Growth assessment and monitoring
- 1. Dr. Tauhid Iqbali MBBS (JIPMER) MD Pead Jr. II (PMCH Patna)
- 2. Learning Objectives To define what is physical growth and to know normal pattern of growth To understand what is percentiles z-scores and percentage of mean To know techniques of growth measurement To define growth monitoring To know recommendations for interval and parameters for growth monitoring To know about growth charts To know what are common growth reference charts To know how to calculate z-scores and correlation between percentiles and z-scores Interpretation of growth charts To know applications of growth charts with examples
- 3. GROWTH DEFINITION: Growth denotes a net increase in the size or mass of tissue Occurring because of two factors:- - Multiplication of cells - Increase of intra cellular substance NORMAL PATTERN OF GROWTH FROM CONCEPTION TO ADOLESCENCE FETAL GROWTH(TILL BIRTH ) It is broadly divided into 4 phases: ŌĆó Up to 16 weeks ŌĆō slow rate , less than 10 gram/week (100g) ŌĆó 16-28 weeks - Accelerated rate , approximately 85 g/week (1005g) ŌĆó 28-37 weeks - Maximum rate , nearly 200 g/week (2859g) ŌĆó 37-42 weeks - Decelerated rate , approximately 70 g/week (3685g)
- 4. BIRTH TO SCHOOL-AGED GROWTH (BIRTH TO 12 YEARS) WEIGHT: Infant looses 7-10% of birth weight in 1st week of life Birth weight is again achieved by end of 2nd week Subsequent rate of weight gain is as follows: AGE WEIGHT GAIN 10days-3months 30g/day 3-6 months 20g/day 6-9 months 15g/day 9-12 months 12g/day 1-3 years 3g/day 4-12 years 2g/day
- 5. LENGTH/HEIGHT: Length of term newborn at birth is approximately 50 cm AGE RATE OF LENGTH/Ht INCREASE Birth-3 months 3.5 cm/month 3-6 months 2 cm/month 6-9 months 1.5 cm/month 9-12 months 1.3 cm/month 2-5 years 6-8 cm/year 5-12 years 5 cm/year HEAD CIRCUMFERENCE: Head circumference at birth is 33-35 cm AGE RATE OF HC INCREASE 0-3 months 2 cm/month 3-6 months 1 cm/month 7-12 months 0.5 cm/month 1-3 years 1 cm/6months 3-5 years 1 cm/year
- 6. ADOSESCENT GROWTH(12 YEARS TO 19 YEARS) Peak growth velocity( nearly double the prepubertal GV ) characterized the commencement of adolescent growth In girls peak GV start during early puberty ( Tanner stage II-III) with mean GV of 9cm/yr (range7-11cm/yr) In boys peak GV begins 2-3 years later than in girls at Tanner stage III-IV with mean GV of 10.3 cm/yr (range7-13 cm/yr) The average total growth during pubertal spurt is 27-30 cm Boys have longer growth spurt period than girls
- 7. AGE DEPENDENT Weight Height HC Chest Circumference AGE INDEPENDENT MUAC BMI RaoŌĆÖs Index KanawatiŌĆÖs Index GROWTH PARAMETERS
- 8. TECHNIQUES OF GROWTH MEASUREMENT
- 9. ’é¦ Measure to the nearest 10g for infant and 100g for children ’é¦ Allow tared weighing ’é¦ Weighting time should be about half an hour before or after a feed ’é¦ Preferably measure at same time of the day WEIGHT MEASUREMENT:
- 10. LENGTH/HEIGHT MEASUREMENT Length measurement: For child <2 years of age (or < 87 cm if the age is not available) Recumbent length is measured by infantometer Head support Frankfurt plane Knee straightSole flat on foot piece Toe pointing upward If a child is <2 year old but can not lie down then: Length(cm)= Height+ 0.7
- 11. Height measurement: For child >2 years of age(or >=87 cm if the age is not available) and is able to stand Height is measured by Stadiometer Measure the height to the last completed 0.1 cm Heels Calf muscle Buttocks Shoulder blades Back of head Frankfurt plane Head piece firmly on head Hand on chin Shoulder level Hands by side Left hand on knee: Knee together and leg straight Right hand on shins: Neels against back And base of board If a child is >=2 years of age but can not stand then: Height(cm)= Length ŌĆō 0.7
