Glaucoma Group F LMCTH 11th batch
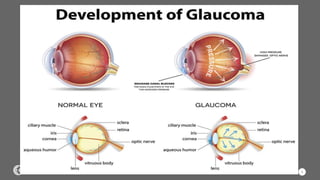
- 2. GLAUCOMA ’é¦ GLAUCOMA IS A DISEASE THAT CAUSES DAMAGE TO THE EYE. ’é¦ THIS DISEASE HAPPENS BECAUSE OF INCREASED PRESSURE IN THE EYE. THE PRESSURE CAUSES DAMAGE TO THE OPTIC NERVE.
- 3. 3
- 4. 4
- 5. 5
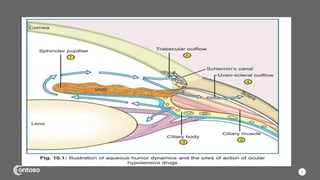
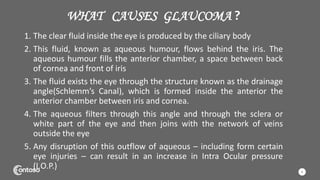
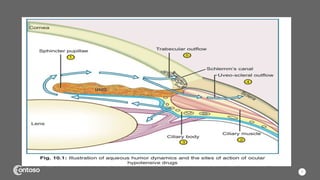
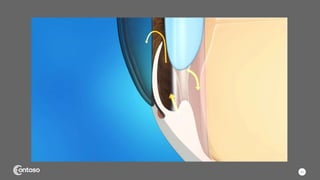
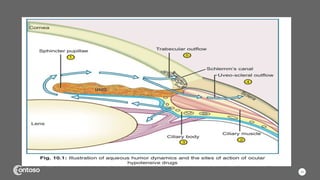
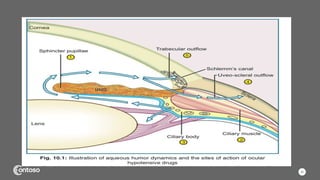
- 6. WHAT CAUSES GLAUCOMA ? 1. The clear fluid inside the eye is produced by the ciliary body 2. This fluid, known as aqueous humour, flows behind the iris. The aqueous humour fills the anterior chamber, a space between back of cornea and front of iris 3. The fluid exists the eye through the structure known as the drainage angle(SchlemmŌĆÖs Canal), which is formed inside the anterior the anterior chamber between iris and cornea. 4. The aqueous filters through this angle and through the sclera or white part of the eye and then joins with the network of veins outside the eye 5. Any disruption of this outflow of aqueous ŌĆō including form certain eye injuries ŌĆō can result in an increase in Intra Ocular pressure (I.O.P.) 6
- 7. 7
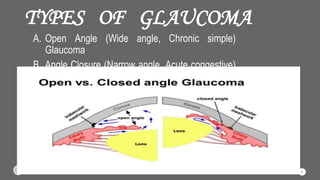
- 8. TYPES OF GLAUCOMA A. Open Angle (Wide angle, Chronic simple) Glaucoma B. Angle Closure (Narrow angle, Acute congestive) Glaucoma 8
- 9. A. OPEN ANGLE (WIDE ANGLE, CHRONIC SIMPLE) GLAUCOMA ŌĆó It is the most common type. ŌĆó The drain structure in the eye ŌĆō it is called trabecular meshwork ŌĆō looks normal, but the fluid dosenŌĆÖt flow out like it should 9
- 10. B. ANGLE CLOSURE (NARROW ANGLE, ACUTE CONGESTIVE) GLAUCOMA ŌĆó It is less common type ŌĆó Eye doesn't drain right because the drain space between iris and cornea become too narrow ŌĆó This can cause a sudden buildup of pressure in our eye 10
- 11. 11
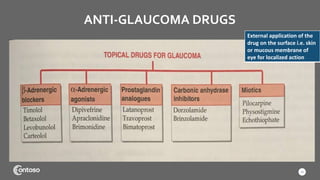
- 12. ANTI-GLAUCOMA DRUGS 12 External application of the drug on the surface i.e. skin or mucous membrane of eye for localized action
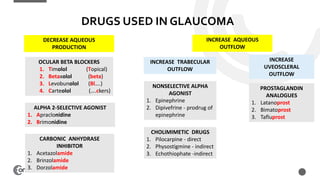
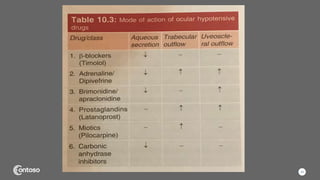
- 13. DRUGS USED IN GLAUCOMA DECREASE AQUEOUS PRODUCTION OCULAR BETA BLOCKERS 1. Timolol (Topical) 2. Betaxolol (beta) 3. Levobunolol (BlŌĆ”.) 4. Carteolol (ŌĆ”.ckers) ALPHA 2-SELECTIVE AGONIST 1. Apraclonidine 2. Brimonidine CARBONIC ANHYDRASE INHIBITOR 1. Acetazolamide 2. Brinzolamide 3. Dorzolamide INCREASE AQUEOUS OUTFLOW INCREASE TRABECULAR OUTFLOW INCREASE UVEOSCLERAL OUTFLOW NONSELECTIVE ALPHA AGONIST 1. Epinephrine 2. Dipivefrine - prodrug of epinephrine CHOLIMIMETIC DRUGS 1. Pilocarpine - direct 2. Physostigmine - indirect 3. Echothiophate -indirect PROSTAGLANDIN ANALOGUES 1. Latanoprost 2. Bimatoprost 3. Tafluprost
- 14. 14
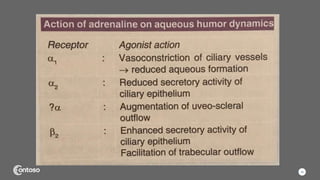
- 15. ALPHA ADRENERGIC AGONIST ’āśAdrenergic Alpha 1:- vasoconstriction of ciliary muscles ’āśAdrenergic Alpha 2:- Reduce action of ciliary epithelium activity ’āśExamples : Dipivefrine, Apraclonidine, Brimonidine. ’āśDipivefrine :- It is a prodrug of ADR; penetrated cornea and is hydrolyzed by the esterase present there into ADR which lowers IOT by augmenting uveoscleral outflow. ’āśApraclonidine :- it decreases aqueous production by primary alpha 2 and subsidiary alpha 1 action on ciliary body ’āśBrimonidine :- it is more Alpha 2 selective and more lipofilic than Apraclonidine. It lowers I.O.T. by reducing aqueous production and by increasing Uveosclereal flow 15
- 16. 16
