Lymphoid Proliferations.pptx
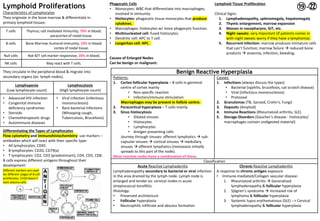
- 1. Lymphoid Proliferations Characteristics of Lymphocytes They originate in the bone marrow & differentiate in primary lymphoid tissues: They circulate in the peripheral blood & migrate into secondary organs (ex: lymph nodes). Differentiating the Types of Lymphocytes Flow cytometry and immunohistochemistry: use markers ŌĆō antibodies which will react with their specific type: ŌĆó All lymphocytes: CD45 ŌĆó B lymphocytes: CD20, CD79(a) ŌĆó T lymphocytes: CD2, CD3 (predominant), CD4, CD5, CD8. B cells express different antigens throughout their development: Phagocytic Cells ŌĆó Monocytes: WBC that differentiate into macrophages, involved in immunity. ŌĆó Histiocytes: phagocytic tissue monocytes that produce cytokines. ŌĆó Macrophages: histiocytes w/ more phagocytic function. ŌĆó Multinucleated cell: fused histiocytes. ŌĆó Dendritic cell: APC to T cell. ŌĆó Langerhan cell: APC. Causes of Enlarged Nodes Can be benign or malignant: Lymphoid Tissue Proliferation Clinical Signs: 1. Lymphadenopathy, splenomegaly, hepatomegaly 2. Thymic enlargement, marrow expansion 3. Masses in nasopharynx, GIT, etc. 4. Night sweats: very important (if patients comes in with night sweats worry if they have a lymphoma). 5. Recurrent infection: marrow produces immature cells that canŌĆÖt function; marrow failure ’āĀ reduced bone products ’āĀ anaemia, infection, bleeding. T cells Thymus; cell mediated immunity; 70% in blood; paracortex of nodal tissue. B cells Bone Marrow; humoral immunity; 10% in blood; cortex of nodal tissue. Null cells Not B/T cell marker responsive; 20% in blood; NK cells May react with T cells. Lymphopenia (Low lymphocyte count) Lymphocytosis (High lymphocyte count) ŌĆó Advanced HIV infection ŌĆó Congenital immune deficiency syndromes ŌĆó Steroids ŌĆó Chemotherapeutic drugs ŌĆó Autoimmune diseases ŌĆó Viral infection (infectious mononucleosis) ŌĆó Rare bacterial infections (Whooping cough, Tuberculosis, Brucellosis) Benign Reactive Hyperplasia Patterns: 1. Cortex follicular hyperplasia ŌĆō B cells in germinal centre of cortex mainly ŌĆó Non-specific reaction ŌĆó Infection/immune stimulation Macrophages may be present in follicle centre. 2. Paracortical hyperplasia ŌĆō T cells mainly 3. Sinus histiocytosis ŌĆó Dilated sinuses ŌĆó Histiocytes ŌĆó Lymphocytes ŌĆó Antigen presenting cells Journey through sinuses: afferent lymphatics ’āĀ sub- capsular sinuses ’āĀ cortical sinuses ’āĀ medullary sinuses ’āĀ efferent lymphatics (metastasis initially spreads to this part of the node). Most reactive nodes have a combination of these. Causes: 1. Infections (always discuss the types) ŌĆó Bacterial (syphilis, brucellosis, cat scratch disease) ŌĆó Viral (infectious mononucleosis) ŌĆó Protozoal 2. Granulomas (TB, Sarcoid, CrohnŌĆÖs, Fungi) 3. Deposits (Amyloid) 4. Immune Reactions (Rheumatoid arthritis, SLE) 5. Storage Disorders (GaucherŌĆÖs disease - histiocytes/ macrophages contain undigested material) Classification Acute Reactive Lymphadenitis Lymphadenopathy secondary to bacterial or viral infection in the area drained by the lymph node. Lymph node is enlarged and tender ex: cervical nodes in acute