Fungal Infections of Skin, Soft tissue.pptx
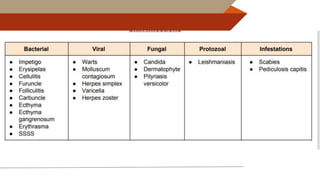
- 2. 2
- 3. Introduction Ō¢░ Affect: skin, nail & hair Ō¢░ Mild & chronic infections Ō¢░ Fungi specialized saprophytes: digest keratin Ō¢░ Three types of infections: Ō¢╗ Surface infection: dead layer of skin- tinea Ō¢╗ Cutaneous infection: cornified layer of skin, dermatophytes Ō¢╗ Subcutaneous infections- mycetoma, rhinosporidiosis 3
- 4. 4
- 5. Surface infection Ō¢╗ Dead layer of skin Ō¢╗ No inflammatory response Ō¢╗ Cosmetic effects Ō¢╗ Eg. Tinea versicolor, Tinea nigra & Piedra. Cutaneous infection: Dermatophytosis/ tinea/ ringworm ’é× cornified layer of skin, hair, nail ’é× Inflammatory & allergic response ’é× Candidiasis 5
- 6. Tinea Versicolor 6 Ō¢░ Tinea versicolor (or pityriasis versicolor) ŌĆō chronic recurrent condition involving the superficial layer (stratum corneum) of skin. Ō¢░ Caused by a lipophilic fungus Malassezia furfur.
- 7. Clinical Manifestations 7 Ō¢░ Characterized by flat-round scaly patches of hypo- to hyperpigmentation of skin. Ō¢░ Lesions - non-inflammatory and non-pruritic Ō¢░ Areas rich in sebaceous glands - commonly involved - neck, chest, or upper arms Ō¢░ Disease is more common in moist humid areas. A B
- 8. ’é× Localized infection of stratum corneum ’é× Painless brown or black macular lesions- hands ŌĆó Causative agent: ŌĆó Hortaea wernickii (Exophiala werneckii), black coloured fungus
- 9. ŌĆó Infection of hair ŌĆó Characterized by firm, irregular nodules along the hair shaft ŌĆó Black piedra ŌĆō Piedraia hortae ŌĆó White piedra ŌĆō Trichosporon beigelii
- 10. Laboratory Diagnosis 10 Ō¢░ Direct microscopy: Skin scrapings examined - after treating with 10% KOH. Ō¢░ Mixture of budding yeasts and short septate hyphae ŌĆō seen -spaghetti and meatballs appearance- Malassezia furfur.
- 11. Laboratory Diagnosis (Cont..) 11 Ō¢░ Culture: SDA with olive oil overlay - ŌĆśfried eggŌĆÖ colonies- Malassezia furfur appear after incubating for 5ŌĆō7 days at 32ŌĆō35┬░C Ō¢░ Urease test: positive Ō¢░ WoodŌĆÖs lamp examination: golden yellow fluorescence. Ō¢░ White Piedra- : Trichosporon beigelii, yeast like fungus, arthrospores Ō¢░ Black Piedra- Piedraia hortae- Phaeoid fungus
- 12. Dermatophytoses 12 Ō¢░ Dermatophytoses (or tinea or ringworm) - most common superficial mycoses affecting skin, hair and nail- infecting keratinized tissues- inflammatory & HST reaction Ō¢░ Classification ’āś Trichophyton species: Infect skin, hair and nail ’āś Microsporum species: Infect skin and hair ’āś Epidermophyton species: Infect skin and nail
- 13. Pathogenesis 13 Ō¢░ Acquired by direct contact with soil, animals or humans infected with fungal spores Ō¢░ Predisposing factors - moist humid skin and tight ill-fitting underclothing Ō¢░ Fungal products: local inflammation Ō¢░ Hypersensitivity to fungal antigens Ō¢░ Severity depends on the infecting fungi, immune status of the host and the site of lesion
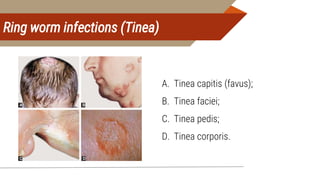
- 15. Ring worm infections (Tinea) 15 A B C D A. Tinea capitis (favus); B. Tinea faciei; C. Tinea pedis; D. Tinea corporis.