- 12. HEAD CIRCUMFERENCE MEASUREMENT: Measured upto age of 5 years Should not be measured before 36 hours of age Measured to the nearest 0.1cm Use flexible nonstretchable tape for the measurement Occipital prominence Supraorbital ridges
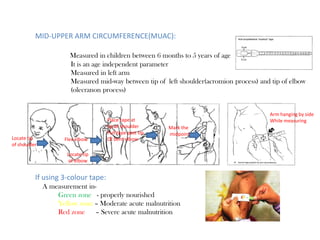
- 13. MID-UPPER ARM CIRCUMFERENCE(MUAC): Measured in children between 6 months to 5 years of age It is an age independent parameter Measured in left arm Measured mid-way between tip of left shoulder(acromion process) and tip of elbow (olecranon process) Locate tip of shoulder Locate tip of elbow Flex elbow Place tape at tip of shoulder Pull tape past tip Of bent elbow Mark the midpoint Arm hanging by side While measuring If using 3-colour tape: A measurement in- Green zone - properly nourished Yellow zone ŌĆō Moderate acute malnutrition Red zone ŌĆō Severe acute malnutrition
- 14. GROWTH MONITORING Definition: Following the growth rate of a child in comparison to a standard by frequent periodic anthropometric measurements in order to assess growth adequacy The purpose is to determine whether a child is growing ŌĆ£normallyŌĆØ or growing ŌĆ£ abnormallyŌĆØ i.e. Has a growth problem Purpose of growth monitoring: Growth Monitoring involves five steps Step 1: Determining correct age of the child Step 2: Accurate weighing of the child Step 3: Plotting the weight accurately on a growth chart of appropriate gender Step 4: Interpreting the direction of the growth curve and recognising if the child is growing properly Step 5: Discussing the childŌĆÖs growth and follow-up action needed with the mother STEPS IN GROWTH MONITORING
- 15. RECOMMENDATIONS FOR INTERVAL AND PARAMETERS FOR GROWTH MONITORING Age group Parameters Intervals Birth -18 months Weight, Length Head circumference Birth, 6wks,10wks,14wks, 9 Mo,15 Mo and 18Mo 18 months -5 yrs Weight, Height 6 monthly >5 years Weight, Height , BMI Annually
- 16. GROWTH CHARTS The most powerful tool for growth monitoring Growth charts are visible display of childŌĆÖs physical growth and development It was first designed by David Morley and was later modified by WHO
- 17. Blue charts for boys and pink charts for girls
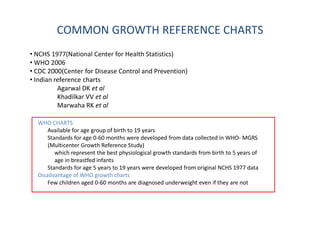
- 18. COMMON GROWTH REFERENCE CHARTS ŌĆó NCHS 1977(National Center for Health Statistics) ŌĆó WHO 2006 ŌĆó CDC 2000(Center for Disease Control and Prevention) ŌĆó Indian reference charts Agarwal DK et al Khadilkar VV et al Marwaha RK et al WHO CHARTS Available for age group of birth to 19 years Standards for age 0-60 months were developed from data collected in WHO- MGRS (Multicenter Growth Reference Study) which represent the best physiological growth standards from birth to 5 years of age in breastfed infants Standards for age 5 years to 19 years were developed from original NCHS 1977 data Disadvantage of WHO growth charts Few children aged 0-60 months are diagnosed underweight even if they are not
- 19. CDC 2000 CHARTS Available for age group of birth ŌĆō 20 years These are revised version of original NCHS 1977 data Sample population were formula/mixed fed children Disadvantage of CDC growth charts Do not truly reflect ideal growth of breastfed children WHICH GROWTH CHART TO USE? RECOMMENDATIONS: Under 5 children - WHO 2006 STANDARDS Above 5 children - Nationally representative references Recommendation for indian children:
- 20. INTERPRETATION OF GROWTH CHARTS AND GROWTH PARAMETERS
- 21. PERCENTILES Percentiles are obtained by dividing an ordered set of data into 100 equal sized group If a 3-month-old child is in the 40th percentile for weight that means 40 percent of 3-month-old boys weigh the same as or less than this baby and 60 percent weigh more 50th percentile means 50 per cent above or under Z-scores or SD scores It is used to describe mathematically how far a measurement is from the median (average) 50% 50% 97% Correlation between percentiles and z-scores Z-score Exact percentile Rounded percentile 0 50 50 -1 15.9 15 -2 2.3 3 -3 0.1 1 1 84.1 85 2 97.7 97 3 99.9 99