streptococcal tonsillitis. Histology: ŌĆó Preserved architecture ŌĆó Follicular hyperplasia ŌĆó Neutrophilic infiltrate and abscess formation Chronic Reactive Lymphadenitis A response to chronic antigen exposure ŌĆó Immune-mediated/Collagen vascular disease: 1. Rheumatoid arthritis ’āĀ Generalised lymphadenopathy & follicular hyperplasia 2. Sj├ČgrenŌĆÖs syndrome ’āĀ Increased risk of lymphoma & follicular hyperplasia 3. Systemic lupus erythematosus (SLE) --> Cervical lymphadenopathy & follicular hyperplasia Different markers are used for different stages of B cell proliferates; CD20 doesnŌĆÖt stain plasma cells Ōæ▓-ŃēÆ
- 2. Investigation of an Enlarged Lymph Node Diagnostic Questions: ’ü▒ Is the node benign or malignant? ’ü▒ If benign is there an identifiable cause for node enlargement? ’ü▒ If malignant is it a carcinoma, lymphoma (most likely), melanoma or sarcoma? ’ü▒ If it is a metastatic carcinoma, where is the primary site? 1. Proper history and clinical examination. Ask: ’ü▒ Evidence of recent infection? ’ü▒ Evidence of malignancy in adjacent lymphatic draining site? ’ü▒ Any localising symptoms? ’ü▒ Any weight loss? ’ü▒ Any night sweats? ’ü▒ Duration of lymphadenopathy? ’ü▒ Are nodes sore/tender? 3. Investigations: ŌĆó FBC ŌĆó CRP (C-reactive Protein) ’āĀ indicates inflammation ŌĆó LDH ’āĀ indicates RBC lysis ŌĆó Viral screen ŌĆó Chest X-ray ŌĆó CT chest and abdomen ŌĆó Biopsy (to investigate histology) 1. Fine needle aspiration/biopsy 2. Incisional biopsy 3. Excision of whole node ’āĀ ensures that malignant portion is not missed & is thus the best sample. 4. Bone marrow trephine NB: enlarged retroperitoneal nodes present because theyŌĆÖre in the abdomen and need to be very large to be felt. Malignant (Lymph Node Enlargement) Causes: Primary: ŌĆó Lymphoma ŌĆó Leukaemia Secondary: ŌĆó Metastatic carcinoma ŌĆō commonest ŌĆó Metastatic melanoma ŌĆó Metastatic sarcoma ŌĆō rare ŌĆó Others i.e. Germ cell ŌĆō rare To investigate likely primary site of a metastasis in a node: ŌĆó Suspect the area which drains that node: Examples: 1. Metastasis in inguinal node ’āĀ due to melanoma of skin of lower limb (not squamous cell carcinoma because it rarely metastasises) 2. Metastasis in supraclavicular node ’āĀ upper GIT carcinoma, bronchogenic carcinoma, breast 3. Metastasis in cervical node ’āĀ nasopharyngeal carcinoma, oropharyngeal carcinoma, head and neck carcinoma, salivary glands, thyroid. 4. Metastasis in axillary node ’āĀ breast carcinoma 5. Melanoma ’āĀ check anal skin and retina for primary site. Histological features that identify type of malignancy: Morphological features that suggest a carcinoma: ŌĆó Keratin ŌĆōSquamous cell carcinoma ŌĆó Mucin ŌĆōAdenocarcinoma ŌĆó Tubules ŌĆōAdenocarcinoma If morphological features are not evident, we use tumour markers: ŌĆó Cytokeratin ŌĆōCK ŌĆō Epithelial ŌĆōMetastatic Carcinoma ŌĆó Vimentin ŌĆō Mesenchymal ŌĆó CD45 ŌĆō Common Leucocyte Antigen ŌĆō Lymphoma ŌĆó S100P and HMB45 ŌĆō Melanoma o If an undifferentiated malignancy in a lymph node is CD45 (Common Leucocyte antigen) positive, then diagnosis is of a LYMPHOMA. o If an undifferentiated neoplasm is Cytokeratin (CK) positive it is a metastatic carcinoma.
