Hirschsprungs disease
- 1. Hirschsprung’s Disease R.K.Bagdi Senior Consultant Apollo Children;s Hospital
- 2. Patient S.C. • Newborn male • Full-term, uncomplicated vaginal delivery • Normal birth weight: 3115 g • Apgars 91, 95 • Mother: 36 yo, G1P0, healthy
- 3. Patient S.C. • Started breast feeding DOL 1 • DOL 2-3 noted to have increasing abdominal distention • No meconium passed in first 24 hrs of life • 1 episode Non-bilious emesis
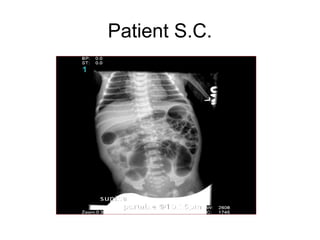
- 4. Patient S.C.
- 5. Patient S.C. • Pediatric Surgical Consult • Rectal Exam – Empty rectal ampulla – Tight anal sphincter – Large amount of stool and air upon withdrawal of finger
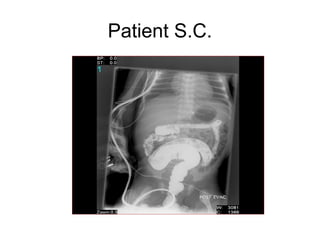
- 6. Patient S.C.
- 7. Patient S.C. • Rectal mucosal biopsy – No ganglia identified
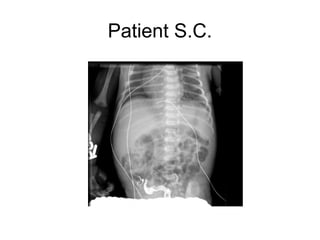
- 8. Patient S.C.
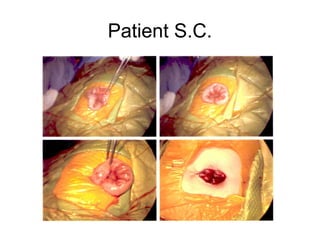
- 9. Patient S.C. • Pt taken to OR for end colostomy and Hartmann’s pouch • Dilated descending and sigmoid colon • Prominent colonic blood vessels • Site of colostomy, frozen section of colonic muscularis propria revealed ganglion cells
- 10. Patient S.C.
- 11. Patient S.C. • Postoperative course uneventful • Stool from colostomy POD 1 • Tolerated breast feeding • Discharged POD 6 • 2nd stage pull through procedure planned in several weeks
- 12. Hirschsprung’s Disease R.K.Bagdi Apollo Children’s Hospital
- 13. Hirschsprung’s Disease • Neurogenic form of intestinal obstruction • Absence of ganglion cells in the myenteric and submucosal plexus • Failure in relaxation of the internal anal sphincter and affected bowel • Upstream bowel becomes dilated secondary to functional obstruction
- 14. History • 1691 Ruysch latin texts • 1886 Harald Hirschsprung – autopsy • 1901 Tittel – histologic findings • 1949 Swenson – pathophysiology and definitive operative treatment
- 15. Epidemiology • Prevalence: 1/5000 births • 3-5% of pts have Down’s syndrome • Definite family history • 80% affected are boys • Total colonic aganglionosis, 35% girls • >95% cases are full term babies
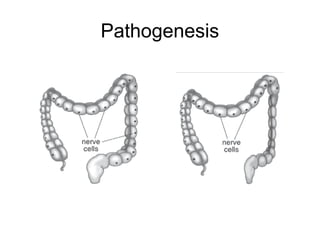
- 16. Pathogenesis
- 17. Pathogenesis • Failure of neural crest cells to migrate caudally • Aganglionosis begins at anorectal line • 80% involve only rectosigmoid area • 10% extend proximal to splenic flexure • 10% involves the entire colon and part of small bowel • Rarely involves entire gastrointestinal tract
- 18. Pathogenesis—genetics • 10th chromosome • RET-protooncogene • Endothelin B gene
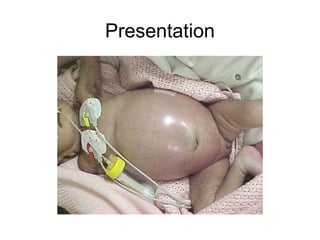
- 19. Presentation
- 20. Presentation • Severe abdominal distention • 95% - failure to pass meconium in first 24 hours life • Bilious vomiting • Older children - constipation, failure to thrive • 10-15% - severe diarrhea alternating w/ constipation—enterocolitis of Hirschsprung’s disease
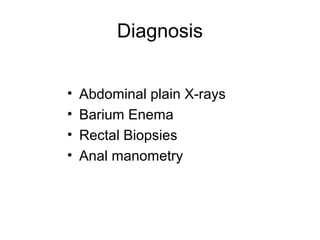
- 21. Diagnosis • Abdominal plain X-rays • Barium Enema • Rectal Biopsies • Anal manometry
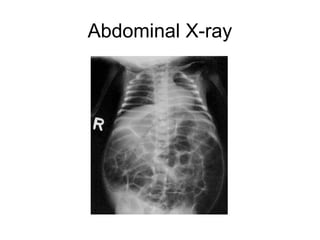
- 22. Abdominal X-ray