- 16. TENIA CAPITIS Favus: dense crusts (scutula) develop in the hair follicles ŌĆō leads to alopecia & scarring Kerioon: boggy lesions with marked inflammatory reactions
- 19. DISEASE COMMON CAUSATIVE AGENTS Tinea capitis Microsporum any spp., trichophyton most spp. Favus T.schoenleinii, T. violaceum, M. gypseum Tinea barbae T. rubrum, T. mentagrophytes, T. verrucosum Tinea imbricata T. concentricum Tinea corporis T. rubrum & any other dermatophyte Tinea cruris E. floccosum, T. rubrum Tinea pedis T. rubrum, E. floccosum Ectothrix hair infection Microsporum spp., T. rubrum, T. mentagrophytes Endothrix hair infection T.schoenleinii, T. tonsurans, T. violaceum
- 20. ŌĆó Sample collection ŌĆó Scraping from the edge of the lesions ŌĆó Infected hair to be plucked out ŌĆō ectothrix / endothrix ŌĆó Infected nail clippings ŌĆó KOH mount ŌĆó Culture on SDA with antibiotics & cycloheximide ŌĆō incubated at R.T. ŌĆó Growth slow ŌĆō 1-3 weeks
- 22. Laboratory Diagnosis 22 Woods Lamp Examination: Ō¢░ Positive for various Microsporum species &Trichophyton schoenleinii Ō¢░ Fluorescence is due to the presence of pteridine pigment in cell wall
- 23. Laboratory Diagnosis (Cont..) 23 Ō¢░ KOH mount or calcofluor white stain - thin septate hyaline hyphae with arthroconidia Ō¢░ Hair ŌĆō arthroconidia on the surface of shaft (ectothrix) or within the shaft (endothrix)
- 24. Laboratory Diagnosis (Cont..) 24 Ō¢░ Culture: Ō¢░ SDA containing cycloheximide - incubated at 26ŌĆō28┬░C for 4 weeks Ō¢░ Potato dextrose agar ŌĆō better sporulation Ō¢░ Identification is made by: ’āś Macroscopic appearance of the colonies - rate of growth, texture, pigmentation, colony topography
- 25. Macroconidia of various dermatophyte species 25 C D E C. Trichophyton mentagrophytes; D. Microsporum canis; E. Epidermophyton floccosum
- 26. Microscopic appearance of various dermatophyte species (LPCB mount) 26 A. Trichophyton mentagrophytes; B. Microsporum canis; C. Epidermophyton floccosum.
- 27. Special types of hyphae seen in dermatophytes 27 G H I
- 28. Laboratory Diagnosis (Cont..) 28 Ō¢░ Other Methods of Diagnosis: Ō¢░ Hair perforation test: ’āś Fungi pierce hair producing wedge-shaped perforations ’āś Positive ŌĆō T.mentagrophytes and M.canis Ō¢░ Urease test: Trichophyton mentagrophytes is urease positive
- 29. SUBCUTANEOUS MYCOSES 29 Ō¢░ The agents of subcutaneous mycoses usually inhabit the soil Ō¢░ They enter the skin by traumatic inoculation with contaminated material- thorn prick Ō¢░ Tend to produce granulomatous lesions in the subcutaneous tissue Ō¢░ Eg Mycetoma, rhinosporidiosis, sporotrichosis, chromoblastomycosis
- 30. SUBCUTANEOUS MYCOSES 30 Sprotrichosis- lymphocutaneous mycosis- Sprothrix schenckii- thermally dimorphic fungus
- 31. Mycetoma 31 Ō¢░ Chronic, slowly progressive granulomatous infection of the skin and subcutaneous tissues Ō¢░ Triad: Swelling, discharging sinuses and presence of granules in the discharge Ō¢░ Maduramycosis or Madura foot - first described in Madurai-John Gill (1842) Ō¢░ Eumycetoma ŌĆō caused by fungi Ō¢░ Actinomycetoma ŌĆō Caused by bacteria Ō¢░ Bacterial (botryomycosis)- Staphylococcus, Streptomyses
- 32. Clinical Manifestations 32 Ō¢░ Clinical triad 1. Tumor like swelling (tumefaction) 2. Discharging sinuses 3. Granules in sinuses Commonest site ŌĆō Feet (Hands, back) Ō¢░ Osteolytic or osteosclerotic bony lesions Ō¢░ Usually painless