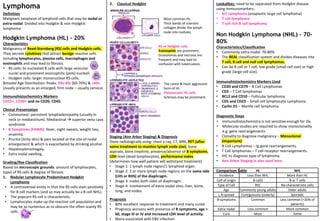
- 3. Lymphoma Definition Malignant neoplasm of lymphoid cells that may be nodal or extra-nodal. Divided into Hodgkin & non-Hodgkin lymphoma. Hodgkin Lymphoma (HL) ŌĆō 20% Characteristics Malignancy of Reed-Sternberg (RS) cells and Hodgkin cells. They secrete cytokines that attract benign reactive cells including lymphocytes, plasma cells, macrophages and eosinophils and may lead to fibrosis. ŌĆó RS cells: bi-nucleated B cells with large vesicular nuclei and prominent eosinophilic (pink) nucleoli. ŌĆó Hodgkin cells: larger mononuclear RS cells. Bimodal Age Distribution: Peaks: 20s-30s (60-70%) & >60s. Usually presents as an enlarged, firm node ŌĆō usually cervical. Immunohistochemistry Markers CD15+, CD30+ and no CD20, CD45. Clinical Presentation ŌĆó Commonest: persistent lymphadenopathy (usually in neck or mediastinum). Mediastinal ’āĀ superior vena cava syndrome. ŌĆó B Symptoms (FAWN): fever, night sweats, weight loss, anaemia. ŌĆó Pruritis (itchy skin) & pain located at the site of nodal enlargement & which is exacerbated by drinking alcohol. ŌĆó Hepatosplenomegaly. ŌĆó Extra nodal swelling. Grading/Rye Classification Based on microscopic grounds: amount of lymphocytes, types of RS cells & degree of fibrosis: 1. Nodular Lymphocyte Predominant Hodgkin Lymphoma ŌĆó A controversial entity in that the RS cells stain positively for B cell markers (and so may actually be a B cell NHL). ŌĆó The popcorn RS cell is characteristic. ŌĆó Lymphocytes make up the reactive cell population and may be so numerous as to obscure the often scanty RS cells. 2. Classical Hodgkin Staging (Ann Arbor Staging) & Diagnosis Done radiologically using: chest x-ray, CT, MRI, PET (after some treatment to monitor lymph node size), bone aspirate, bone trephine, presence/absence of B symptoms, LDH level (dead lymphocytes), performance index (determines how well patient will withstand treatment) ŌĆó Stage 1: 1 lymph node region/1 lymphoid organ. ŌĆó Stage 2: 2 or more lymph node regions on the same side (LHS or RHS) of the diaphragm. ŌĆó Stage 3: nodes both sides of diaphragm. ŌĆó Stage 4: involvement of extra-nodal sites: liver, bone, lung, and nodes. Prognosis ŌĆó 80% excellent response to treatment and many cured. ŌĆó Prognosis worsens with presence of B symptoms, age > 60, stage III or IV and increased LDH level of activity. ŌĆó Many associated with EBV infection. Lookalikes: need to be separated from Hodgkin disease using Immunomarkers: ŌĆó Ki1 Lymphoma (anaplastic large cell lymphoma) ŌĆó T cell lymphoma ŌĆó T cell rich B cell lymphoma Non Hodgkin Lymphoma (NHL) ŌĆō 70- 80% Characteristics/Classification ŌĆó Commonly extra-nodal: 70-80% ŌĆó The REAL classification system and divides diseases into T cell, B cell and null cell lymphomas. ŌĆó Can be B cell or T cell, low grade (small cell size) or high grade (large cell size). Immunohistochemistry Markers Used ŌĆó CD20 and CD79 ŌĆō B Cell Lymphomas ŌĆó CD3 ŌĆō T Cell lymphomas ŌĆó BCL2 and CD10 ŌĆō Follicular lymphoma ŌĆó CD5 and CD23 