jaundice-new.ppt
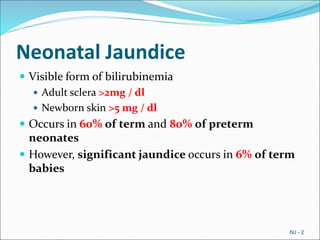
- 2. Neonatal Jaundice ï Visible form of bilirubinemia ï Adult sclera >2mg / dl ï Newborn skin >5 mg / dl ï Occurs in 60% of term and 80% of preterm neonates ï However, significant jaundice occurs in 6% of term babies NJ - 2
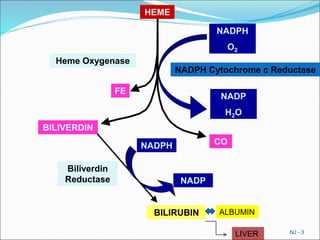
- 3. NJ - 3 HEME NADPH O2 NADPH Cytochrome c Reductase Heme Oxygenase NADP H2O FE BILIVERDIN Biliverdin Reductase BILIRUBIN CO NADPH NADP ALBUMIN LIVER
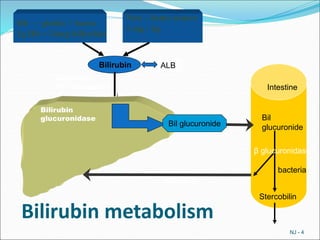
- 4. Bilirubin metabolism NJ - 4 Hb â globin + haem 1g Hb = 34mg bilirubin Non â heme source 1 mg / kg Bilirubin glucuronidase Bilirubin Bilirubin Ligandin (Y - acceptor) Bil glucuronide Intestine Bil glucuronide Stercobilin bacteria Îē glucuronidase ALB
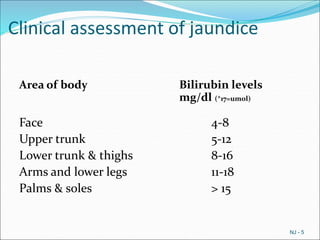
- 5. Clinical assessment of jaundice Area of body Bilirubin levels mg/dl (*17=umol) Face 4-8 Upper trunk 5-12 Lower trunk & thighs 8-16 Arms and lower legs 11-18 Palms & soles > 15 NJ - 5
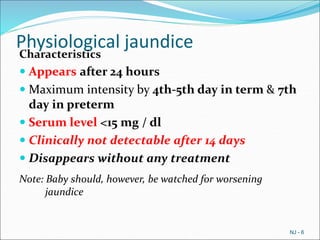
- 6. Physiological jaundice Characteristics ï Appears after 24 hours ï Maximum intensity by 4th-5th day in term & 7th day in preterm ï Serum level <15 mg / dl ï Clinically not detectable after 14 days ï Disappears without any treatment Note: Baby should, however, be watched for worsening jaundice NJ - 6
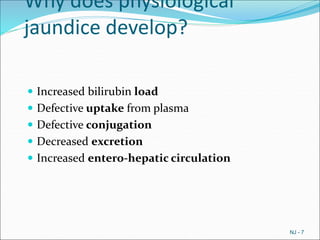
- 7. Why does physiological jaundice develop? ï Increased bilirubin load ï Defective uptake from plasma ï Defective conjugation ï Decreased excretion ï Increased entero-hepatic circulation NJ - 7
- 8. NJ - 8 Age in Days Term Preterm 1 2 3 4 5 6 10 11 12 13 14 15 10 5 Bilirubin level mg/dl Course of physiological jaundice
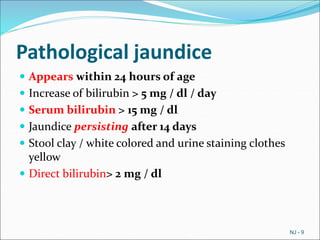
- 9. Pathological jaundice ï Appears within 24 hours of age ï Increase of bilirubin > 5 mg / dl / day ï Serum bilirubin > 15 mg / dl ï Jaundice persisting after 14 days ï Stool clay / white colored and urine staining clothes yellow ï Direct bilirubin> 2 mg / dl NJ - 9
- 10. Causes of jaundice Appearing within 24 hours of age ï Hemolytic disease of NB : Rh, ABO ï Infections: TORCH, malaria, bacterial ï G6PD deficiency Appearing between 24-72 hours of life ï Physiological ï Sepsis ï Polycythemia ï Concealed hemorrhage ï Intraventricular hemorrhage ï Increased entero-hepatic circulation NJ - 10
- 11. Causes of jaundice After 72 hours of age ï Sepsis ï Cephalhaematoma ï Neonatal hepatitis ï Extra-hepatic biliary atresia ï Breast milk jaundice ï Metabolic disorders NJ - 11
- 12. Risk factors for jaundice JAUNDICE ï J - jaundice within first 24 hrs of life ï A - a sibling who was jaundiced as neonate ï U - unrecognized hemolysis ï N â non-optimal sucking/nursing ï D - deficiency of G6PD ï I - infection ï C â cephalhematoma /bruising ï E - East Asian/North Indian NJ - 12
- 13. Common causes ï Exaggerated physiological ï Blood group incompatibility â ABO,Rh ï G6PD deficiency ï Bruising and cephalhaematoma ï Intrauterine and postnatal infections ï Breast milk jaundice NJ - 13