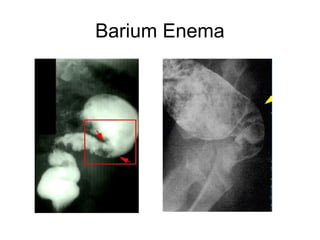
- 23. Barium Enema
- 24. Barium Enema • Less sensitive for detecting short lesions, total colon aganglionosis, and disease of the newborn • Many newborns do NOT show definitive transition zone • Delayed evacuation of contrast
- 25. Rectal biopsy • Submucosal suction biopsy – Meissner’s submucosal plexus • Full thickness rectal biopsy – Auerbach’s myenteric plexus • Acetylcholinesterase staining – increased staining of neurofibrils
- 26. Anorectal manometry • Absent rectoanal inhibitory reflex • Lack of internal anal sphincter relaxation in response to rectal stretch
- 27. Surgical Options • Swenson Procedure (1948) • Duhamel Procedure (1960) • Soave Procedure (1963)
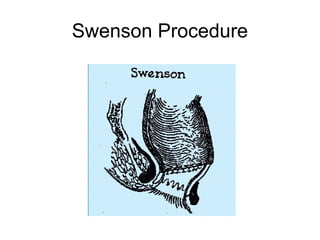
- 28. Swenson Procedure • Sharp extrarectal dissection down to 2 cm above the anal canal • Aganglionic colonic segment resected • End-to-end anastamosis of normal proximal colon to anal canal • Completely removes defective aganglionic colon
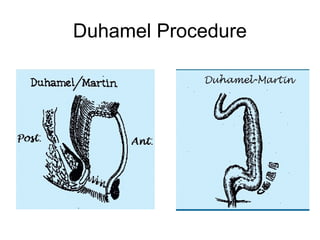
- 30. Duhamel Procedure • Posterior portion of defective colon segment resected • Side to side anastamosis to left over portion of rectum • Constipation a major problem d/t remaining aganglionic tissue • Simpler operation, less dissection
- 32. Soave Procedure • Circumferential cut through muscular coat of colon at peritoneal reflection • Mucosa separated from the muscular coat down to the anal canal • Proximal normal colon is pulled through retained muscular sleeve • Telescoping anastamosis of normal colon to anal canal
- 33. Soave Procedure
- 34. Soave Procedure • Advantage: rectal intramural dissection ensures no damage to pelvic neural structures • Higher rate enterocolitis, diarrhea • Problems w/ cuff abscesses, often requires repeated dilations
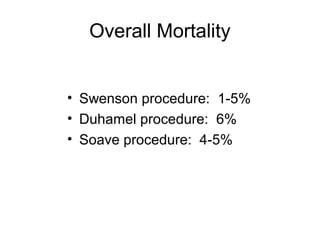
- 35. Overall Mortality • Swenson procedure: 1-5% • Duhamel procedure: 6% • Soave procedure: 4-5%
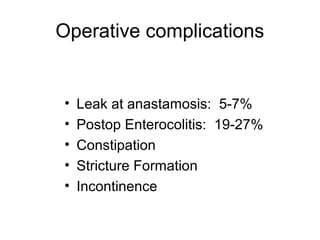
- 36. Operative complications • Leak at anastamosis: 5-7% • Postop Enterocolitis: 19-27% • Constipation • Stricture Formation • Incontinence
- 37. One vs Two Stage procedure • Historically, two stage procedure performed: preliminary colostomy, then completion pull through • Delicate muscular sphincters of newborn may be injured • 1980s, 1 stage procedures became more popular
- 38. One vs Two Stage procedure – Early complications: No difference in incidence of anastomotic leak, pelvic infection, prolonged ileus, wound infection, wound dehiscence – Late complications: No difference in incidence of anastomonic stricture, late obstruction, constipation, incontinence, urgency – Postoperative enterocolitis higher in 1 stage (42% vs 22%)
- 39. Laparoscopic techniques • Small studies of laparoscopic pull through procedures • Excised aganglionic tissues removed through anal canal, no abdominal incision • Better results in terms of pain, return of bowel function, hospital stay • Similar incidence of leaks, pelvic abscesses, enterocolitis, postop bowel function