ŌĆō Small cell lymphocytic Lymphoma ŌĆó Cyclin D1 ŌĆō Mantle cell lymphoma Diagnostic Steps ŌĆó Immunohistochemistry is not sensitive enough for Dx. ŌĆó Molecular studies are required to show monoclonality e.g. gene rearrangements. ŌĆó Clonality to diagnose malignancy ŌĆō Monoclonal (important) ŌĆó B Cell Lymphomas ŌĆō Ig gene rearrangements. ŌĆó T Cell lymphomas ŌĆō T cell receptor rearrangements. ŌĆó IHC to diagnose type of lymphoma. ŌĆó Ann Arbor Staging is also used here. Comparison Table Most common HL. Thick bands of sclerotic collagen divide the lymph node into nodules. RS or Hodgkin cells. Eosinophils are prominent. Granulomas and necrosis are frequent and may lead to confusion with tuberculosis. The rarest & most aggressive form of HL. Pleomorphic RS cells. Sclerosis may be prominent. HL NHL Incidence Less than NHL More than HL Cell of origin B-cells B or T cells Type of Cell RSC No characteristic cells Age Commonly young adults Older adults L.N spread Contiguously (orderly) Sporadic B-symptoms Common Less common (>20% of patients) Extra-nodal Less common More common Cure Most Some
- 4. Non-Hodgkin Lymphoma (NHL) contŌĆÖd B cell NH-Lymphomas: B Cell Lymphoma Cell of Origin & Markers Pathogenesis & Presentation Epidemiology & Prognostics Follicular B Cell Lymphoma Centrocyte/ Centroblast BCL2 & CD10. Definition: Small neoplastic B cells form follicle-like nodules. Cause: t(14;18) BCL2. Pathogenesis: Antiapoptotic BCL2 gene on chromosome 18 translocated to chromosome 14 ’āĀ overexpression of anti-apoptotic proteins ’āĀ B cell proliferation. NB: Follicular Lymphoma is BCL2 positive, monoclonal, destroys lymph node architecture and doesnŌĆÖt have tingible body macrophages where as reactive follicular hyperplasia is the opposite. One of the commonest lymphomas: ŌĆó Affects >50 years ŌĆó 60% stage III or IV at presentation. ŌĆó Rarely get cured but indolent (not aggressive) and progressive disease. ŌĆó 70% - 5 year survival. ŌĆó 20% - transform to high grade. Small Cell Lymphocytic Lymphoma Lymphocyte CD5 & CD23 Definition: Chronic lymphocytic leukaemia that has spread to/manifested in the tissues. Presentation: Widespread adenopathy, Splenomegaly, decreased Ig ’āĀ increased infection ŌĆó 5-10% RichterŌĆÖs Syndrome ŌĆō high grade transformation (cells become big) ŌĆó Commonly stage III or IV because asymptomatic at presentation. Mantle Cell Lymphoma Mantle cells Cyclin D1 Definition: diffuse replacement of node by malignant/neoplastic mantle B-cells. Cause: t(11;14) Cyclin D1. Pathogenesis: Cyclin D1 gene on chromosome 11 translocated to chromosome 14 ’āĀ inc. cyclin D1 ’āĀ more cells enter G1/S phase ’āĀ increased proliferation. <5% of all lymphomas (rarer): ŌĆó Age distribution: peak 60-70 years. ŌĆó Often high stage at presentation . ŌĆó 20-40% - 5 year survival. Marginal Zone Lymphoma (ex: Maltoma ŌĆō GIT) Marginal zone cells Definition: Extra-nodal lymphomas that are usually low grade. Predisposing Factors: Antigen Challenge. Pathogenesis: associated with and found in chronic inflammatory