gastroprotective role of nitric oxide
- 1. GASTROPROTECTION: THE ROLE OF NITRIC OXIDE OWONIKOKO, W. MATHEW PHYSIOLOGY DEPARTMENT, IGBINEDION UNIVERSITY OKADA, EDO STATE. (owonikoko.mathew@yahoo.com) 1
- 2. OUTLINEOUTLINE ’éŚThe functional anatomy of the stomach ’éŚGastric defence mechanisms ’éŚMechanisms of gastropathy ’éŚGastric physiological condition ’éŚGastric pathological condition ’éŚNitric Oxide (NO) ’éŚNO in physiological gastroprotection ’éŚNO in healing processes ’éŚConclusion 2
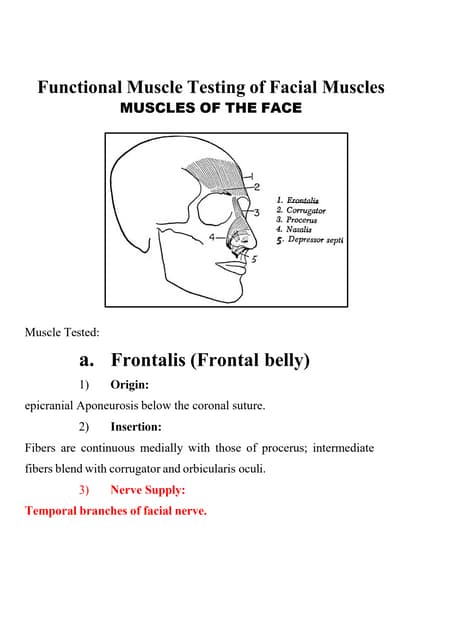
- 3. THE STOMACHTHE STOMACH Located in the upper left quadrant of the abdominal cavity to the left of the liver and in front of the spleen, the stomach has the following functions, namely; ’āśStorage ’āśDigestion ’āśMix the stomachŌĆÖs content ’āśInhibit bacterial growth ’āśProvide intrinsic factor for Vitamin B12 absorption ’āśRegulate the rate of emptying to the small intestine Constant exposure of the stomach to detrimental agents in foods and other substances predisposes the stomach to gastropathies. William, 2009 3
- 4. GASTRIC MUCOSA ENVIRONMENTGASTRIC MUCOSA ENVIRONMENT Laine et al, 2008 4
- 5. BICARBONATE-RICH MUCOUS FROM SURFACE EPITHELIAL CELLBICARBONATE-RICH MUCOUS FROM SURFACE EPITHELIAL CELL Silva and Sousa, 2011 5
- 6. GASTROPATHYGASTROPATHY ŌĆó Gastropathies e.g. peptic ulcer is a deep defect in the gastric wall penetrating the entire mucosal thickness and the muscularis mucosa (Tarnawski, 2000). ŌĆó ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł ’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł’üł 6
- 7. STOMACH IN HEALTH ANDSTOMACH IN HEALTH AND DISEASEDISEASE Silva and Sousa, 2011 7
- 8. HelicobacterHelicobacter pyloripylori AND ULCERAND ULCER FORMATIONFORMATION Silva and Sousa, 2011 8
- 9. MECHANISM OF NSAIDs-INDUCED DAMAGEMECHANISM OF NSAIDs-INDUCED DAMAGE Wallace, 2008.9
- 10. NITRIC OXIDENITRIC OXIDE First gas known to act as a biological messenger; it serves different functions depending on body system. i.e. neurotransmitter, vasodilator, bactericide. Nitric oxide is a diatomic free radical consisting of one atom of nitrogen and one atom of oxygen. Its one of the smallest molecules in nature and the natural form is a gas NO can be transported to the target cell due to its following features ’éŚ It is small, lipid-soluble, uncharged and the half life is less than 30sec in living systems, hence capable of diffusing through the cellmembrane ’éŚ It interact with thiol groups forming Nitrosothiols (SNO) (Nitin et al, 2011). N O 10
- 11. SOURCES OF NITRIC OXIDESOURCES OF NITRIC OXIDE 1. NO can be produced from L-arginine by NOS (Nitin et al, 2011) 2. Also dietary nitrate is reduced in the oral cavity to nitrite by bacterial reductase (Duncan et al, 1995) yielding NO after acidification in gastric lumen (McKnight et al, 1997) 3. NO can as well be produced from nitrite and nitrate during hypoxic condition by Xanthine oxidoreductase enzyme. 4. H2O2 react with arginine producing NO (Nagase et al, 1997) 5. NO is produced in the colon by anaerobic bacteria (Brittain et al, 1992). 1,2 and 3 above are enzyme dependent while 3 and 4 are non-enzyme dependent. COO- C (CH2)3 NH C H2N H NH2+ +H3N Arginine NOS NADPH + O2 NAD+ COO- C (CH2)3 NH C H+H3N N + H2N H OH N-w-Hydroxyarginine COO- C (CH2)3 NH H+H3N + NO NOS C O NH2 Citrulline 11
- 12. REACTION AND CATALYSIS OF NOSREACTION AND CATALYSIS OF NOS Alderton et al, 2001 12
- 13. TYPES OF NOSTYPES OF NOS Alderton et al, 2001 13
- 14. NITRIC OXIDE IN THE ACTNITRIC OXIDE IN THE ACT 14Wallace and Miller, 2000.
