HIPAA Omnibus Rule: Critical Changes for Business Associates
- 1. HIPAA Omnibus Rule Critical Changes for Business Associates Presented by Susan A. Miller, JD Hosted by
- 2. agenda ŌĆó ŌĆó ŌĆó ŌĆó ŌĆó ŌĆó ŌĆó What the Omnibus Rule includes Effective and Compliance Dates Business Associates Breach Notification Genetic Information Non-discrimination Act (GINA) Enforcement Questions
- 3. Dates + 4 Rules The Omnibus Final Rule is effective on March 26, 2013 and the compliance date is September 23, 2013: ŌĆó July 2010 Notice of Proposed Rule Making (NPRM) on HITECH privacy and security changes to HIPAA ŌĆó October 2009 Notice of Proposed Rule Making (NPRM) on Genetic Information Nondiscrimination Act (GINA) changes to HIPAA ŌĆó August 2009 Interim Final Rule (IFR) on HIPAA Breach Notification ŌĆó October 2009 Interim Final Rule (IFR) on HIPAA Enforcement Rule
- 4. Business Associates Under HITECH Who is a Business Associate? ŌŚÅ ŌŚÅ Omnibus Final Rule: An entity that ŌĆ£ŌĆ”creates, receives, maintains, or transmits [PHI] for a function or activity regulated by [HIPAA]ŌĆ”ŌĆØ on behalf of a Covered Entity Omnibus Final Rule expanded the definition of Business Associates to include: ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ Health Information Organizations E-prescribing Gateways Personal Health Records (PHR) providers on behalf of a Covered Entity Patient Safety Organizations Subcontractors that create, receive, maintain, or transmit Protected Health Information (PHI) on behalf of Business Associates Subcontractor means a person whom a Business Associate delegates a function, activity, or service, other than in the capacity of a member of the workforce of such Business Associate
- 5. New Business Associate Obligations Summary of BA Obligations Prior to HITECH ŌŚÅ Prior to the HITECH Act, a BA was not subject to direct enforcement and compliance with HIPAA Privacy and Security requirements ŌŚÅ A BAŌĆÖs obligations arose solely under the terms of its BA agreement with the Covered Entity (CE) ŌŚÅ The BA was subject only to contractual remedies for breach of the BA agreement (BAA)
- 6. New Business Associate Obligations Summary of BA Obligations Under Omnibus Final Rule ŌŚÅ Direct compliance with all requirements of the HIPAA ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ Security Rule Directly liable for impermissible uses and disclosures of PHI under HIPAA Provide CE with notice of breach in accordance with the Breach Notification Rule Required to provide access to a copy of electronic PHI to the CE (or the individual) Provide PHI where required by the Secretary to investigate the BAŌĆÖs compliance with HIPAA Provide an accounting of disclosures as required by HITECH (Final Rule Pending)
- 7. New Business Associate Obligations BA Security Rule Compliance and Oversight ŌŚÅ The Omnibus Final Rule requires BAs to comply with the HIPAA Security RuleŌĆÖs requirements and implement policies and procedures in the same manner as a CE ŌŚÅ Requires BA to implement: ŌŚÅ Administrative ŌŚÅ Physical, and ŌŚÅ Technical Safeguards in compliance with the HIPAA Security Rule (most BA agreements require this by contact) ŌŚÅ Compliance date under the Omnibus Final Rule ŌĆō 9/23/13
- 8. New Business Associate Obligations BA Security Rule Compliance and Oversight (ContŌĆÖd) ŌŚÅ BAs must conduct a risk assessment and be more ŌŚÅ ŌŚÅ ŌŚÅ proactive and diligent to monitor new rules, regulations and guidance Large BAs may already have a comprehensive security compliance program Smaller BAs, particularly those that are not exclusively dedicated to the healthcare industry, may have a lot of work to do The good news ŌĆō the Security Rule reflects prudent risk management practices and flexible standards
