Genu valgus
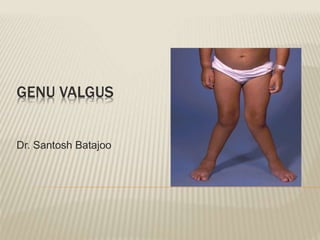
- 1. GENU VALGUS Dr. Santosh Batajoo
- 2. ï Genu valgum or knock knee ï Outward deviation of the longitudinal axis of tibia.
- 3. DEFORMITY ï Medial angulation of the knee and outward deviation of the longitudinal axis of both the tibia and the femur. ï Advanced cases- the distal ends of the femur and tibia are rotated externally by the pull of the biceps femoris and the tensor fascia lata. ï Distal shaft of the tibia develops a compensatory internal rotation ï Pronated and flat foot.
- 4. ï Idiopathic variety is the commonest. ï Bilateral ï Physiological genu valgum appears at the age of 2-3 years and nearly always corrects by the age of 6.
- 5. PATHOPHYSIOLOGY ï The mechanical axis shifts laterally, pathologic stress is placed on the lateral femur and tibia, inhibiting growth and possibly leading to vicious cycle.
- 6. ï Asymmetrical rate of growth of the epiphyseal plate- trauma, infection. ï Static abnormality like deformed femur or the tibia or muscle imbalance brings excessive pressure on one end of the plate. ï Metabolic and nutritional disturbance ï Malunion of fracture at the metaphysis ï Developmental disturbances â osteogenesis imperfecta, chondrodysplasia
- 7. ï The medial condyle assumes larger proportions, and the articular surfaces lie at an oblique angle. ï The quadriceps extensor mechanism crosses the joint over the lateral aspect where the patella tends to subluxate or dislocate outward. ï Soft tissue structures on the lateral side are shortened (biceps, iliotibial band, peroneal nerve) ï Medial collateral ligament is lax.
- 8. TYPES Physiological â Compensatory- ï Varus, valgus and rotational deformities of the proximal femur. ï Persistent anteversion of the femoral neck Pathological- ï Distorted epiphyseal or physeal growth. ï Rickets, injuries of the epiphyseal and physeal growth cartilage.
- 9. In adults- ï Common in females. ï May be sequel to childhood deformity, rheumatoid arthritis, ligament injury, malunited fractures, pagetâs disease. ï Complications- ï Patello-femoral osteoarthritis due to abnormal tracking of the patella.
- 10. CAUSES ïą Idiopathic ïą Post-traumatic fractures of the lateral femoral or tibial condyles damage to lateral lower femoral or upper tibial epiphyses. ïą Post inflammatory damage to lateral epiphyses by infection. ïą Neoplastic tumour causing growth disparity e.g. chondroblastoma
- 11. ïą Bone softening rickets and osteomalacia, bone dysplasias, RA ïą Stretching of joints charcotâs disease, paralytic disease ïą Cartilage thinning OA of the lateral compartment of the knee
- 12. CLINICAL FEATURES ï Knee pain ï Gait- limp or circumduction ï Deformity of the knee. ï Intermalleolar gap- distance between the medial malleoli when the knees are touching with the patella facing forwards, is more than 8cm.
- 13. ï Plumb line test. ï Knee flexion test to detect whether it lies in the femur or tibia.
- 14. RADIOGRAPHS X-ray ï Entire lower limb with the patient weight bearing ï Angle formed between femoral and tibial shafts (normal 6š)
- 15. ï Lateral distal femoral angle (normal - 84š) ï Proximal medial tibial angle (normal â 87š)
- 16. TREATMENT CONSERVATIVE- ï Depends on the cause. ï vitamin D and calcium supplements ï Weight loss ï Exercise
- 17. ï Pronation of the feet is corrected by elevating the inner border of the shoes ï Knock knee braces are worn continuously
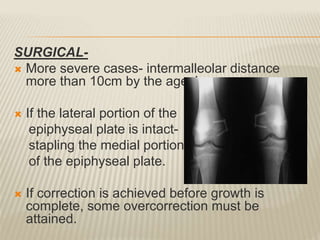
- 18. SURGICAL- ï More severe cases- intermalleolar distance more than 10cm by the age 4. ï If the lateral portion of the epiphyseal plate is intact- stapling the medial portion of the epiphyseal plate. ï If correction is achieved before growth is complete, some overcorrection must be attained.
- 19. Open wedge osteotomy- ï After epiphyseal fusion- an osteotomy at the site of maximum deformity, either femur or the tibia. ï If the length of the extremity is adequate, a wedge of bone is removed from the medial side. ï If the length is short, osteotomy from the outer side lengthens the extremity.
- 20. THANK YOUâĶ