Gynecologic Tumor Markers
- 1. Gynecologic Tumor MarkersDr. WaleedShehadatObstetrician & Gynecologist
- 2. Tumor markers are glycoproteins that are usually detected by monoclonal antibodies.They are produced by the tumor itself or by the body in response to the presence of cancer or certain benign conditions.The levels of tumor marker are not altered in all cancer patients, especially in early stage cancer. The level of some tumor markers can be elevated in patients with noncancerous conditions.Some tumor markers can be used for screening, diagnosis, management, determining response, and recurrence. Some markers show promise as prognostic indicators.
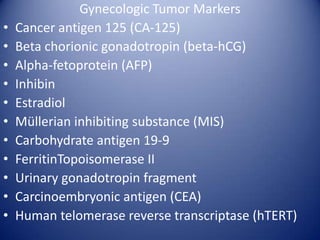
- 3. Gynecologic Tumor MarkersCancer antigen 125 (CA-125)Beta chorionic gonadotropin (beta-hCG)Alpha-fetoprotein (AFP)InhibinEstradiolMĂĽllerian inhibiting substance (MIS)Carbohydrate antigen 19-9FerritinTopoisomerase IIUrinary gonadotropin fragmentCarcinoembryonic antigen (CEA)Human telomerase reverse transcriptase (hTERT)
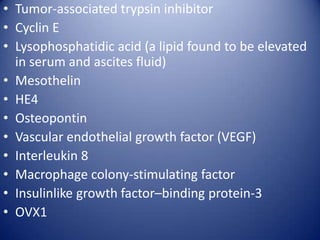
- 4. Tumor-associated trypsin inhibitorCyclin ELysophosphatidic acid (a lipid found to be elevated in serum and ascites fluid)MesothelinHE4OsteopontinVascular endothelial growth factor (VEGF)Interleukin 8Macrophage colony-stimulating factorInsulinlike growth factor–binding protein-3OVX1
- 5. No marker is completely specific; therefore, diagnostic immunohistochemistry testing must be used in conjunction with morphologic and clinical findings.
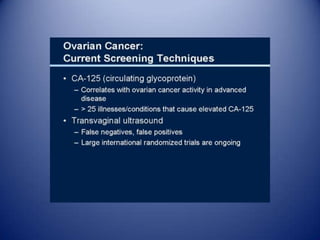
- 14. Cancer Antigen 125The serum CA-125 level has been widely used as a marker for a possible epithelial ovarian cancer in the primary assessment of a pelvic mass.False-positive results may derive from several conditions, especially those associated with peritoneal inflammation, such as endometriosis, adenomyosis, pelvic inflammatory disease, menstruation, uterine fibroids, or benign cysts.Malignancies other than ovarian cancer can also increase CA-125 levels, but the most marked elevations (>1500 U/mL) are generally seen with ovarian cancer.Postmenopausal women with serum levels of CA-125 higher than 35 U/mL or premenopausal women with CA-125 levels higher than 200 U/mL should be referred to a gynecologic oncologist.
- 15. Cancer Antigen 125CA-125 is an important tumor marker for the diagnosis, treatment, and follow-up care of patients with epithelial ovarian cancer and has been recommended for screening. It can be used clinically to determine response to treatment, relapse, and survival.It can be expressed in a number of gynecologic (eg, endometrium, fallopian tube) and nongynecologic (eg, pancreas, breast, colon, lung) cancers. CA-125 levels are frequently elevated with tumor spread beyond the uterus and have been found highly sensitive in detecting extrauterine disease.Serum CA-125 markers are primarily used to monitor the progress of ovarian cancer (A CA-125 level less than 15 U/mL after a standard 6-course treatment generally correlates with longer progression-free intervals, while a CA-125 value greater than 35 U/mL after a standard 6-course chemotherapy treatment predicts the presence of disease).
