Formation of Urine.pptx mechanism of formation
- 2. Urine • Urine, a typically sterile liquid by-product of the body, is secreted by the kidneys through a process called urination and excreted through the urethra. • The normal chemical composition of urine is mainly water content, but it also includes nitrogenous molecules, such as urea, as well as creatinine and other metabolic waste components. • Other substances may be excreted in urine due to injury or infection of the glomeruli of the kidneys, which can alter the ability of the nephron to reabsorb or filter the different components of blood plasma. • Urine is often used as a diagnostic feature for many disease conditions. These may be based on either physical or chemical components, that may give insight to processes within the body, often through urinalysis, a common clinical analysis of urine. • Physical Characteristics • Physical characteristics that can be applied to urine include color, turbidity (transparency), smell (odor), pH (acidity – alkalinity) and density. Many of these characteristics are notable and identifiable by by vision alone, but some require laboratory testing. • Color: Typically yellow-amber, but varies according to recent diet and the concentration of the urine. Drinking more water generally tends to reduce the concentration of urine, and therefore causes it to have a lighter color. Dark urine may indicate dehydration. Red urine indicates red blood cells within the urine, a sign of kidney damage and disease.
- 3. • Smell: The smell of urine may provide health information. For example, urine of diabetics may have a sweet or fruity odor due to the presence of ketones (organic molecules of a particular structure) or glucose. Generally fresh urine has a mild smell but aged urine has a stronger odor similar to that of ammonia. • The pH of normal urine is generally in the range 4.6 – 8, with a typical average being around 6.0. Much of the variation occurs due to diet. For example, high protein diets result in more acidic urine, but vegetarian diets generally result in more alkaline urine (both within the typical range of 4.6 – 8). • Density: Density is also known as “specific gravity.” This is the ratio of the weight of a volume of a substance compared with the weight of the same volume of distilled water. The density of normal urine ranges from 0.001 to 0.035. • Turbidity: The turbidity of the urine sample is gauged subjectively and reported as clear, slightly cloudy, cloudy, opaque or flocculent. Normally, fresh urine is either clear or very slightly cloudy. Excess turbidity results from the presence of suspended particles in the urine, the cause of which can usually be determined by the results of the microscopic urine sediment examination. Common causes of abnormal turbidity include: increased cells, urinary tract infections or obstructions.
- 5. • Chemical Composition of Urine • Normal urine consists of water, urea, salts, and pigments. • Urine is an aqueous solution of greater than 95% water, with a minimum of these remaining constituents, in order of decreasing concentration: • Urea 9.3 g/L. • Chloride 1.87 g/L. • Sodium 1.17 g/L. • Potassium 0.750 g/L. • Creatinine 0.670 g/L. • Other dissolved ions, inorganic and organic compounds ( metabolites).
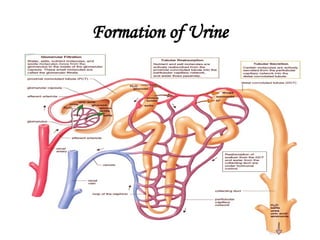
- 6. Formation of Urine • There are three stages involved in the process of urine formation. They are- 1. Glomerular filtration or ultra- filtration 2. Tubular Reabsorption 3. Tubular Secretion
- 8. Glomerular Filtration • This takes place through the semipermeable walls of the glomerular capillaries and Bowman’s capsule. • The afferent arterioles supplying blood to glomerular capsule carries useful as well as harmful substances. The useful substances are glucose, aminoacids, vitamins, hormones, electrolytes, ions etc and the harmful substances are metabolic wastes such as urea, uric acids, creatinine, ions, etc. • The diameter of efferent arterioles is narrower than afferent arterioles. Due to this difference in diameter of arteries, blood leaving the glomerulus creates the pressure known as hydrostatic pressure. • The glomerular hydrostatic pressure forces the blood to leaves the glomerulus resulting in filtration of blood. A capillary hydrostatic pressure of about 7.3 kPa (55 mmHg) builds up in the glomerulus. However this pressure is opposed by the osmotic pressure of the blood, provided mainly by plasma proteins, about 4 kPa (30 mmHg), and by filtrate hydrostatic pressure of about 2 kPa (15 mmHg in the glomerular capsule. • The net filtration pressure is, • Therefore: 55-(30 +15) = 10mmHg.
- 12. • By the net filtration pressure of 10mmHg, blood is filtered in the glomerular capsule. • Water and other small molecules readily pass through the filtration slits but Blood cells, plasma proteins and other large molecules are too large to filter through and therefore remain in the capillaries. • The filtrate containing large amount of water, glucose, aminoacids, uric acid, urea, electrolytes etc in the glomerular capsule is known as nephric filtrate of glomerular filtrate. • The volume of filtrate formed by both kidneys each minute is called the glomerular filtration rate (GFR). In a healthy adult the GFR is about 125 mL/min, i.e. 180 litres of filtrate are formed each day by the two kidneys
- 13. Tubular Reabsorption • As the filtrate passes to the renal tubules, useful substances including some water, electrolytes and organic nutrients such as glucose, aminoacids, vitamins hormones etc are selectively reabsorbed from the filtrate back into the blood in the proximal convoluted tubule. • Reabsorption of some substance is passive, while some substances are actively transported. Major portion of water is reabsorbed by Osmosis. • Only 60–70% of filtrate reaches the Henle loop. Much of this, especially water, sodium and chloride, is reabsorbed in the loop, so that only 15–20% of the original filtrate reaches the distal convoluted tubule, More electrolytes are reabsorbed here, especially sodium, so the filtrate entering the collecting ducts is actually quite dilute. • The main function of the collecting ducts is to reabsorb as much water as the body needs. • Nutrients such as glucose, amino acids, and vitamins are reabsorbed by active transport. Positive charged ions ions are also reabsorbed by active transport while negative charged ions are reabsorbed most often by passive transport. Water is reabsorbed by osmosis, and small proteins are reabsorbed by pinocytosis.
- 16. Tubular Secretion • Tubular secretion takes place from the blood in the peritubular capillaries to the filtrate in the renal tubules and can ensure that wastes such as creatinine or excess H+ or excess K+ ions are actively secreted into the filtrate to be excreted. • Excess K+ ion is secreted in the tubules and in exchange Na+ ion is reabsorbed otherwise it causes a clinical condition called Hyperkalemia. • Tubular secretion of hydrogen ions (H+) is very important in maintaining normal blood pH. • Substances such as , e.g. drugs including penicillin and aspirin, may not be entirely filtered out of the blood because of the short time it remains in the glomerulus. Such substances are cleared by secretion from the peritubular capillaries into the filtrate within the convoluted tubules. • The tubular filtrate is finally known as urine. Human urine is usually hypertonic.
- 19. Micturition • The process of time to time collection and removal of urine from urinary bladder is known as micturition. Collection of more than 300ml of urine in urinary bladder creates pressure on the wall. The pressure stimulates the desire for urination.
- 22. Thank you !!!!