conditions: GIT ŌĆōHLO in stomach, Thyroid ŌĆōHashimotoŌĆÖs, Salivary gland ŌĆōSjogrenŌĆÖs, Lungs Due to increased cell turnover precipitated by the underlying condition Diffuse Large Cell B Cell Lymphoma Centroblasts Definition: Large mononuclear neoplastic B cells proliferate and can spread to extra-nodal sites. Commonest high grade B cell lymphoma: ŌĆó Aggressive but curable. Lymphoblastic B Cell Lymphoma Lymphoblast Rare (Majority are T cell LBLs); Bone lytic lesions. ŌĆó Many children and young adults BurkittŌĆÖs Lymphoma Lymphoblast, EBV + & activated c-Myc Definition: Type of lymphoblastic lymphoma. Intermediate B cell proliferation. Cause: t(8;14) c-Myc. Pathogenesis: EBV associated, c-Myc translocation from chromosome 8 to 14 present ’āĀderegulation of oncogenic function ’āĀ increased cell growth. Clinical Presentation: extra-nodal mass in jaw, GIT, gonads in young adults/kids. IHC ’āĀ starry sky appearance on microscopy. ŌĆó African form ’āĀ jaw. ŌĆó Sporadic form ’āĀ abdomen. ŌĆó Rare in Europe. ŌĆó Occurs in children and adolescents. Lymphocyte, Mantle cell, Marginal cell, Lymphoblast, Immunoblast, Centrocyte/Cleaved FCC ŌĆō follicle centre cell Centroblast/Non cleaved FCC Plasma cell ŌĆō large B cells F.C.C. Cleaved & non-cleaved Aka ’āĀ centrocytes/ centroblasts Histiocytes Mantle cells Marginal Cells Plasma cell Lymphocytes L O W G R A D E H I G H G R A D E
- 5. T cell NH-Lymphomas Low Grade 1. Mycosis Fungoides ŌĆō T cell lymphoma producing scaly, pruritic, well-demarcated skin plaques and patches. In the later stages of the disease, mushroom-shaped tumours develop within the plaque lesions, and ultimately lymphadenopathy and hepatosplenomegaly can develop. ŌĆó Occurs in adults ŌĆó 12 year survival 2. Sezary syndrome ŌĆō Cutaneous (skin) T-cell lymphoma with leukaemic dissemination of mutated T cells (which distinguishes it from mycosis fungoides). It thus becomes a T cell leukaemia and is considered an advanced stage of mycosis fungoides. 3. T cell Chronic Lymphocytic leukaemia (CLL) High Grade 1. Peripheral T CellLymphoma (most high grade are classified as this) 2. Enteropathy associated T CellLymphoma (EATL) ŌĆō It is a complication of celiac disease, occurs in the small bowel and is commoner in those with poor dietary control. 3. T Lymphoblastic Lymphoma ŌĆó Young adults but very rare ŌĆó Rapid enlargement of nodes ŌĆó On histology, large lymphoid cells that react with T lymphocyte markers 4. T Adult T cell leukaemia/lymphoma ŌĆó Rare ŌĆó Japan/Caribbean ŌĆó HTLV1 Virus ŌĆó Hypercalcaemia (PTH) Other Lymphomas 1. Extra-Nodal Lymphoma ŌĆó Lymphomas of mucosa and non-nodal tissue 2. Nasal Lymphoma ŌĆó High grade lymphoma of nose ŌĆó Null of NK cells ŌĆó Common in Asia but uncommon in Europe ŌĆó EBV associated Causes of Lymphoma 1. Antigen challenge: the first encounter between an immunocompetent lymphocyte and an invading antigen. 