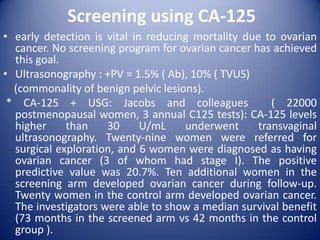
- 16. Screening using CA-125early detection is vital in reducing mortality due to ovarian cancer. No screening program for ovarian cancer has achieved this goal.Ultrasonography : +PV = 1.5% ( Ab), 10% ( TVUS) (commonality of benign pelvic lesions). * CA-125 + USG: Jacobs and colleagues ( 22000 postmenopausal women, 3 annual C125 tests): CA-125 levels higher than 30 U/mL underwent transvaginalultrasonography. Twenty-nine women were referred for surgical exploration, and 6 women were diagnosed as having ovarian cancer (3 of whom had stage I). The positive predictive value was 20.7%. Ten additional women in the screening arm developed ovarian cancer during follow-up. Twenty women in the control arm developed ovarian cancer. The investigators were able to show a median survival benefit (73 months in the screened arm vs 42 months in the control group ).
- 17. Ovarian cancer screening is not recommended for women with no risk factors (RR≤3).For women with increase risk (RR=3-6 times), after evaluating risks and benefits, ovarian cancer screening with CA-125 and/or transvaginalultrasonography can be done.In women at inherited risk (RR>6 times), usually with mutations in ovarian cancer susceptibility genes, should receive screening by a combination of transvaginalultrasonography and CA-125.For patients with mutations in BRCA1 or the mismatch repair genes, MLH1, MSH2, and MSH6, screening should begin around 30-35 years of age.
- 18. For patients with mutations in BRCA2, ovarian cancer screening should be performed around 35-40 years of age.In the next decade, the challenge will be to identify new markers that will complement CA-125 in monitoring ovarian cancer and facilitate screening for occult early-stage disease. The expression of growth factors and their receptors and application of monoclonal antibodies to immunohistochemistry and radionuclide imaging may also provide new areas of diagnostic application for monoclonal antibodies in gynecologic oncology.
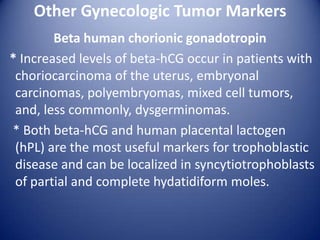
- 19. Other Gynecologic Tumor MarkersBeta human chorionic gonadotropin * Increased levels of beta-hCG occur in patients with choriocarcinoma of the uterus, embryonal carcinomas, polyembryomas, mixed cell tumors, and, less commonly, dysgerminomas. * Both beta-hCG and human placental lactogen (hPL) are the most useful markers for trophoblastic disease and can be localized in syncytiotrophoblasts of partial and complete hydatidiform moles.
- 20. The following diagnostic criteria is commonly used for malignant gestational trophoblastic disease:Plateauing of beta-hCG levels over at least 3 weeks10% or greater rise in beta-hCG for 3 or more values over at least 2 weeksPersistence of beta-hCG 6 months after molar evacuationHistologic identification of choriocarcinoma.
- 21. Patients who have undergone molar pregnancy evacuation should undergo weekly beta-hCG monitoring until normal levels are achieved, then monthly monitoring until 6-12 months of normal values have been achieved. About 20% patients undergoing evacuation of molar pregnancy will develop postmolar gestational trophoblastic disease, usually manifesting as failure to normalize the postevacuation beta-hCG levels. A 10% rise in beta-hCG over 3 or more weekly titers or a beta-hCG titer of 40,000 mIU/L 4-5 months after uterine evacuation constitutes a serological diagnosis of postmolartrophoblastic disease.
- 28. Choriocarcinoma
- 29. MLH1: MutL homolog 1, colon cancer, nonpolyposis type 2 (E. coli), also known as MLH1, is a human gene located on Chromosome 3. It is a gene commonly associated with hereditary nonpolyposis colorectal cancer.MSH2 is a gene commonly associated with Hereditary nonpolyposis colorectal cancerMSH6 is a gene commonly associated with hereditary nonpolyposis colorectal cancer