- 22. How to calculate Z scores (Standard Deviation Score) Example: Actual length 96.1 cm Median 90.4 cm Standard deviation 3.3 Z score = ( 96.1-90.4)/3.3 = 5.7/3.3 = +1.73 97%
- 23. PERCENTAGE OF MEDIAN This is merely the weight/height of the individual child relative to the average weight/height of the comparable children in the reference population, expressed as a percentage For example: A 80 cm tall girl weigh 8.0 kg and the average weight for 80 cm tall girls is 10.2 kg Therefore, the percent of median for this 8.0 kg girl is 78.4 % For height <90% - Short stature For weight <80% - Underweight Under weight
- 24. Growth chart types Percentile graphs have a narrower range, because the 97th centile corresponds approximately to a Z score +2 Hence a Z-score of +3 or -3 is more likely to be definitely abnormal (above 97 centile or below 3 centile) Percentile chart Z-score chart
- 25. INTERPRETATION OF GROWTH CURVE This is determining whether the child is growing appropriately or not. Normal growth curve: a healthy childŌĆÖs growth curve is parallel to the printed curves on the chart. ŌĆó The direction of the growth curve is more important than the position of the curve on the chart Important consideration on premature infants where growth failure can be over diagnosed, this can be avoided by subtracting the weeks of prematurity from postnatal age when plotting the growth measurements
- 26. A horizontal growth curve (static) : ŌĆó This indicates danger, this means the child is not growing. ŌĆó A sign of disease, especially malnutrition. ŌĆó This makes them prone to recurrent infection as they can not resist disease Downward growth curve: ŌĆó Indicates a very dangerous situation where the child is losing the weight. ŌĆó This requires extra care immediately ’éŚ An upward curve in the growth chart is ideal ’éŚ A flat and downward curves are not desirable
- 27. INTERPERATION OF GROWTH PARAMETERS May be abnormal Use BMI
- 29. CALCULATING AND PLOTTING MPH ’é¦ MPH is plotted on growth chart at 18 years of age ’é¦ Normal range is 2SD above or below the MPH (Which approximately corresponds to +/- 8cm For example: Father Ht - 164cm Mother Ht - 151cm Assessment MPH-151(143-159cm)
- 30. CALCULATING AND PLOTTING GROWTH VELOCITY For example: 12 year old girl Ht ŌĆō 135 cm After 6 months Ht ŌĆō 138.5 cm A = 3.5 B = 6 GV=3.5 X 12/6 =7 cm Per year Point -12.25 years Assessment GV ŌĆō 50 Percentile GV = A x 12/B Per year A- Interval growth B- Months b/t measurements
- 31. 12 year old girl Ht - 135cm,Wt - 28kg Father Ht - 164cm Mother Ht - 151cm Assessment: MPH-151(143-159cm) Ht age-9.5years Wt age-8.5 years Familial short stature
- 32. Follow-up 6 months Ht ŌĆō 138.5 cm GV=3.5 X 12/6 =7 cm Per year Assessment GV ŌĆō 50 Percentile
- 33. 13 year old boy Ht ŌĆō 135cm,Wt ŌĆō 30kg Father Ht-169 Mother Ht-156 Bone age ŌĆō 10.5 years Assessment MPH - 169 cm Height age -9.5 years Weight age -9.5 years Constitutional short stature
- 34. 10 year old girl Ht-120cm Wt-15kg Father Ht-163cm Mother Ht-150cm Interpretation Height age-7years Weight age-4 years Nutritional short stature
- 35. 8 year old boy Ht-100cm Wt-18kg Father Ht-169cm Mother Ht-156cm Bone age-3 years Interpretation Ht age - 3.5cm Wt age - 5 cm Endocrine- GHD/Hypothyroidism
- 36. 12 year old boy, obese Ht-160cm Wt-70kg Father Ht-169cm Mother Ht-156cm Interpretation Ht age-13.5years Wt age-19 years Constitutional obesity
- 37. 12 year boy, Obese Ht-132cm Wt-59kg Father Ht-169cm Mother Ht-156cm Interpretation Ht age ŌĆō 9years Wt age - 15.5years Pathological obesity
- 38. SHORT STATURE Wt age << Ht age < Age ŌĆō Nutritional Ht age << Wt age < Age - Endocrine OBESITY Age < Ht age < Wt age ŌĆō Nutritional Ht age < Age < Wt age - Endocrine