2. Viruses ŌĆó EBV associated with: BurkittŌĆÖs, Nasal lymphomas, HodgkinŌĆÖs (BNH) 3. Immunodeficiency 4. Radiation 5. Previous chemotherapy Leukaemia vs Lymphoma Summary of Management (for ALL NHLs) Diagnosis ŌĆō ŌĆó Radiologist takes the trucut ŌĆó Painless persistent enlargement of node ┬▒ B symptoms ŌĆó Loss of normal architecture (not reactive follicular hyperplasia) ŌĆó Monoclonality ’āĀ malignancy (determined by molecular studies of gene rearrangements) ŌĆó Hodgkin or Non Hodgkin ŌĆó Reed Sternberg cell ’āĀ Dx Hodgkins ŌĆó No RS cells Dx ’āĀ Non Hodgkins ŌĆó Small cells (Low Grade) or large cells High Grade) replace node ŌĆó Lymphoid markers are essential to type lymphoma correctly ŌĆó Molecular markers now being increasingly used Grade ŌĆō Rye Grading Stage ŌĆō Ann Arbor Staging ŌĆō CT, PET, BMT Treatment ŌĆō ŌĆó Rituximab ŌĆōB cell (CD20 monoclonal antibody) ŌĆó Chemotherapy ŌĆó Radiotherapy ŌĆó Bone marrow transplant Lymphoma Leukaemia High WCC >20,000 Normal WCC Patchy marrow involvement Extensive marrow replacement Little lymphadenopathy Prominent lymphadenopathy
- 6. Thymus The thymus arises from the endoderm of 3rd and 4th branchial pouch. It migrates down from the neck to the mediastinum where it houses T cells and produces hormones that allow them to mature further. Thymus gets smaller after birth and is almost completely atrophied in adults. Functions of Thymus ŌĆó Responsible for differentiation and direction of T cells ŌĆó Central role in cell mediated immunity Enlargement of Thymus 1. Myasthenia gravis ŌĆó 80% thymic hyperplasia ŌĆō autoimmune thymitis ŌĆó 80% AChr antibody ŌĆō against myeloid cells ŌĆó 15% get thymoma ŌĆó Treatment ŌĆō Thymectomy 2. Thymomas (epithelial neoplasm of thymus; ŌĆśomaŌĆÖ doesnŌĆÖt indicate benign or malignant - can be either) ŌĆó May present with associated diseases: Ōüā 30% myasthenia gravis Ōüā Rheumatoid arthritis Ōüā SjogrenŌĆÖs syndrome Ōüā Anterior mediastinal mass Ōüā NB: Prognosis behaviour correlates with grade 3. Lymphomas ŌĆó T cell ŌĆō most are T cell ŌĆó B cell 4. Germ cell tumours 5. Carcinoid tumours Spleen ŌĆó White pulp: lymphoid follicles (Malpighian bodies). ŌĆó Red pulp: venous sinuses & cords (lymphocytes). ŌĆó Weight: 120-150g. Functions of Spleen Splenic Atrophy ŌĆó Physiological ŌĆō old age. ŌĆó Sickle cell disease ŌĆō sickle cells get trapped in blood vessels that supply the spleen ’āĀ spleen becomes infarcted in areas ’āĀ heals by fibrosis ’āĀ small spleen. ŌĆó Coeliac disease ŌĆō idiopathic. Splenomegaly Splenomegaly causes: hypersplenism which is the enlargement of spleen for any reason ŌĆōcausing destruction of blood cells and consequently a reduction in these cells in the peripheral blood ’āĀ anaemia, thrombocytopenia & leukopenia. Causes of splenomegaly include: 1. Congestive ŌĆó Cirrhosis of liver ’āĀ portal vein thrombus ’āĀ inc. pressure on the splenic vein. 2. Collagen Vascular Diseases (Autoimmune Disorders) ŌĆó Rheumatoid arthritis ŌĆó Systematic Lupus Erythematosus (SLE) ŌĆó Polyarteritis Nodosa (PAN) 3. Storage Disorders ŌĆó Hyperlipidaemias ŌĆó Lipid storage disorders ŌĆó GaucherŌĆÖs disease ŌĆó Neiman PickŌĆÖs Disease 4. Infections ŌĆó Malaria ŌĆó Leishmaniasis (protozoal) ŌĆó Infectious mononucleosis ’āĀ spontaneous rupture ŌĆó Brucellosis ŌĆó S.B.E ŌĆō subacute bacterial endocarditis ŌĆó Endocarditis ŌĆō septic emboli from endocarditis go to the spleen ’āĀ abscess. NB: Splenomegaly due to infection is more seen in children and when seen in adults more due to viral than bacterial infection (esp. infectious mono). 