- 17. BETA ADRENERGIC BLOCKERS ’āś Beta 2 adrenoreceptors located on ciliary epithelium enhance aqueous secretion by a increased cAMP and they are blocked by Timolol / Betaxolol. ’āś Beta blockers reduce the I.O.P by blockade of sympathetic nerve ending in the ciliary epithelium causing a fall in aqueous humor production ’āś Timolol :- it is the prototype of ocular beta blockers it is non selective (╬▓1 + ╬▓2) ’āś Betaxolol :- it is a ╬▓1 selective blocker offering the advantage of less bronchopulmonary and probably less cardiac central and metabolic side effects. However it is less efficious in lowering I.O.T. than timolol because, ocular beta receptors are predominantly of the ╬▓2 subtype. ’āś Most opthmalogist prefer to start with betaxolol and change over to timolol if there is insufficient control or local intolerance to betaxolol 17
- 18. CONTINUED ’āśSide effects are 1. Ocular side effect ’ü▒Stinging(smoke stinging/burning sensation), redness, dryness of eye, corneal hypoesthesia(decrease in sensation), blur vision. 2. Systemic side effect ’ü▒Bronchospasm, bradycardia ( decrease heart rate) 18
- 19. PROSTAGLANDIN ANALOGUE ’āśIt act by increasing Uveoscleral outflow, possibly by increasing permeability of tissues in ciliary muscles or by an action on episcleral vessels(clear layer on top of the white part of eye, outside which conjunctiva is present. ’āśExample : Latanoprost, Travoprost, Bimatoprost. ’ü▒Latanoprost ’üČIt is the 1st choice drug for open angle glaucoma because of ŌĆó Good Efficacy (maximum response of drug) ŌĆó Once daily Application ŌĆó Absence of systemic complication ’ü▒Bimatoprost ’üČIt is equally effective as Latanoprost how ever it has more side effects 19
- 20. 20
- 21. CARBONIC ANHYDRASE INHIBITORS MOA ’āśIt work by inhibiting carbonic anhydrase (isoenzyme II), which is found in ciliary body epithelium. This reduces the formation of bicarbonate ions, which reduces fluid transport, reducing fluid I.O.P ’āśExample Acetazolamide, Dorzolamide ’ü▒Acetazolamide ’üČIt is given Orally ’ü▒ Dorzolamide ’üČIt is given Topically (external application of the drug on the surface i.e. skin or mucous membrane of eye for localized action) 21
- 22. MIOTICS ’āśThese reduce eye pressure by increasing the drainage of intraocular fluid through the trabecular meshwork i.e by increasing ciliary muscle tone ’āśThese drugs especially Pilocarpine previously were the standard antiglaucoma drug ’āśHowever, because of several drawbacks, they are used only as THE LAST OPTION. 22
- 23. 23
- 24. 24 ’āś Start monotherapy with Latanoprost / another PG Analogue / Topical beta blocker If target I.O.T. is not attained, ’āś Either change over to the alternative drug or use both above concurrently (at the same time) . When there are contraindication to PG analogues and/or beta blockers or to supplement their action ’āś Brimonidine / Dorzolamide (occasionally Dipivefrine) are used ’āś Topical miotics and Acetazolamide are added (used as the last Option)
- 25. ANGLE CLOSURE 25 Vigorous therapy employing several measures to reduce I.O.T. ’āśHypertonic mannitol ’āśAcetazolamide ’āśMiotic ’āśTopical beta blockers ’āśApraclonidine 1% (/Latanoprost 0.005%) NOTE These drugs are used only to terminate the attack of angle closure glaucoma Definitive treatment is surgical or laser peripheral iridotomy (standard first-line treatment) These may be treated with these drugs for long periods, but often surgery or laser therapy is ultimately required.
- 26. 26
- 27. TEAM 27 PRABHAT KUMAR SHANTANU NISHAN LAMICHHANE NEHA GHIMIRE NISHANT KHAKUREL
- 28. TEAM 28 NISHIKA SHAH NEHA PRABHA CHATURVEDI NASREEN
- 29. TEAM 29 NISHA RAJ PRAKRITI ADHIKARI
- 30. THANKYOU Visit my Instagram:- @pshantanu @_neeshan pshantanu14@gmail.com nishanlamichhane21@gmail.com Reference : K.D. Tripathi, Wikipedia, Youtube