- 9. New Business Associate Obligations BA Privacy Rule Limited to HITECH Changes ŌŚÅ The HITECH Act does not impose ALL Privacy Rule obligations upon a BA ŌŚÅ BAs are subject to direct enforcement of HIPAA Privacy obligations and penalties in the same manner as a CE, BUT only to the extent required under HITECH ŌĆō not all the HIPAA Privacy Rule obligations
- 10. New Business Associate Obligations BA Privacy Rule Impacts ŌŚÅ Disclosure of Protected Health Information (PHI) must be ŌŚÅ kept to limited data set or minimum necessary ŌŚÅ ŌŚÅ ŌŚÅ Health Provider must honor a request by any individual to restrict disclosure of PHI to Health Plan if individual pays for service out-of-pocket in full Individual has a right to a copy of PHI in electronic format Sale of PHI prohibited unless authorized by individual Certain marketing communications require authorizations ŌŚÅ extent applicable to BAŌĆÖs access to PHI on behalf of CE Compliance date under Omnibus Final Rule ŌĆō 9/23/13 ŌŚÅ BA must comply with all the above requirements to the
- 11. New Business Associate Obligations BAs and Breach Notification ŌŚÅ BA must notify CE in the event of a breach of unsecured ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ PHI Notice must be made without unreasonable delay and not more than 60 days from when the breach was discovered (CEs typically seek to shorten this time) Discovery is when BA knew or ŌĆ£should have knownŌĆØ Breach Notice to CE must identify the individuals whose PHI was involved in the breach BA must provide any other available information that the CE is required to provide in its notice to individuals
- 12. New Business Associate Obligations BA Agreements (BAA)s Required Provisions ŌŚÅ Omnibus Final Rule clarified the required HITECH Act Provisions: ŌŚÅ BA required to comply with ALL HIPAA Security Rule obligations ŌŚÅ BA must report to CE any breach or unsecured PHI as required by the Breach Notification Rule ŌŚÅ BA must enter into BAAs with sub-contactors imposing the same obligations that apply to the BA ŌŚÅ BA must comply with the HIPAA Privacy Rule to the extent the BA is carrying out a CEŌĆÖs obligations under the HIPA Privacy Rule
- 13. New Business Associate Obligations BAAs Implementation Timeline ŌŚÅ For HIPAA compliant BAAs executed prior to publication of the Final Rule (1/25/2013) ŌĆō Entities may have up to 1 additional year beyond the 9/23/2013 Compliance Date ŌŚÅ BAAs executed PRIOR to 1/25/2013 that are not set to terminate or renew before 9/23/2013 ŌĆō These must be compliant by the earlier of the renewal date or 9/22/2014 ŌŚÅ For new BAAs executed AFTER 1/25/2013 or existing BAAs scheduled to be renewed before 9/23/2013 ŌĆō These must be compliant by 9/23/2013
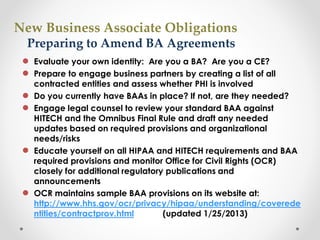
- 14. New Business Associate Obligations Preparing to Amend BA Agreements ŌŚÅ Evaluate your own identity: Are you a BA? Are you a CE? ŌŚÅ Prepare to engage business partners by creating a list of all ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ contracted entities and assess whether PHI is involved Do you currently have BAAs in place? If not, are they needed? Engage legal counsel to review your standard BAA against HITECH and the Omnibus Final Rule and draft any needed updates based on required provisions and organizational needs/risks Educate yourself on all HIPAA and HITECH requirements and BAA required provisions and monitor Office for Civil Rights (OCR) closely for additional regulatory publications and announcements OCR maintains sample BAA provisions on its website at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/coverede ntities/contractprov.html (updated 1/25/2013)