- 15. TARGETS FOR THE GASTROPROTECTIVE ROLE OF NO ON NSAID-TARGETS FOR THE GASTROPROTECTIVE ROLE OF NO ON NSAID- INDUCED GASTRIC DAMAGEINDUCED GASTRIC DAMAGE Mannick et al,1996. 15
- 16. ACTIONS OF NOACTIONS OF NO Kolios et al, 2004 16
- 17. NO IN MUCOSA BLOODFLOWNO IN MUCOSA BLOODFLOW Kolluru et al, 2012 17
- 18. ULCER HEALINGŌĆ£CONDIMENTSŌĆØULCER HEALINGŌĆ£CONDIMENTSŌĆØ Gastric Ulcer healing is an active andcomplicated process: ŌĆó Inflammation, granulation tissue formation, ŌĆó Tissue remodeling, Angiogenesis, ŌĆó Cell division, ŌĆó Fibroblast migration, ŌĆó Mucosal regeneration, ŌĆó Reconstruction of gastric glands, etc. (Tarnawski, 2000). Processes controlled by factors: ŌĆó TNF-alpha, COX-2, PGE2, ŌĆó Serum Response Factor (SRF), ŌĆó Nitric Oxide (NO), Angiopoietins, ŌĆó Endothelin, Metalloproteinases, ŌĆó Transcription factors, Cytokines, etc. (Schmassmann, 2005). 18
- 19. MOLECULAR UPREGULATIONS IN WOUND HEALING PROCESSESMOLECULAR UPREGULATIONS IN WOUND HEALING PROCESSES Gould et al, 2008 19
- 20. ULCER HEALING PROCESSESULCER HEALING PROCESSES Fornai et al, 2011 20
- 21. NITRIC OXIDE AND WOUNDNITRIC OXIDE AND WOUND HEALINGHEALING Luo and Chen, 2005 21
- 22. RECOMMENDATION AND CONCLUSIONRECOMMENDATION AND CONCLUSION ’āśNSAIDs and H. pylori are capable of enormous erosion of gastro-protective agents and should best be avoided. ’āśThe mechanism of NO protection in normal gastric conditions include mucus, acid, bicarbonate and prostaglandins secretion, while re-epithelialization, tissue remodelling, angiogenesis etc which are the major processes involved in gastric injury healing remains the same target for NO gastro-protections. ’āśHence, clinical development of NO-NSAIDs has newly been introduced but still has to be completed before its potentials in human can be fully validated; even though the available pre-clinical and clinical data are encouraging. 22
- 23. REFERENCESREFERENCES ’éŚ Laine L., et al. (2008). Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology, Vol.135, No.1, (July 2008), pp.41-60 ’éŚ Tarnawski, 2000 ’éŚ Schmassmann, 2005 ’éŚ Kolluru et al, 2012.Endothelial Dysfunction and Diabetes: Effects on Angiogenesis, Vascular Remodeling, andWound Healing, International Journal of Vascular Medicine ’éŚ Wallace, 2009. Cyclooxygenase-inhibiting nitric oxide donators for osteoarthritis; Trends in Pharmacological Sciences Vol.30 No.3 ’éŚ Luo and Chen, 2005. Nitric oxide: a newly discovered function on wound healing. Acta pharmacologica sinica; 26 (3), pg 259-264. ’éŚ Nitin et al, 2011. Nitric oxide and the gastrointestinal tract. International journal of pharmacology; 7 (1) pg 31-39. ’éŚ Wallace JL, Miller MJS, 2000: Nitric oxide in mucosal defence. A little goes a long way. Gastroenterology, vol. 119 pg 512-520 ’éŚ Duncan et al, 1995. chemical generation of nitric oxide in the mouth from the enterosalivary circulation of dietary nitrate. Nat. Med., 1: 546-551 23
- 24. REFERENCESREFERENCES ’éŚ McKnight et al, 1997. chemical synthesis of nitric oxide in the stomach from dietary nitrate in humans. Gut, 40: 211-214. ’éŚ Nagase et al, 1997. A novel nonenzymatic pathway for the generation of nitric oxide by the reaction of hydrogen peroxide and D- or L-arginine. Biochem. Biophys. Res. Commun., 233: 150-153. ’éŚ Brittain et al, 1992. Bacterial nitrite-reducing enzymes. Eur. J. biochem., 209: 793-802 ’éŚ Gould et al, 2008. Arginine metabolism and wound healing Wound. Healing Southern