Kub - xray and usg
- 2. Kidneys a. Retroperitoneal b. 10 – 15 cm in length (xray); Left > Right c. 3 and ½ lumbar vertebrae d. Hilum at L1 vertebral level; Ant to Post: VAP e. Functional unit : Nephron
- 4.  Relations a. Posteriorly: Diaphragm, 12th Rib, Pleura, med – lat: Psoas, QL, TA b. Superiorly: Adrenals c. Anteriorly: Right: Liver, Duod 2nd, Asc colon, SI. Left: Stomach, Pancreas, Spleen, SF, Jejunum
- 6.  Capsules a. Fibrous capsule: surrounds kidney b. Renal fascia of Gerota (ant) and Zuckerkandl (post): Fuse Laterally as lateral Conal Fascia
- 7.  Coronal Cross Section
- 10.  Developmental anomalies 1. Duplication of collecting system – commonest (4%) 2. Persistant fetal lobulation 3. Accessory arteries
- 12. 4. Horse shoe Kidney
- 13. 5. Persistent Pelvic Kidney
- 14. 6. Crossed fused ectopia
- 17.  Blood supply Renal arteries from Aorta at L1/L2 level. Right renal artery > Left; posterior to IVC Left renal vein > Right; anterior to Aorta
- 18. Large left renal pelvic calculus with deviation of left ureter
- 19. Ultrasound  Kidney size smaller than on radiographs – 9-12 cm  Visualization: Posterolateral, Lateral or Posterior approach
- 20. Junctional cortical/ parenchymal defects: triangular echogenic areas In upper pole. Represent normal extensions of renal sinus due to partial fusion of embryonic renunculi. DD: Renal Scar, Angiomyolipoma
- 21. Hypertrophied Column of Bertin: Partial renal duplication of septal cortex in mid portion of kidney – pseudomass appearance Associated with bifid pelvis
- 22. Uncomplicated renal cyst • well-marginated anechoic lesion with thin walls • a few thin septa (5% of cysts) • the back wall should be visible • posterior acoustic enhancement - nonspecific • a small amount of intracystic hemorrhage/deb ris may be present, and may require further evaluation
- 23. Complicated renal cyst • ​cystic lesions with thickened or irregular walls or septa are suspicious for renal cell carcinoma and warrant further work up • vascularity of the septa on color or spectral Doppler is suspicious for renal cell carcinoma
- 24. Calculus in lower pole • echogenic foci • acoustic shadowing • twinkle artefact on colour Doppler • colour comet-tail artefact
- 25. Hydronephrosis
- 26. Chronic kidney disease Grade 1 Grade 2 Grade 3
- 27. Pyelonephritis  particulate matter/debris in the collecting system  reduced areas of cortical vascularity by using power Doppler  gas bubbles (emphysematous pyelonephritis)  abnormal echogenicity of the renal parenchyma 1  focal/segmental hypoechoic regions (in oedema) or hyperechoic regions (in haemorrhage)  mass-like change
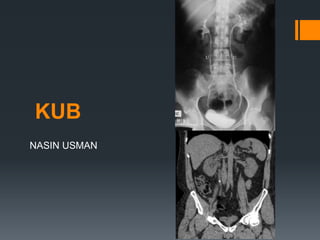
- 28. CT KUB  Slices T12 to L3  Renal substance: homogenous in unenhanced CT [HU - 30-50]  After IV contrast: a. Arterial corticomedullary: after 25 – 70 sec b. Venous Nephrographic: 80 – 180 sec (contrast homogenous) c. Excretory phase: after 180 sec (contrast in collecting system) Arteries in first 25 secs; Veins after 60 secs
- 29.  Findings  identification of calcified renal tract calculi size and position  stone composition assessment with dual energy CT  assessment of the sequelae of calculi  obstruction  infection  assessment of other causes of flank pain if negative for calculus disease  presence of further calculi at risk of obstructing
- 30. Staghorn calculus with enlarged left kidney
- 32. Pyelonephritis with subcapsular collection
- 33. Ureters  25 – 30 cm long; diameter of 3mm  Narrower at following sites: • Junction of pelvis and ureter • Pelvic brim • Intravesical ureter
- 34.  Relations:  Abdominal ureter  Following the course of the ureter from superior to inferior:  posteriorly: psoas muscle; genitofemoral nerve; common iliac vessels; tips of L2-L5 transverse processes  anteriorly  Right ureter: descending duodenum, gonadal vessels; right colic vessels; ileocolic vessels  left ureter: gonadal artery; left colic artery; loops of jejunum; sigmoid mesentery and colon  medially  right ureter: IVC  left ureter: abdominal aorta, inferior mesenteric vein
- 36.  Pelvic ureter • posteriorly: sacroiliac joint, internal iliac artery • inferiorly • male: seminal vesicle • female: lateral fornix of the vagina • anteriorly • male: ductus deferens • female: uterine artery (in the broad ligament) • medially • female: cervix
