Kidney donation
- 1. Kidney Donation; Ethical issues, Selection & Exclusion criteria MOHAMED ELSAWY MD CANDIDATE ALEXANDRIA UNIVERSITY EMAIL: DR.SAWY@GMAIL.COM
- 2. Ethical issues in kidney transplantation ? Introduction: ? A central tent of medical ethics is to do good for the patient, although no physical good will accrue to the donner, it is accepted that the psychological benefits to the living donner justify the risk involved.
- 3. Ethical aspects of living donner: 1. Information and consent: Donner should be able to give his or her free consent to donation after understanding the information provided about the -The risk and benefits of organ donation -Alternative treatment available -The long term consensus of the decision Donner has the right to withdrawn at any time
- 4. 2. Safety: Many risks are associated with living donner nephrectomy, therefore good assessment of the donner health and psychological status to evaluate if the benefits outweigh the risk
- 5. 3. Financial gain: ? Offering or receiving money is considered legally unacceptable as it violates the principles of justice and equality
- 6. 4. DonnerˇŻs motivation: It is important to identify psychosocial apects to identify whether the donner motivation is altruist or not and to detect any kind of coercion
- 7. 5. DonnerˇŻs confidentiality DonnerˇŻs confidentiality must be protected and the evaluation must be carried out in the absence of recipient
- 8. 6. Unrelated donner: ? Living unrelated donner should only be accepted after the local ethical committee has given permission according to the rules of the country at which the donation is taking place
- 9. Deceased organ donner 1. Consent: ? Consent to be taken from patient or from relatives during life can be defining as opting in ? In some European countries the opposite situation applies, consent is presumed unless the patient has specifically opted out before death ( this type can increase organ donation)
- 10. 2. Allocation of deceased organ: ? In European system, distribution based on HLA matching , waiting time, matchability and sensitization and not on race, religion and wealth.
- 11. Kidney donation: Inclusion criteria (Eligibility criteria) ? Living donner eligibility criteria: ? Must be 19 years and above as age is not a limiting factor in kidney donation. ? Medically suitable to donate. ? Psychologically stable. ? Capable of giving informed consent.
- 12. ? Deceased kidney eligibility criteria: ? A diagnosis of brain death is required in comatose subject who may potentially be a deceased organ donner.
- 13. Exclusion criteria ( contraindicated donner) Absolute contraindications ˇńBoth age <18 years and mentally incapable of making an informed decision. ˇńUncontrolled hypertension or history of hypertension with end-organ damage. ˇńHIV infection, unless the requirements for a variance are met, including institutional review board (IRB) approval consistent with research criteria. ˇńDiabetes mellitus. ˇńBlood type incompatibility.
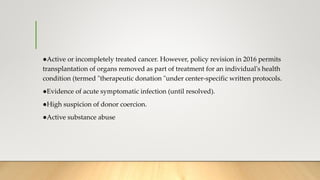
- 14. ˇńActive or incompletely treated cancer. However, policy revision in 2016 permits transplantation of organs removed as part of treatment for an individual's health condition (termed "therapeutic donation "under center-specific written protocols. ˇńEvidence of acute symptomatic infection (until resolved). ˇńHigh suspicion of donor coercion. ˇńActive substance abuse
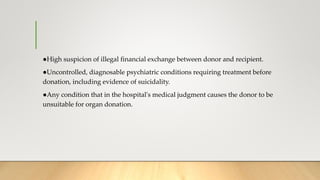
- 15. ˇńHigh suspicion of illegal financial exchange between donor and recipient. ˇńUncontrolled, diagnosable psychiatric conditions requiring treatment before donation, including evidence of suicidality. ˇńAny condition that in the hospital's medical judgment causes the donor to be unsuitable for organ donation.
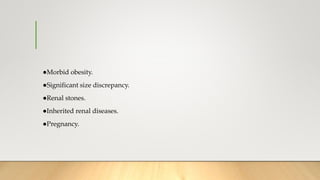
- 16. ˇńMorbid obesity. ˇńSignificant size discrepancy. ˇńRenal stones. ˇńInherited renal diseases. ˇńPregnancy.
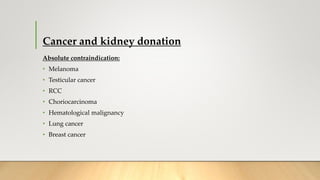
- 17. Cancer and kidney donation Absolute contraindication: ? Melanoma ? Testicular cancer ? RCC ? Choriocarcinoma ? Hematological malignancy ? Lung cancer ? Breast cancer
- 18. Special exception for infection: HCV positive donner ? In HCV positive recipient, transplant is allowed following informed consent. ? In HCV negative recipient, there is a high risk of disease transmission, howver it is possible in emergency situation following consent.
- 19. ? HBsAg positive donner -HBV-infected organ donors may be a relevant organ source for kidney transplantation. Kidneys from HBcAb-positive organ donors may be transplanted safely in successfully vaccinated or in HBsAg-positive patients with an anti-HBs titer >10 IU/L; these organ could be allocated even to HBsAb-negative recipients with a very low risk of transmission. In these patients, an antiviral prophylaxis with lamivudine or, alternatively, with entecavir, may be warranted. -Kidney transplantation from HBsAg-positive donor kidneys may be safely allocated in HBsAg-positive recipients. All transplant recipients should undergo antiviral prophylaxis. -Kidney transplantation in HBsAb-positive recipients with an anti-HBs titer of at least >10 IU/L could be performed safely with post-transplant HBV monitoring and, eventually, with the use of antivirals to prevent the risk of hepatitis B progression -Kidney transplantation from HBsAg-positive donors to HBV-na?ve recipients, although some promising results have been reported, needs further data to be extensively adopted, and should be limited to urgent life-threatening conditions.
- 20. Cancer and kidney donation Possible donation: Treated cancers with high probability of cure after 5-10 years eg ? Colon cancer ? Nonmelanoma skin cancer ? CIS of cervix and vulva
- 21. Relative contraindication: ? Age above 65. ? Controlled hypertension. ? Impaired glucose tolerance. ? Obesity. ? Borderline renal function. ? Microscopic haematuria. ? Single renal stones.
- 22. Thanks