5. Amyloidosis 6. Disorders of blood & marrow ŌĆó Leukaemias and Lymphomas ŌĆó Haemolytic anaemia ’āĀ red cells broken down by histiocytes & macrophages in spleen ’āĀ gets bigger. ŌĆó Myelofibrosis ’āĀ myelo = fibrosis; spleen canŌĆÖt produce red cells & blood components so function taken over by the liver. ŌĆó Myeloproliferative disorders Myeloproliferative Cell Neoplasms/Disorders Clonal neoplastic proliferation of stem cells, affecting all cell lines of the bone marrow with variable clinical presentation and variable prognosis (excluding acute leukaemia). ŌĆó Diagnosis ŌĆó Clinical presentation ŌĆō (3 conditions) ŌĆó FBC ŌĆó BMT and BM aspirate ŌĆó Pathogenesis ŌĆō activating mutation in gene coding for tyrosine kinases. Characteristics 1. Arise from common stem cell cases with intermediate features 2. Frequent evolution of 1 type to another 3. Invariable involvement of more than 1 cell line ŌĆō due to an abnormal clone with increased sensitivity to growth factors. 4. Occur in people > 50 years 5. Splenomegaly 6. Mutation of the tyrosine kinase JAK2 (Janus kinase ŌĆō 2 gene). Causes increased sensitivity to intercellular signalling from growth factors. Presentation Concepts ŌĆó Excess of one cell type may cause a decrease of other cell types High content of one cell type may cause symptoms ŌĆó Anaemia and infection ŌĆó Bleeding/thrombosis ŌĆó Hyperviscosity syndrome Tumour Markers in Nodes & Spleen, Thymus and Bone Marrow 1. Haemopoiesis 2. Antibody formation 3. Cell sequestration 4. Cell destruction 5. Iron metabolism 6. Phagocytosis
- 7. 1. Chronic granulocytic/myeloid leukaemia (commonest) 2. Myelofibrosis ŌĆō 60% JAK2 3. Polycythaemia rubra vera (RBC) ŌĆō 90% JAK2 4. Essential thrombocythaemia/ Thrombocytosis (Platelets) ŌĆō 60% JAK2 1) Chronic Myeloid/Granulocytic Leukaemia (CML/CGL) ŌĆó Neoplastic proliferation of stem cells that differentiate into mature myeloid cells, especially granulocytes (characteristically basophils). ŌĆó Characterised by Philadelphia fusion chromosome ŌĆō t(9;22) which results in a BCR-ABL fusion protein with increased tyrosine kinase activity. ŌĆó This is also an MPD (Myeloproliferative Disorder). Presentation ŌĆó Marrow replacement with/without failure ’āĀ anaemia, bleeding, bruising, infection. ŌĆó Marked leucocytosis ŌĆō 50,000 abnormal. ŌĆó Marked hepatosplenomegaly. ŌĆó Weight loss. Epidemiology ŌĆó Middle age 40-60 years. Diagnosis 1. WCC above 100,000 instead of 7,000 2. Increased blasts in the peripheral blood ’āĀ too many being released (shouldnŌĆÖt normally be there) ’āĀ can become a crisis. 