- 15. New Business Associate Obligations Agency Relationship Considerations ŌŚÅ The Omnibus Final Rule makes clear that a CE is liable ŌŚÅ ŌŚÅ for the acts or omissions of its BA acting within the scope of ŌĆ£agencyŌĆØ BAs are likewise liable for the acts or omissions of its Subcontractor acting within the scope of ŌĆ£agencyŌĆØ This means: ŌŚÅ An entity can be penalized for its agentŌĆÖs violations ŌŚÅ Knowledge by the agent will be imputed to the principal (e.g., knowledge of a breach or other violation) ŌŚÅ Federal common law of Agency will govern whether an agency relationship exists between the parties regardless of what the contract actually says
- 16. New Business Associate Obligations Agency Relationship Considerations ŌŚÅ ŌŚÅ Whether an agency relationship exists will depend on the right or authority of the CE to control the BAs conduct and performance based on the right to give interim instructions Agency Consideration Factors ŌŚÅ The time, place and purpose of the BAs conduct ŌŚÅ Whether the BA engaged in a course of conduct subject to ŌŚÅ ŌŚÅ ŌŚÅ (ContŌĆÖd) control by the CE Whether the BAŌĆÖs conduct is commonly done by a BA Whether or not the CE reasonably expected that a BA would engage in the conduct in question This will be a fact-specific analysis and in some cases an agency relationship may exist simply based on the nature of the relationship between the CE and BA
- 17. New Business Associate Obligations Liability for Agents ŌŚÅ ŌŚÅ ŌŚÅ CE is liable for acts of agents within the scope of agency ŌŚÅ Includes members of workforces ŌŚÅ Includes agents who are business associates regardless of whether BA contract is in place BA is also liable for acts of agents within the scope of agency ŌŚÅ Workforce ŌŚÅ Agents who are subcontractor business associates Fact specific: taking into account ŌŚÅ Business associate contract and ŌŚÅ Totality of circumstances of relationship ŌŚÅ Does the CE have authority to provide interim instructions or directions?
- 18. New Business Associate Obligations BAs: Evaluate HIPAA Security Rule Compliance ŌŚÅ Review OCR Security Rule Guidance at ŌŚÅ National Institute of Standards and Technology (NIST) Special Publication (SP) 800-66 is another good resource Conduct a HIPAA Security Risk Assessment ŌŚÅ http://www.hhs.gov/ocr/privacy/hipaa/administrative/securityrule/s ecurityruleguidance.html ŌŚÅ This will help identify areas of vulnerability and threats against ŌŚÅ ŌŚÅ existing controls and actions to address NIST SP 800-30 is a good place to start NIST Security Risk Assessment Toolkit; download free at http://scap.nist.gov/hipaa/ ŌŚÅ NIST SPs available at: ŌŚÅ Review OCR Enforcement Audit Protocol at http://csrc.nist.gov/publications/PubsSPs.html http://www.hhs.gov/ocr/privacy/hipaa/enforcement/audit/protocol. html
- 19. Breach Notification ŌŚÅ HITECH Act: First federal law mandating breach notification for the health care industry; applies to: ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ Covered Entities Business Associates Personal Health Records (PHR) vendors, and PHR service providers ŌŚÅ Federal Trade Commission (FTC) regulates PHRs ŌŚÅ Health and Human Services (HHS) regulations CEs and BAs
- 20. Breach Notification Remember State Law ŌŚÅ 46 states (plus DC, Puerto Rico, and the Virgin Islands) have notification laws ŌŚÅ Evaluate state law as well as the Omnibus Rule requirements: ŌŚÅ Trigger ŌŚÅ Timing ŌŚÅ Content ŌŚÅ Recipients
- 21. Data Breach Notification Overview ŌŚÅ Upon discovery of a ŌŚÅ Breach of ŌŚÅ Unsecured ŌŚÅ Protected Health Information (PHI) ŌŚÅ Covered Entities and Business Associates must make notifications ŌŚÅ Subject to certain exceptions
- 22. Definition of Breach ŌŚÅ Breach of ŌŚÅ Unauthorized acquisition, access, use disclosure of unsecured PHI ŌŚÅ In a manner not permitted by the HIPAA Privacy Rule ŌŚÅ That compromises the security or privacy of PHI ŌŚÅ So far so good, but ŌĆ”