- 33. Laboratory Diagnosis 33 Specimen Collection: Ō¢░ Grains/ Granules/ biopsy collected on sterile gauze by pressing the sinuses from periphery or by using a loop Direct Examination: Ō¢░ Granules washed in sterile saline; crushed between the slides and examined
- 34. Laboratory Diagnosis (Cont..) 34 Ō¢░ Macroscopic appearance of granules - color, size, shape, texture Ō¢░ Suspected Eumycetoma : ’āś KOH mount - hyphae of 2ŌĆō6 ╬╝m width along with chlamydospores at margin Ō¢░ Suspected Actinomycetoma: ’āś Gram staining - filamentous gram positive bacilli (0.5ŌĆō1 ╬╝m wide) ’āś Modified acid fast stain ŌĆō Nocardia is weekly acid fast
- 35. Laboratory Diagnosis (Cont..) 35 Ō¢░ Histopathological staining and KOH of the granules: A B
- 36. Laboratory Diagnosis (Cont..) 36 Culture: Ō¢░ Granules - best specimen for culture Ō¢░ Both fungal (SDA) and bacteriological media (Lowenstein Jensen medium, Blood agar) - inoculated Ō¢░ Eumycetoma agents - growth rate, colony morphology, production of conidia and their sugar assimilation patterns
- 37. Other Subcutaneous Mycoses Ō¢░ Sporotrichosis- Lymhocutaneous Ō¢░ Chrmoblastomycosis- slow growing and polymorphic - verrucose (most common type), crusted, ulcerative and nodular or tumor-like lesions, Caused by darkly pigmented fungi- that produce a characteristic morphology called sclerotic body- Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii Ō¢░ Rhinosporidiosis- rhinosporidium seeberi- Ō¢░ now considered protista- not cultivable 37
- 38. Laboratory Diagnosis (Cont..) 38 Ō¢░ Microscopy- Ō¢░ Asteroid body - central basophilic yeast cell surrounded by radiating extensions of eosinophilic mass, composed of antigen-antibody complexes- sporotrichosis, also observed in zygomycosis, candidiasis, aspergillosis and blastomycosis Ō¢░ Sclerotic bodies: brown thick walled round cells (5ŌĆō12 ╬╝m size) with multiple internal transverse septa - also called Medlar bodies or muriform cells or ŌĆ£copper pennies.ŌĆØ- Chromoblastomycosis
- 39. Laboratory Diagnosis (Cont..) 39 Ō¢░ Culture: Definitive tool for diagnosis. Ō¢░ Specimens - inoculated onto SDA and blood agar in duplicate - incubated at 25┬░C and 37┬░C simultaneously - S. schenckii is a dimorphic fungus ’āś At 25┬░C: Produces mycelial form - slender delicate hyphae with conidia arranged in - flower-like pattern. ’āś At 37┬░C: Produces yeast form - moist creamy white colonies which turn brown black in 10ŌĆō14 days. A B
- 40. OPPORTUNISTIC MYCOSES OF SKIN 40 Ō¢░ Penicillium marneffei - thermally dimorphic fungus, Renamed as - Talaromyces marneffei Ō¢░ Causes opportunistic infection in HIV-infected patients. Ō¢░ Skin lesions: Warty lesions mimicking that of molluscum contagiosum Ō¢░ Lab Diagnosis- Histopathological staining- oval or elliptical yeast cells with central septation Ō¢░ Culture on SDA- black pigment
- 41. Candidiasis 41 Ō¢░ Candida species are the most common fungal agent to cause lesions of skin and mucosa. Ō¢░ Oropharyngeal candidiasis : white, adherent, painless patch Ō¢░ Vulvovaginitis: pruritus, pain, and vaginal discharge (whitish curd like in severe cases) Ō¢░ Balanitis and balanoposthitis Ō¢░ Esophageal candidiasis