- 14. Approach to jaundiced baby ï Ascertain birth weight, gestation and postnatal age ï Ask when jaundice was first noticed ï Assess clinical condition (well or ill) ï Decide whether jaundice is physiological or pathological ï Look for evidence of kernicterus* in deeply jaundiced NB *Lethargy and poor feeding, poor or absent Moro's, opisthotonus or convulsions NJ - 14
- 15. Workup ï Maternal & perinatal history ï Physical examination ï Laboratory tests (must in all)* ï Total & direct bilirubin* ï Blood group and Rh for mother and baby* ï Hematocrit, retic count and peripheral smear* ï Sepsis screen ï Liver and thyroid function ï TORCH titers, liver scan when conjugated hyperbilirubinemia NJ - 15
- 16. Management ï Rationale: reduce level of serum bilirubin and prevent bilirubin toxicity ï Prevention of hyperbilirubinemia: early feeds, adequate hydration ï Reduction of bilirubin levels: phototherapy, exchange transfusion, drugs NJ - 16
- 17. Principle of phototherapy Native bilirubin Photo isomers of bilirubin Insoluble Soluble NJ - 17 450-460nm of light
- 18. Babies under phototherapy Baby under conventional phototherapy Baby under triple unit intense phototherapy
- 19. Phototherapy Technique ï Perform hand wash ï Place baby naked in cradle or incubator ï Fix eye shades ï Keep baby at least 45 cm from lights, if using closer monitor temperature of baby ï Start phototherapy NJ - 19
- 20. Phototherapy ï Frequent extra breast feeding every 2 hourly ï Turn baby after each feed ï Temperature record 2 to 4 hourly ï Weight record- daily ï Monitor urine frequency ï Monitor bilirubin level NJ - 20
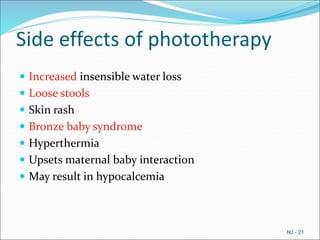
- 21. Side effects of phototherapy ï Increased insensible water loss ï Loose stools ï Skin rash ï Bronze baby syndrome ï Hyperthermia ï Upsets maternal baby interaction ï May result in hypocalcemia NJ - 21
- 22. Choice of blood for exchange blood transfusion ï ABO incompatibility ï Use O blood of same Rh type, ideal O cells suspended in AB plasma ï Rh isoimmunization ï Emergency 0 -ve blood Ideal 0 -ve suspended in AB plasma or baby's blood group but Rh -ve ï Other situations ï Baby's blood group NJ - 22
- 23. Hyperbilirubinemia 24 48 72 96 120 144 NJ - 24 420 400 380 360 340 320 300 280 260 240 220 200 180 160 140 120 100 80 60 40 20 V. IV. III. II. I.
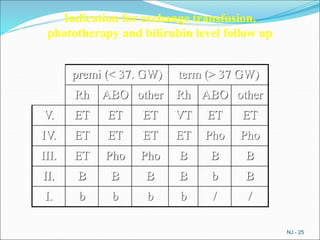
- 24. NJ - 25 premi (< 37. GW) term (> 37 GW) Rh ABO other Rh ABO other V. ET ET ET VT ET ET IV. ET ET ET ET Pho Pho III. ET Pho Pho B B B II. B B B B b B I. b b b b / / Indication for exchange transfusion, phototherapy and bilirubin level follow up
- 25. Prolonged indirect jaundice Causes ï Crigler Najjar syndrome ï Breast milk jaundice ï Hypothyroidism ï Pyloric stenosis ï Ongoing hemolysis, malaria NJ - 26
- 26. Conjugated hyperbilirubinemia Suspect ï High colored urine ï White or clay colored stool Caution ïAlways refer to hospital for investigations so that biliary atresia or metabolic disorders can be diagnosed and managed early NJ - 27
- 27. Conjugated hyperbilirubinemia Causes ï Idiopathic neonatal hepatitis ï Infections -Hepatitis B, TORCH, sepsis ï Biliary atresia, choledochal cyst ï Metabolic -Galactosemia, tyrosinemia, hypothyroidism ï Total parenteral nutrition NJ - 28