- 23. Omnibus Final Rule Presumption ŌŚÅ An impermissible acquisition, access, use disclosure of unsecured PHI is ŌŚÅ Presumed to be a reportable breach ŌŚÅ UNLESS the entity demonstrates that there is a low probability that the PHI has been compromised (lo pro co) ŌŚÅ Compromise is not defined by the HIPAA Rules; from the preamble: ŌĆ£inappropriately viewed, re-identified, re-disclosed, or otherwise misusedŌĆØ
- 24. Breach Risk Assessment ŌŚÅ A documented risk assessment needs to demonstrates that there is a low probability that the PHI has been compromised ŌŚÅ Four mandatory factors: ŌŚÅ ŌŚÅ ŌŚÅ ŌŚÅ What PHI: Nature and extent of PHI involved Who: The unauthorized person who used the PHI or to whom the disclosure was made Acquired: Whether the PHI actually was acquired or viewed Mitigation: The extent to which the risk to the PHI has been mitigated ŌŚÅ Other factors may be considered ŌĆō Evaluation of overall probability
- 25. Breach Risk Assessment ŌŚÅ Risk Assessment must be: ŌŚÅ Thorough ŌŚÅ Completed in good faith ŌŚÅ Have reasonable conclusions ŌŚÅ Discretion to provide notification without performing risk assessment
- 26. Lose an Exception ŌŚÅ Unauthorized person not reasonably have been able to retain PHI ŌŚÅ Certain good faith or inadvertent access by or disclosures to workforce in same organization ŌŚÅ De-identified information does not pose risk of harm ŌŚÅ Limited data sets without birth dates and zip codes
- 27. Timing of Notice ŌŚÅ Notification must be made ŌĆ£without unreasonable delayŌĆØ ŌŚÅ No more than 60 days after discovery ŌŚÅ Subject to law enforcement delay
- 28. Discovery ŌŚÅ ŌĆ£DiscoveryŌĆØ of a breach occurs when: ŌŚÅ Entity has actual knowledge of a breach including through a workforce member or agent (but not person committing the breach) or ŌŚÅ Using reasonable diligence, entity would have known of the breach ŌŚÅ Remember: agency is based on federal common law
- 29. Contents of Notice to Individuals ŌŚÅNotices must contain: ŌŚÅ Brief description of what occurred ŌŚÅ Description of types of unsecured PHI involved (e.g., name, SSN, DOB, address) but not the actual PHI ŌŚÅ Steps individuals should take to protect themselves ŌŚÅ Brief description of what Covered Entity is doing to investigate the breach, mitigate the damage, and protect against further breaches ŌŚÅ Contact information for questions
- 30. Breach Notification ŌŚÅ Covered Entity to notify affected individuals ŌŚÅ Written notice ŌŚÅ Substitute notice ŌŚÅ Covered Entity to notify HHS ŌŚÅ Timing depends on the size of the breach ŌŚÅ ŌŚÅ 500 or more = contemporaneous notification Small breaches (<500) = annual notification ŌŚÅ Within 60 days of the end of the calendar year in which the breach was discovered (not occurred) ŌŚÅ Covered Entity may have to notify media if more than 500 residents in a State affected ŌŚÅ Business Associates to notify Covered Entity
- 31. Practical Steps ŌŚÅ Revise breach notification policies and procedures ŌŚÅ Security Risk Analysis ŌĆō revisit (or do) ŌŚÅ Develop or revisit Security Incident Response Plan ŌŚÅ Pay special attention to portable media and personal devices ŌŚÅ Train entire workforce ŌŚÅ ŌŚÅ ŌŚÅ Avoidance Alert to potential breaches Response to breach
- 32. Practical Steps ŌŚÅ Prepare incident response team ŌŚÅ Be ready to respond to news media attention ŌĆō have a designated spokesperson ŌŚÅ Consider tightening Business Associate Agreements, particularly for agents ŌŚÅ Encryption! Make the most of the encryption safe harbor, and Verify document destruction ŌŚÅ National Institute of Standards and Technology (NIST) Guidance specifying the technologies and methodologies that render PHI unusable, unreadable, or indecipherable to unauthorized individuals ŌŚÅ Audit access to PHI and enforce policies
