hyperparathyroidism imaging metabolic bone disease.pptx
- 1. Presenter: Dr. K Revathi Avani Moderator: Dr. B V G Srinivas.
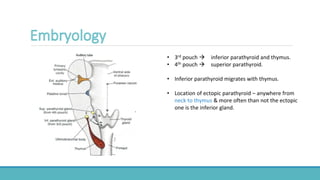
- 2. • 3rd pouch ïƒ inferior parathyroid and thymus. • 4th pouch ïƒ superior parathyroid. • Inferior parathyroid migrates with thymus. • Location of ectopic parathyroid – anywhere from neck to thymus & more often than not the ectopic one is the inferior gland.
- 3. • Normally - visceral space of the neck, pos- terior to the thyroid gland, in the vicinity of the tracheoesophageal groove. • Other structures near the tracheoesophageal groove - paratracheal lymph node chain and the recurrent laryngeal nerve. • They may be located either inside or outside the thyroid capsule
- 4. SUPERIOR PARATHYROID INFERIOR PARATHYROID NORMAL LOCATION Posterior aspect of superior or middle 1/3rd of thyroid. Inferior lobe - Posterior / Anterior / lateral aspect ECTOPIC • Above upper pole of thyroid • Posterior to pharynx or esophagus – in neck / superior mediastinum • Intra thyroid • Neck – in anterior mediastinum • Intra thyroidal • In the thymus- posterior aspect of thymic capsule. • Great vessels – adjacent to carotid sheath
- 5. ➢Microdeletion at 22q11. ➢Failure of the development of the 3rd & 4th pharyngeal pouches ➢Affecting the thymus and parathyroid glands. ➢ Poor thymic development ïƒ abnormal immune system development and deficiencies in T-cells. ➢ Improper parathyroid gland development leads to hypocalcemia. ➢ Patients with DiGeorge Syndrome can also present with congenital cardiac defects (particularly of the outflow tracts), abnormal facial development, and cleft palates
- 6. Temporal bone malformations • lateral semicircular canal dysplasia • dense stapes superstructure Brain and cerebrovascular malformations • Persistent cavum septum pellucidi • Aberrant cortical veins • Polymicrogyria • White matter hyperintensities • Brain volume loss, most pronounced in the cerebellum. Cardiovascular defects, particularly conotruncal defects, • Tetrology of fallot • Interrupted aortic arch.
- 7. ✓ Maintains Calcium homeostasis ✓ Promotes bone remodeling ✓ Low PTH ïƒ bone formation ✓ Increases calcium absorption indirectly also by promoting vitamin D synthesis.
- 11. Presentation : â–ªFemales > Males â–ªAge > 45 years. â–ªAsymptomatic. (routine lab investigation ïƒ increased calcium ) â–ªCauses: 1. Single gland adenoma (85 %) 2. Multiple gland adenoma (14 %) 3. Rare – familial hypocalciuric hypercalcemia, carcinoma, ectopic PTH secretion.
- 12. Causes: ➢CKD, Vitamin D or calcium deficiency. ➢Ineffective renal functioning - PO4 excretion and activation of Vitamin D are both reduced, and Ca reabsorption falls. ➢As a result of low Ca and high PO4 levels, PTH is elevated.
- 13. Signs, Symptoms, Complications: Renal osteodystrophy in patients with CKD. ~Primary hyperparathyroidism: Bone pain, increased fractures, and osteitis fibrosa cystica. Calciphylaxis can also occur; indicate that Ca - PO4 products deposit in the blood vessels, fat, and skin, leading to thrombosis and necrosis. Though rare, this is a serious complication of secondary hyperparathyroidism.
- 14. ➢After longstanding secondary hyperparathyroidism ➢Secondary hyperparathyroidism that persists after successful renal transplantation. ➢Long-standing chronic kidney disease (CKD) is associated with several metabolic disturbances that lead to increased secretion of PTH, including hyperphosphatemia, calcitriol deficiency, and hypocalcaemia. ➢Hyperphosphatemia has a direct stimulatory effect on the parathyroid gland cell resulting in nodular hyperplasia and increased PTH secretion.
- 15. •They also may become resistant to calcimimetic treatment. •The main indication for treatment is persistent hypercalcemia and/or an increased PTH. •Primary treatment is surgery. Common procedures are - 1. Total parathyroidectomy with or without autotransplantation 2. Subtotal parathyroidectomy, and 3. Limited parathyroidectomy.
- 17. ➢ ULTRASOUND : •May be diagnostic in patients with a negative result at 99mTc sestamibi scintigraphy. •For correlating or confirming uncertain findings. •Combined USG and 99mTc sestamibi scintigraphy are reported to have increased sensitivity for the preoperative localization of parathyroid adenomas.
