metabolic syndrome and its clinical implications
- 1. METABOLIC SYNDROME DrVinoth Gnana Chellaiyan D
- 2. International Diabetes Federation Definition: Abdominal obesity plus two other components: elevated BP, low HDL, elevated TG, or impaired fasting glucose
- 3. Definition Constellation of metabolic abnormalities that confer increased risk of cardiovascular disease(CVD) and diabetes mellitus.
- 4. Alternative names ? Metabolic syndrome ? Syndrome X ? Insulin resistance syndrome ? Deadly quartet ? Reaven’s syndrome
- 5. The major features of metabolic syndrome include ?Central obesity ?Hypertrilgyceridemia ?Low high density lipoprotein (HDL) ?Hyperglycemia ?hypertension
- 6. EPIDEMIOLOGY ? Prevalence increases with age ? Greater industrialization and urbanization ? Increase in waist circumference is found predominantly in women. ? Fasting TG>150 mg/dl and hypertension more likely in men.
- 7. Risk factors ? Overweight/ obesity- central (key feature) ? Sedentary lifestyle ? Predictor of CVd events and associted mortality ? Associated with central obesity, TG’s, HDL, BP, glucose intolerance ? Aging- prevalence increases with age ? Diabetes mellitus- approx. 75% of T2DM or IGT have metabolic syndrome ? Coronary heart disease- 50% of CHD patients have metabolic syndrome ? ? About 1/3rd of MS patients have premature CAD ? Lipodystrophy- both genetic or acquired have severe insulin resistance
- 8. CLINICAL FEATURES ? Usually asymptomatic and a high index of suspicion is needed for diagnosis ? Examination - ?Increased waist circumference ?Increased Blood Pressure ?Lipoatrophy ?Acanthosis nigricans/ skin tags Should alert to search for other abnormalities
- 10. Other associated conditions 1) Cardiovascular disease increased risk for new onset CVD, ischemic stroke, PVD 2) Type 2 diabetes mellitus increased risk by 3-5 folds 3) NAFLD and/or NASH 4) Hyperuricemia 5) PCOS- prevalence 40-50% 6) OSA- commonly associated with obesity, HTN & insulin resistance (CPAP improves insulin sensitivity)
- 12. IDF criteria 1. Waist circumference: ≥90 in males ≥80 in females 2. Plus two or more of the following a) Hypertriglyceridemia: ≥150 TG’s or specific medication b) Low HDL cholesterol: <40(M) and <50(F) or specific medication c) Hypertension: blood pressure ≥130 mm systolic or ≥85 mm diastolic or specific medication d) Fasting plasma glucose: ≥100 mg/dl or specific medication or previously diagnosed T2DM
- 13. IDF criteria *Diagnosis is established when ?3 of these risk factors are present. ? Abdominal obesity is more highly correlated with metabolic risk factors than is ? BMI. ? Some men develop metabolic risk factors when circumference is only marginally increased. <40 mg/dL <50 mg/dL or Rx for ↓ HDL Men Women >90 cm >80 cm Men Women ?100 mg/dL or Rx for ↑ glucose Fasting glucose ?130/?85 mm Hg or on HTN Rx Blood pressure HDL-C ?150 mg/dL or Rx for ↑ TG TG Abdominal obesity? (Waist circumference? ) Defining Level Risk Factor
- 14. Waist circumference Country / Ethnic group 94 cm 80 cm Male Female Europids * In the USA, the ATP III values ( 102 cm male; 88 cm female) are likely to continue to be used for clinical purposes 90 cm 80 cm Male Female South Asians Based on a Chinese , Malay and Asian-Indian population 90 cm 80 cm Male Female Chinese 90 cm 80 cm Male Female Japanese ** Use South Asian recommendations until more specific data are available Ethnic South and Central Americans Use European data until more specific data are available Sub-Saharan Africans Use South Asian recommendations until more specific data are available EMME ( Arab) populations IDF criteria contd…
- 16. Pathogenesis ? Insulin resistance ? Increased waist circumference ? Dyslipidemia ? Glucose intolerance ? Hypertension ? Decreased adiponectin levels
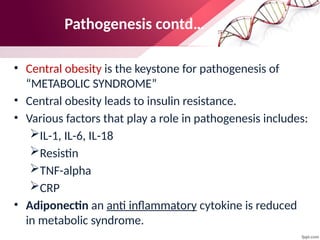
- 17. Pathogenesis contd… ? Central obesity is the keystone for pathogenesis of “METABOLIC SYNDROME” ? Central obesity leads to insulin resistance. ? Various factors that play a role in pathogenesis includes: ?IL-1, IL-6, IL-18 ?Resistin ?TNF-alpha ?CRP ? Adiponectin an anti inflammatory cytokine is reduced in metabolic syndrome.
