Meningiomyelitis
- 2. Rab 8 year old Labrador X Referred to SAH for urinary and faecal incontinence
- 3. Clinical Presentation 26.06.14: • Urinary/faecal incontinence • Mild ataxia • Had MRI and found disc protrusion at L7-S1 30.06.14: • Acute hind limb collapse • Marked hind limb ataxia • Urinary and faecal incontinence
- 4. Clinical Exam • QAR • Temperature 39.3 • Markedly ataxic on hind limbs but able to walk • Continued to urinate after bladder palpated • NAD otherwise
- 5. Neurological Exam Cranial Nerve Assessment • NAD on exam Postural Reaction Testing • Absent proprioceptive placing on both hind limbs • Reduced hopping reaction in both hind limbs Sensory Evaluation • Neck manipulation good • Pain over thoracolumbar spine
- 6. Gait • Hind limbs ataxic • Hind limbs cross over • Knuckle on right hind at times • Grade 2 at initial presentation • Now grade 3
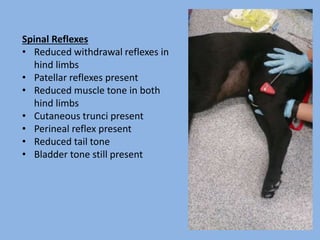
- 7. Spinal Reflexes • Reduced withdrawal reflexes in hind limbs • Patellar reflexes present • Reduced muscle tone in both hind limbs • Cutaneous trunci present • Perineal reflex present • Reduced tail tone • Bladder tone still present
- 8. Recognising and Localising Spinal Cord and Peripheral Nerve Lesions (2014) Jacques Penderis Lesion localised to T3-L3
- 9. Differential Diagnoses 1. Inflammatory- Meningitis - Myelitis 2. Neoplasia- Lymphoma 3. Degenerative- Degenerative Myelopathy
- 10. Overnight Plan • Methadone q6h for pain control • Urinary catheter • No food after 10pm
- 11. Investigation 1. Bloods Haematology- NAD Biochemistry- decreased albumin 2. Electromyelography NAD 3. CSF Analysis Smear - NCC 720 per microlitre (ref range 5) - 42% non degenerative neutrophils - 39% macrophages - 19% lyphocytes Protein- 7080 mg/L
- 12. Results • Neoplasia excluded from previous MRI • Negative EMG excluded myelopathies • Marked increase in WBCs in CSF indicated inflammatory process -non degenerate neutrophils excludes bacterial meningitis
- 14. Treatment Plan Treating as if Meningoencephalitis • Cytarabine 0.49ml BID • Prednisolone 62.5mg BID • Clindamicin 450mg BID • Methadone q6h switched to Vetergesic (as of 02.07.14) • Urinary catheter until less painful • Hartmann’s Fluids 2X maintenance as not drinking
- 15. Progress Slowly improving! Improved withdrawal reflexes on both hind limbs Walking with sling but mostly unassisted
- 16. Steroid-Responsive Meningitis- Arteritis • Most common form of Meningitis in dogs • Non-infectious inflammatory condition of meninges • Usually affects young dogs from 8-18 months • Breeds affected- Newfoundland, Pointer, Weimaraner, Vizla
- 17. Clinical Signs of SRMA • Pyrexia • Spinal pain- predominately cervical - cervical rigidity - will not turn head • Anorexia • Neurological deficits in chronic form
- 18. Diagnosis • Signalment- right age - clinical signs - breed • No radiographic abnormalities • CSF analysis- inflammatory - non degenerative neutrophils • Acute phase proteins may be supportive
- 19. Treatment • Prednisolone- tapering from initial immunosuppresive dose of 2-4 weeks - continue to taper dose over 4-6 months • Some patients require longer treatment or another drug such as Cytarabine Prognosis is good if treated early and aggressively
- 20. Special thanks to Carmen Yeamans, Intan Shafie and all of the Neurology team BSAVA Manual of Canine and Feline Neurology Approach to Spinal Pain, Acute Paralysis and Progressive Paralysis (2014), Jacques Penderis Recognising and Localising Spinal Cord and Peripheral Nerve Lesions (2014), Jacques Penderis