- 18. Pre operative knowledge of the likelihood of an ectopic superior gland in the tracheoesophageal groove facilitates surgical exploration. Parathyroid glands are composed of chief cells, oxyphil cells, and transitional oxyphil cells mixed with adipose tissue.  Chief cells ïƒ PTH.  The oxyphil cells are packed with mitochondria, and their function is unknown.
- 19. •For hyperfunctioning para-thyroid localization - thallium-201 scintigraphy. •201Tl is taken up by both thyroid and parathyroid. • it was used in conjunction with 99mTc pertechnetate, which is taken up only by the thyroid. •The 99mTc scintigram then was digitally subtracted from the 201Tl scintigram to allow parathyroid localization. • 99mTcsestamibi rapidly replaced thallium-201 for parathyroid scintigraphy due to better dosimetry and sensitivity. •A variation of this method is the subtraction of thyroid images obtained with iodine-123 or 99mTc pertechnetate from those obtained with 99mTc sestamibi.
- 20. Single-isotope dual-phase (early- and delayed-phase) scintigraphic technique : • 99mTc sestamibi consists of lipophilic cationic molecules. •After intravenous injection, the molecules are distributed according to blood flow in the body, cross the cell membranes by passive diffusion, and become concentrated intracellularly in the region of the mitochondria •99mTc sestamibi washes out more rapidly from the thyroid gland than from hyperfunctioning parathyroid glands. •It is normally is distributed to the parotid and submandibular salivary glands, thyroid gland, heart, and liver, mild generalized uptake in the bone marrow. •In younger individuals, mild to moderate thymic uptake and brown fat uptake may also be seen. • Uptake is not seen in normal parathyroid glands.
- 21. • Single injection of 99mTc sestamibi, followed by imaging at approximately 10–15 minutes and 1.5–3 hours after the injection. • Parathyroid adenoma showing delayed washout. SPECT
- 22. • Cortical bone erosion – Phalanges •Most sensitive site : Radial aspects of middle phalanges of index and middle fingers. • Tufts of distal phalanges. •Acrosteolysis – distal phalanges, Outer clavicle, pubic symphysis, sacroiliac joints, proximal medial cortex of tibia, proximal humeral shaft, ribs and femur.
- 27. ◦ OSTEOCLASTIC ACTIVITY IN HAVERSIAN CANALS. ◦ Radiographic translucencies in cortex – Cortical tunneling. ◦ Non specific – also seen in Paget’s disease of bone, normal childhood ( cond. with increased bone turnover).
- 29. ➢Deposition of CPPD crystals ïƒ articular and fibrocartilage visible on radiographs. ➢X rays of : Hand ïƒ triangular ligament. Knees ïƒ articular cartilage and menisci. Symphysis pubis.
- 30. ➢Osteoclastic resorption ïƒ Cystic lesion in bone. ➢Cavities filled with fibrous tissue and osteoclasts, fibrous tissue, necrotic and hemorrhagic liquefaction. ➢On x rays : Low density multiloculated cysts Expansion of bones. ➢ Can be mistaken for neoplastic lesions.
- 33. m/c in pt with 20 to CKD ïƒ Excessive accumulation of poorly mineralized osteoid. Radiographically dense than normal bone. Axial skeleton >> effected. Vertebral bodies – End bodies >> effected. Bands of dense bones adjacent to end plates with central band of lower bone density. In 10 – Bone resorption ïƒ Exaggerated osteoblastic response.
- 35. Excessive resorption ïƒ Radiodensity. In postmenopausal women ïƒ bone resorption >> new bone formation. On BMD cortical bone density >> trabecular bone. Marked reduction – In bones with predominant cortical bone (distal forearm). Parathyroidectomy ïƒ Bone density increases.
- 36. m/c in 20 hyperparathyroidism. In 10 ïƒ phosphate retention with bone resorption Soft tissue calcification other than fibrocartilage and articular cartilage. Hyperparathyroidism (subperiosteal lesions)with impaired renal function amorphous calcium phosphate deposition in organs, blood vessels, soft tissues. (Hyperparathyroidism features with vascular and soft tissue calcifications).
- 37. Surgical removal of overactive parathyroid – in 10 Non surgical – ➢Annual monitoring of serum calcium and creatinine levels. ➢BMD monitoring every 1-2y. ➢10 - Calcimimetics. ➢20 - Dietary phosphate reduction, phosphate binders, vit D sterols and Calcimimetics ➢In refractory cases.
- 39. THANK YOU TOMORROW’S SEMINAR : Dr. Reshma Sri on Paget’s disease.