- 33. GINA ŌŚÅ Genetic Information: broadly defined to include manifestation of a disease or disorder in a family member of an individual in addition of genetic tests of individuals and family members and receipt if genetic services ŌŚÅ A Health Plan that uses or discloses PHI for underwriting purposes must revise its NPP stating that it will not use or disclose genetic information for such purposes ŌŚÅ Health Plan definition has also been revised; HHS has exercised its authority to expand GINA to include all Health Plans except for Long Term Care Health Plans
- 34. Increased Enforcement ŌŚÅ HITECH Act significantly strengthened HIPAA Enforcement ŌŚÅ Interim Final Rule of October 2009 ŌŚÅ Created 4 categories of culpability with corresponding penalties ŌŚÅ Took effect immediately ŌŚÅ Omnibus Rule = Final Enforcement Rule ŌŚÅ Enforcement Rule applies to Covered Entities and Business Associates
- 35. Increased Enforcement ŌŚÅ Focus on Willful Neglect ŌŚÅ Willful Neglect: conscious, intentional failure or reckless indifference to the obligation to comply with HIPAA ŌŚÅ OCR will investigate all cases of possible neglect ŌŚÅ OCR will impose penalty on all violations due to willful neglect
- 36. Increased Enforcement Violation Category Each Valuation All Identical Violations for Calendar Year Did Not Know $100 - $50,000 $1,500,000 Reasonable Cause $1000 - $50,000 $1,500,000 Willful Neglect ŌĆō corrected in 30 days $10,000 - $50,000 $1,500,000 Willful Neglect ŌĆō not corrected $50,000 $1,500,000 Limits are per type of violation, e.g., four types of continuous violations over three years could equal $18 million
- 37. What to Do Now! ŌŚÅ Create a Culture of Compliance ŌŚÅ OCR aggressively enforcing the HIPAA Privacy, Breach and Security Rules ŌŚÅ OCR suggests that Covered Entities and Business Associates should have a robust HIPAA Privacy and Security Compliance Program, including: ŌŚÅ Employee Training ŌŚÅ Vigilant implementation of policies and ŌŚÅ ŌŚÅ procedures A prompt plan to respond to incidents and breaches Regular internal audits
- 38. Sample Fines ŌĆó CVS: Privacy, $2.25M, 2009: Complaint ŌĆó Cignet: Privacy, $4.3 M, 2011: CMP, Complaint ŌĆó Phoenix Cardiac Surgery: Privacy & Security $100K, 2012: OCR Audit ŌĆó MEEI: Security, $1.5M, 2012: Self Reported Breach ŌĆó BCBS Tennessee, $1.5M, 2012: Self Reported Breach ŌĆó Alaska Medicaid, Security, $1.7 M, 2012: Self Reported Breach ŌĆó Hospice of North Idaho, Security, $50,000, 2013: Self Reported Breach of less than 500 ŌĆó PLUS Onerous Corrective Action Plans
- 39. QUESTIONS Susan A. Miller, JD TMSAM@aol.com (O) 978-3692092 (C) 978-505-5660 Thank You!




![Business Associates Under HITECH
Who is a Business Associate?
ŌŚÅ
ŌŚÅ
Omnibus Final Rule: An entity that ŌĆ£ŌĆ”creates, receives,
maintains, or transmits [PHI] for a function or activity regulated
by [HIPAA]ŌĆ”ŌĆØ on behalf of a Covered Entity
Omnibus Final Rule expanded the definition of Business
Associates to include:
ŌŚÅ
ŌŚÅ
ŌŚÅ
ŌŚÅ
ŌŚÅ
ŌŚÅ
Health Information Organizations
E-prescribing Gateways
Personal Health Records (PHR) providers on behalf of a Covered
Entity
Patient Safety Organizations
Subcontractors that create, receive, maintain, or transmit Protected
Health Information (PHI) on behalf of Business Associates
Subcontractor means a person whom a Business Associate
delegates a function, activity, or service, other than in the
capacity of a member of the workforce of such Business
Associate](https://image.slidesharecdn.com/hipaaomnibusruleapril11ba-131127131334-phpapp01/85/HIPAA-Omnibus-Rule-Critical-Changes-for-Business-Associates-4-320.jpg)