3. PHI chromosome 22.9 (used to) 4. BCR-ABL rearrangement diagnostic of CML. 2) Myelofibrosis - 60% JAK2 Neoplastic proliferation of mature myeloid cells especially megakaryocytes. Primary Myelofibrosis: Megakaryocytes produce excess platelet-derived growth factor (PDGF) ’āĀ marrow fibrosis. Secondary Myelofibrosis: ŌĆó Metastases to marrow ŌĆó Radiotherapy to marrow ŌĆó Cytotoxic drugs Presentation ŌĆó Fibrosis reduces marrowŌĆÖs haematopoietic capability ’āĀ migration of erythroid precursors to spleen & liver ’āĀ extramedullary haematopoiesis ’āĀ hepato- splenomegaly & poikilocytosis (abnormal RBCs). ŌĆó Loss of marrow cells ŌĆó Terminal blast crisis ŌĆó Life expectancy - 7 years Treatment ŌĆó Supportive ŌĆó Marrow stimulation ŌĆó +/- Splenectomy (cells being produced are being destroyed in the spleen remove it to salvage the few being produced) 3) Essential thrombocythemia/thrombocytosis (platelets) - 60% JAK2 Neoplastic proliferation of mature myeloid cells especially platelets. Presentation: ŌĆó Increased platelet count: 1 million; (normal: 350,000) ŌĆó Bleeding/thrombotic abnormalities ŌĆó Enlarged spleen ŌĆó Enlarged liver Treatment ŌĆó Hydroxyurea 4) Polycythaemia Rubra Vera ŌĆō 90% JAK2 Neoplastic proliferation of mature myeloid cells especially RBCs ’āĀ increased red cell volume. Primary Polycythaemia: ŌĆó Malignancy of red blood cells ŌĆó High Hb and Haematocrit Secondary Polycythaemia: ŌĆó High altitudes ŌĆó Congenital Heart Disease ŌĆó Tumours (e.g. renal cell carcinoma ) ŌĆó Erythropoietin production (e.g. renal carcinoma) Presentation ŌĆó Red face (jumping jacks ’āĀ JAK ’āĀ red face) ŌĆó Thrombotic and haemorrhagic events ŌĆó Increased Hb ŌĆó Enlarged spleen ŌĆó Marrow erythropoiesis Treatment 1. 1st line: Phlebotomies (older patients): remove excess cells by removing blood. 2. 2nd line: Hydroxyurea (myelosuppressive treatment) 3. Exclude secondary causes 4. Radiotherapy with 32P isotope. Prognosis: 50%= 12 year survival (usually terminal with blast crisis).
- 8. Investigations ŌĆó FBC ŌĆó Leukocyte ALK phosphatase (LAP) differentiates CML from other causes of leucocytosis ŌĆó BCR-Abl gene rearrangement ŌĆó Uric acid ŌĆó JAK2 ŌĆó BMT ŌĆō bone marrow trephine (always have to do this) Myelodysplastic Syndrome Smouldering neoplastic proliferation of stem cells of bone marrow, majority terminate after 1-3 years in leukaemia (more aggressive) occurs in younger ppl ŌĆó A pre-leukaemic disorder ŌĆó Usually low peripheral cell count with hypercellular marrow ŌĆó Often in Myeloproliferative cell neoplasms/disorders you have a high peripheral cell count and hypercellular marrow ’āĀ ŌĆó Associated with a variety of chromosomal abnormalities ŌĆó Diagnosis based on clinical haematological and bone trephine ŌĆó May follow previous chemotherapy treatment or may occur de novo ŌĆó Classification of myelodysplasia depends on which cell line shows the dominant abnormality. ŌĆó There are 8 different types ŌĆó These are difficult to diagnose and require cytogenetic studies and correlation between the marrow aspirate and the FBC etc ŌĆó Some will progress into Leukaemia within 2 years