrexate ŌĆó Patients on antiepileptic drugs ŌĆó Patients with ulcerative colitis

