Africa;1(1):48-50. ’éŚ Alderton et al, 2001. Nitric oxide synthases : structure, function and inhibition. Biochem. J. 357, 593┬▒615 ’éŚ Kolios et al, 2004. Nitric oxide in inflammatory bowel disease: a universal messenger in an unsolved puzzle. Immunology vol 113 427ŌĆō 437 ’éŚ Matteo Fornai, Luca Antonioli, Rocchina Colucci, Marco Tuccori and Corrado Blandizzi (2011). Pathophysiology of Gastric Ulcer Development and Healing: Molecular Mechanisms and Novel Therapeutic Options, Peptic Ulcer Disease, Dr. Jianyuan Chai (Ed.), ISBN: 978-953-307-976-9 24
Editor's Notes
- #9: Gastric ulcer formatted by Helicobacter pylori. (1) H. pylori catalyzes urea hydrolysis with the formation of ammonium (NH3) that neutralizes the surrounding gastric acid and protects itself from the strong acidicity of the stomach. (2) H. pylori penetrates the mucus layer of stomach, adhere the surface of gastric mucosal epithelial cells, proliferate and finally form the infectious focus. The gastric lesion is developed by destruction of mucosa. Inflammation, mucosal cell death, PUD, DUODENAL ULCER, GASTRIC CANCER AND COLORECTAL CARCINOMA. (ADENIYI, MAY 2013)ITLED ŌĆ£MICROBES: CULPRIT AND THEIR ATTACKERS ON NATUREŌĆÖS FIELDŌĆØ
- #12: (NOS; a1,294 AA enzyme)
- #16: NSAIDs cause adhesion of circulating neutrophil and hence the latter clogs the microvasculature causing a local decrease in mucosal blood flow and a marked release of tissue damaging factor including proteolytic enzymes and luekotriene, which enhances vascular tone, exacerbate tissue ischeamia, stimulate the production of ROS, and promote the destruction of intestinal matrix, leading to a severe degree of focal tissue necrosis,particularly in the presence of a low luminal pH. Most NSAIDs converge on the COX-independent gastric mucosal injury path becos they are weakly acidic. Since they are protonophoric in nature, they penetrate cell membrane and accumulate into epithelial cells, where the inner pH is is at a physiological level of 7.4. At this level, they (e.g. aspirin) dissociate and remain segregated within cell. This accumulation enhances the inhibition of prostaglandin biosysnthesis, uncouple mitochondrial oxidative phosphorylation. The latter leads to decrease in ATP production and an increase in ADP and AMP levels, which are then responsible for increments of intracellular calcium concentration . These changes are followed by mitochondrial injury, increased generation of ROS and alterations in the Na+/ k+ balance which lead to weakening of the mucosal barrier and cellular necrosis (Wallace, 2001). NSAIDs also destroy the integrity of epithelial tight junction by down-regulating Claudin-7, a member of the claudin protein family, which play important roles in the formation of tight junctions. (Oshima et al., 2008).
- #18: Foam cells produce proinflammatory cytokines that are released into the lumen of blood vessel (far right). Increased ROS production through iNOS leads to increased ROS generation. Steps involved in leukocyte adhesion and migration (bottom left). Hyperglycemic effects on the blood vessel. Atherosclerotic plaque formation initiated through uptake of LDL from blood by endothelial cells. Foam cells produce proinflammatory cytokines that are released into the lumen of blood vessel (far right). Increased glucose leads to decreased L-arginine and BH4, which leads to decreased NO production in endothelial cells. All of these factors are proinflammatory and atherogenic.