- 37.  Development a. Blind diverticulum from the metanephric duct  Developmental anomalies a. Duplication: commonest significant congenital anomaly of urinary tract. Commoner in females. b. Weigert-Meyer law: during complete duplication, ureter serving the upper renal moiety drains fewer calyces and is inserted lower into the bladder than that draining the lower moiety – maybe as low as the bladder neck Upper moiety – obstruction Lower moiety – reflux
- 38. Ectopic ureter
- 39. Left ureterocele
- 40.  IVU: oProne views aid filling oDistension of proximal part by compression band across abdomen oOblique views for UV junction  Ultrasound: oProx and distal visible when well distended.  CT: oReplaced IVU as IOC for ureteric calculi
- 41. Bladder  pyramidal muscular organ when empty  It has a triangular shaped base posteriorly  The ureters enter the postero- lateral angles and the urethra leaves inferiorly at the narrow neck , which is surrounded by the (involuntary) internal urethral sphincter  Extraperitoneal – only superiorly covered  The ability of the full bladder to elevate and displace bowel loops is taken advantage of in pelvic ultrasound, where the full bladder provides an acoustic window
- 42. median ligament is the fibrous remnant of the urachus medial ligaments are the fibrous remnants of the umbilical arteries
- 43.  Relations:  male a. anteriorly: pubic symphysis b. posteriorly: rectovesical pouch and rectum c. inferiorly: prostate, obturator internus muscle, levator ani muscle d. superiorly: peritoneum e. laterally: ischioanal fossa  female a. anteriorly: pubic symphysis b. posteriorly: vesicouterine pouch, uterus, cervix, vagina c. inferiorly: pelvic fascia, perineal membrane d. superiorly: uterus, peritoneum e. laterally: ischioanal fossa
- 44. Male
- 45. MRI female
- 46.  Bladder is relatively fixed inferiorly via a. condensations of pelvic fascia, which attach it to the back of the pubis, the lateral walls of the pelvis and the rectum b. continuity with the prostate in male - strong puboprostatic ligaments Bladder rupture - # pelvis - Blunt injury abd
- 47.  Development:  Trigone from mesoderm  Ventral bladder wall endodermal from urogenital sinus Double bladder
- 48. Wall thickness 3-5 mm
- 49. Bladder calculi
- 50. UB mass
- 51. Hyperdense lesion in right lateral wall
- 52. Right VUJ calculus Normal bladder - < 10HU
- 53. Intraperitoneal bladder rupture with extravasation of contrast
- 54. Prostate  shaped like an upside-down truncated cone and surrounds the base of the bladder and the proximal (prostatic) urethra, extending inferiorly to the urogenital diaphragm and external sphincter.  weighs between 20-40 grams with an average size of 3 x 4 x 2 cm  70% glandular tissue and 30% fibromuscular or stromal tissue  seminal vesicles are superior and posterior to the prostate gland. Its ejaculatory ducts pierce the posterior surface of the prostate below the bladder
- 56. 3 zones: - Peripheral (70%) - Central (25%) - Transition (5%)
- 57. Prostatic calcification in Prostate cancers with bony mets
- 58.  Transabdominal Ultrasound can assess the volume of the prostate but is not reliable to diagnose carcinoma  fill their bladder with at least 60ml of fluid  probe is angled approximately 30 degrees caudal using the bladder as a window
- 59. BPH  increase in volume of the prostate with a calculated volume exceeding 30 mL (width x height x length x 0.52)  central gland is enlarged, and is hypoechoic or of mixed echogenicity  calcification may be seen both within the enlarged gland as well as in the pseudocapsule (representing compressed peripheral zone)  PVR
- 60. BPH CT KUB  central zone appears hyperdense between 40-60 HU  peripheral zone appears hypodense between 10-25 HU  useful staging metastatic spread
- 61. Prostate CA In advanced disease, CT scan is the test of choice to detect enlarged pelvic and retroperitoneal lymph nodes, hydronephrosis and osteoblastic metastases


























![CT KUB
 Slices T12 to L3
 Renal substance: homogenous in unenhanced CT [HU - 30-50]
 After IV contrast:
a. Arterial corticomedullary: after 25 – 70 sec
b. Venous Nephrographic: 80 – 180 sec (contrast homogenous)
c. Excretory phase: after 180 sec (contrast in collecting system)
Arteries in first 25 secs; Veins after 60 secs](https://image.slidesharecdn.com/kub-180219162116/85/Kub-xray-and-usg-28-320.jpg)