Knee joint examination
- 1. Knee Joint examination Ahmed Ghoname
- 2. Objectives • General rules • Components of joint examination • Closure of the station
- 3. C L I N I C A L D A Y General rules • Wash hands • Introduce yourself • Confirm patient details – name / DOB • Explain examination: “Today I need to examine your knee joint, this will involve looking, feeling and moving the joint.” • Check understanding and gain consent: “Does everything I’ve said make sense? Are you happy for me to examine your knee joint?” • Expose patient’s legs – ideally the patient should be wearing shorts • Position the patient standing upright • Ask if patient currently has any pain
- 4. C L I N I C A L D A Y Components of joint examination • Look (inspection) • Feel (palpation) • Move: – Active movements – Passive movements – Grading muscular power • Special tests • Neurovascular assessment
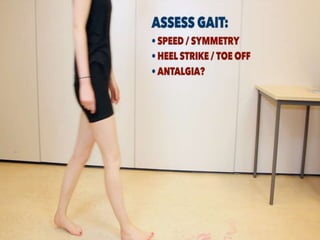
- 7. C L I N I C A L D A Y Look(inspection) • Gait • Is the patient demonstrating a normal heel strike / toe off gait? • Is each step of normal height? – increased stepping height is noted in foot drop • Is the gait smooth and symmetrical? • Any obvious abnormalities? – antalgia / waddling / broad based
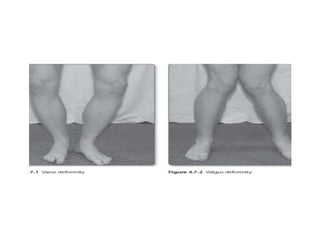
- 10. C L I N I C A L D A Y Look(inspection) • Anteriorly • Scars – previous surgery / trauma • Swellings – effusions / inflammatory arthropathy / septic arthritis / gout • Asymmetry / leg length discrepancy • Valgus or varus deformity • Quadriceps wasting – suggests chronic inflammation / reduced mobility
- 11. C L I N I C A L D A Y Look(inspection) • Posteriorly • Scars • Asymmetry • Popliteal swellings – Baker’s cyst / Popliteal aneurysm
- 13. C L I N I C A L D A Y Feel(palpation) • Ask the patient to lay on the bed. • Assess temperature – ↑ temperature may suggest inflammation / infection • Palpate the quadriceps tendon – whilst leg extended – tenderness suggests synovitis
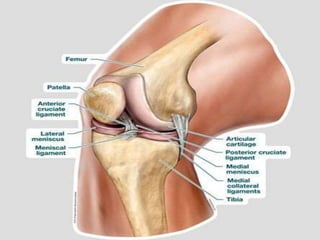
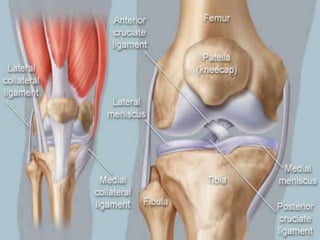
- 14. C L I N I C A L D A Y Feel(palpation) • Palpate the following with the knee flexed at 90°: • Patella – palpate the borders for tenderness / effusion • Tibial tuberosity – tenderness may suggest Osgood Schlatter disease • Head of the fibula – irregularities / tenderness • Tibial and femoral joint lines – irregularities / tenderness • Collateral ligaments – both medial and lateral • Popliteal fossa – feel for any obvious collection of fluid (e.g. a Baker’s cyst)
- 20. C L I N I C A L D A Y Measure quadriceps circumference and compare – 20cm above tibial tuberosity
- 21. C L I N I C A L D A Y • Patellar tap (can detect larger effusions) • 1. Empty the suprapatellar pouch by sliding your left hand down the thigh to the patella. • 2. Keep your left hand in position and use your right hand to press downwards on the patella with your fingertips. • 3. If fluid is present you will feel a distinct tap as the patella bumps against the femur
- 23. C L I N I C A L D A Y • Sweep test (useful for detecting small effusions) • 1. Empty the suprapatellar pouch with one hand whilst also emptying the medial side of the joint using an upwards wiping motion. • 2. Now release your hands and do a similar wiping motion downwards on the lateral side of the joint. • 3. Watch for a bulge or ripple on the medial side of the joint. • 4. The appearance of a bulge or ripple on the medial side of the joint suggests the presence of an effusion.
