Induction of labour1.ppt
- 1. Induction of labour Dr Bellington Vwalika
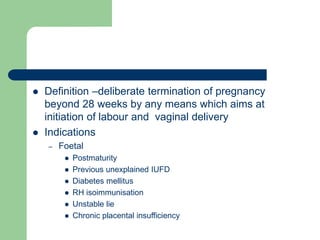
- 2.  Definition –deliberate termination of pregnancy beyond 28 weeks by any means which aims at initiation of labour and vaginal delivery  Indications – Foetal  Postmaturity  Previous unexplained IUFD  Diabetes mellitus  RH isoimmunisation  Unstable lie  Chronic placental insufficiency
- 3.  Maternal – IUFD – Chronic hydromnios with maternal distress – Congenital malformations  Combined (both mother and baby at risk) – PE and eclampsia – Lesser degree of placenta praevia – Placenta abruptio – PROM – Chronic hypertension – Chronic renal disease
- 4.  Contraindications – Contracted pelvis and CPD – Persitent malpresentation – Previuos C/S – High risk pregnancy with compromised foetus – Pelvic tumour – Elderly prigravida with complications
- 5.  Dangers – Maternal  Tendency for abnormal uterine action  Increased operative delivery  Increased morbidity  Psychlogical morbidity so when there is failure for which C/S is contemplated – Foetal  Iatrogenic prematurity  Hypoxia due to disordered uterine action and operative interference
- 6.  Success of induction depends on: – Period of gestation –uterus more sensitive near term – Favourable Bishop`s 7 and above – More easily successful in parous women than elderly primigravida and IUFD
- 7. Bishop`s pre-induction cervical scoring system Factors score 0 1 2 3 Dilat(cm) closed 1-2 3-4 5+ Efface(%) 0-30 40-50 60-70 80+ consist firm medium soft - position posterio midline anterior - station -3 -2 -1,0 +1,+2 Total score =13 favourable=6-13 unfavourable 0-5
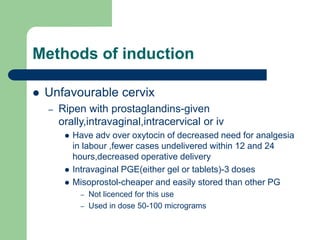
- 8. Methods of induction  Unfavourable cervix – Ripen with prostaglandins-given orally,intravaginal,intracervical or iv  Have adv over oxytocin of decreased need for analgesia in labour ,fewer cases undelivered within 12 and 24 hours,decreased operative delivery  Intravaginal PGE(either gel or tablets)-3 doses  Misoprostol-cheaper and easily stored than other PG – Not licenced for this use – Used in dose 50-100 micrograms
- 9. – Ripening with foleys catheter  Inflate with maximal fluid up to 60cc water ,wait for catheter to drop  Mechanism of action – Mechanical distension of cervix – Local release of prostaglandins – Stimulation of pituitary release of oxytocin (Ferguson`s reflex)
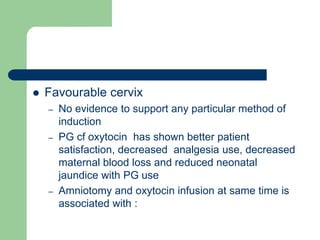
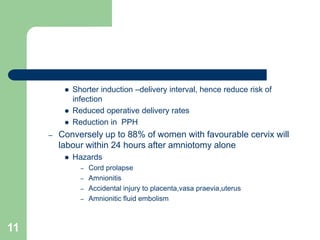
- 10.  Favourable cervix – No evidence to support any particular method of induction – PG cf oxytocin has shown better patient satisfaction, decreased analgesia use, decreased maternal blood loss and reduced neonatal jaundice with PG use – Amniotomy and oxytocin infusion at same time is associated with :
- 11. 11  Shorter induction –delivery interval, hence reduce risk of infection  Reduced operative delivery rates  Reduction in PPH – Conversely up to 88% of women with favourable cervix will labour within 24 hours after amniotomy alone  Hazards – Cord prolapse – Amnionitis – Accidental injury to placenta,vasa praevia,uterus – Amnionitic fluid embolism
- 12.  Oxytocin dosage –may be given by pump or infusion – Start at dose of 1-4 milliunits/min and increase ( titrated against contractions) up to a maximum of 32 mU/Min.Dose of oxytocin required to produce effective uterine contraction is 4-16 Mu/min – No benefit in using interval less than 3o minutes – Need for judicious use of fluid to avoid overload
- 13.  Other methods of ripening the cervix /induction- shown in trials – Membrane sweeppin/stripping-increases chance of delivery within a week – Relaxin – Antiprogestogen eg mifepristone – Nipple stimulation – Hygroscopic dilators eg laminaria – Use of bougies – No evidence that intercourse improves cervical ripeness
- 14. Merits and demerits of Oxytocin and PG use in medical induction oxytocin prostaglandins cheaper costly Widely available Selected centers Iv admnistration Intravaginal,orally,iv Uterine hyper activity stops when infusion stop Continues for variable time after stoppage Antidiuretic effect at high dose No such effect Less effective in-low bishop`s score,IUFD,low GA More effective in those cases