- 25. C L I N I C A L D A Y Movement • Active • This involves the patient performing the movement. Ensure you observe for restricted range of movement and signs of discomfort. • Knee flexion – normal ROM 0-140º – “Move your heel as close to your bottom as you can manage” • Knee extension – “Straighten your leg out as best as you are able to.”
- 26. C L I N I C A L D A Y • Passive • This involves the patient relaxing and allowing you to move the joint freely. It’s important to feel for crepitus as you move the joint and observe any restriction of movement. • Knee flexion and extension • Hyperextension – elevate both legs by the heels – note any hyperextension (<10º is normal)
- 28. C L I N I C A L D A Y Special test • Anterior/Posterior drawer test • Collateral ligaments • Lateral collateral ligament (LCL) • Medial collateral ligament (MCL) • Lachman’s test: ACL • McMurray’s test • Patellar apprehension test • Apley’s test
- 35. C L I N I C A L D A Y Neurovascular assessment • Palpation of pulses • Detailed examination of each nerve, and its sensory and motor component • A quick screening examination of the joint above and below should also be performed if time permits
- 36. C L I N I C A L D A Y Diagnoses to consider • Traumatic diagnoses include collateral or cruciate ligament injuries, fractures and meniscus tears. • Non-traumatic diagnoses include osteoarthritis, septic arthritis, internal derangement of the knee, baker’s cyst and referred hip pain
- 37. C L I N I C A L D A Y Closing the examination • Make sure you leave the patient comfortable • Help them redress if necessary • Thank them • Wash hands
- 39. C L I N I C A L D A Y Summary • General rules • Inspection • Palpation • Movement • Special tests • Neurovascular assessment • Closure
Editor's Notes
- #29: Lachman’s test: this is more specific for ACL integrity. With one hand grasp the femur just above the knee and with the other grasp the tibia just below the knee, keeping the knee in 20° flexion. Attempt lift the tibia forwards. One should be able to feel a definite end to movement indicating an intact ACL. Any excessive movement is abnormal. McMurray’s test: start with the knee in full flexion. Place the examiner’s hand on the patella the fingers palpating the joint line. For the medial meniscus, externally rotate the foot and apply valgus strain to the knee. Now gently extend the knee feeling for any clicks or noting pain as the knee is extended. For the lateral meniscus, internally rotate the foot and apply varus strain to the knee extending it at the same time Patellar apprehension test: hold the leg with the knee in full extension. Gently flex the knee applying pressure on the medial aspect of the patella attempting to displace it laterally. The patient will feel the sensation of dislocation and will stop the examiner progressing with the test. Medial and lateral collateral ligaments: apply varus and valgus stress with the knee in full extension and in 20° of flexion (this relaxes the cruciate ligaments and the knee capsule). It is easier to perform with the lower leg held in examiner’s axilla and the hands on either side of the knee. From this position, the examiner can provide varus or valgus strain feeling for any abnormal mobility. There is some movement in flexion as the rest of the knee ligaments are relaxed and purely collaterals are tested, whereas any movement in full extension is abnormal (Figure 4.7.5). •• Cruciate ligaments drawer test: keep the knees flexed at approximately 90°and the feet pointing forwards. Note any sagging of the tibial condyle as compared to the other side (Figure 4.7.6). This could mean a ruptured posterior cruciate ligament (PCL). Next the examiner stabilises the patient’s legs by sitting close to, or gently on top of, the patient’s feet (this manoeuvre braces the feet against the examiner so the following step can be performed). If both the tibial condyles are at the same level, grasp the leg firmly with fingers in the popliteal fossa and thumbs on the tibial tubercle. Check that the hamstrings are relaxed and attempt to move the leg forwards with a firm jerk (Figure 4.7.7). Any excessive movement suggests a ruptured anterior cruciate ligament (ACL).