- 19. Pathogenesis contd… Impaired insulin mediated glucose uptake Toxic injury to pancreatic islets Increased insulin resistance Hyperglycemia Type 2 DM Insulin resistance pp/fasting hyperinsulinemia Lipolysis by LPL Abundance of FFA’s
- 22. How to diagnose? ? IDF criteria ? H/o symptoms of OSA in all patients ? H/o PCOS in premenopausal women ? Family H/o CVD and DM ? Waist circumference and BP measurement ? Laboratory investigations ? Fasting lipid profile and fasting glucose ? hs-CRP, fibrinogen, uric acid, urinary microalbumin ? LFT for NAFLD ? Sleep study for OSA ? Testosterone, FSH, LH for PCOS
- 23. TREATMENT
- 24. ? Weight reduction- include a combination of caloric restriction, increased physical activity, and behavior modification. LIFESTYLE MODIFICATIONS
- 25. ? ~500 kcal restriction daily equates to weight reduction of 1 lb per week. ? Diets restricted in carbohydrate typically provide a rapid initial weight loss. ? Adherence to the diet is more important than which diet is chosen. ? A high-quality diet— i.e., enriched in fruits, vegetables, whole grains, lean poultry, and fish—should be encouraged to provide the maximum overall health benefit. DIET---
- 26. What to do..?
- 27. PHYSICAL ACTIVITY- ? 60–90 min of daily activity (At least 30 min.) Gradual increases in physical activity should be encouraged to enhance adherence and avoid injury. ? Some high-risk patients should undergo formal cardiovascular evaluation before initiating an exercise program. ? Physical activity could be formal exercise such as jogging, swimming, or tennis or routine activities, such as gardening, walking, and housecleaning.
- 28. ? Appetite suppressants- phentermine and sibutramine. ? Absorption inhibitors- Orlistat ? Bariatric surgery is also an option for patients with BMI >40 kg/m2 or >35 kg/m2 with comorbidities. OBESITY
- 29. ? A fasting triglyceride value of <150 mg/dL is recommended. A weight reduction of >10% is necessary to lower fasting triglycerides. ? A fibrate (gemfibrozil or fenofibrate) is the drug of choice to lower fasting triglycerides and typically achieve a 35–50% reduction. ? Other drugs that lower triglycerides include statins, nicotinic acid, and high doses of omega-3 fatty acids. TRIGLYCERIDES
- 30. ? For rise in HDL cholesterol, weight reduction is an important strategy. ? Nicotinic acid is the only currently available drug with predictable HDL cholesterol-raising properties. ? Statins, fibrates, and bile acid sequestrants have modest effects (5–10%), and there is no effect on HDL cholesterol with ezetimibe or omega-3 fatty acids. HDL Cholesterol
- 31. LDL Cholesterol For patients with the metabolic syndrome and diabetes, LDL cholesterol should be reduced to <100 mg/dL.
- 32. BLOOD PRESSURE ? The direct relationship between blood pressure and all-cause mortality rate has been well established. ? Best choice for the first antihypertensive should usually be an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker. ? In all patients with hypertension, a sodium-restricted diet enriched in fruits and vegetables and low-fat dairy products should be advocated.
- 33. ? Insulin resistance is the primary Patho-physiologic mechanism for the metabolic syndrome. ? Several drug classes [biguanides, thiazolidinediones (TZDs)] increase insulin sensitivity. ? Both metformin and TZDs enhance insulin action in the liver and suppress endogenous glucose production. TZDs, but not metformin, also improve insulin-mediated glucose uptake in muscle and adipose tissue. ? Benefits of both drugs have also been seen in patients with NAFLD and PCOS, and the drugs have been shown to reduce markers of inflammation and small dense LDL. INSULIN RESISTANCE
- 34. ? Most patients with metabolic syndrome exhibit a prothrombotic state characterized by elevations of plasminogen activator inhibitor-1 and fibrinogen. ? Use of low dose aspirin can be recommended for patients with metabolic syndrome, who have a high CV risk, those with overt type 2 diabetes mellitus, or atherosclerotic cardiovascular diseases. ? Metabolic syndrome frequently is accompanied by a pro-inflammatory state, characterized by increased CRP levels. No specific treatment available. PROTHROMBOTIC & PROINFLAMMATORY STATE
Editor's Notes
- #11: In addition to type 2 diabetes, insulin resistance is associated with the development of a broad spectrum of clinical conditions. These include hypertension, atherosclerosis, dyslipidemia, decreased fibrinolytic activity, impaired glucose tolerance, acanthosis nigricans, hyperuricemia, polycystic ovary disease, and obesity. Adapted from Consensus Development Conference of the American Diabetes Association. Diabetes Care. 1998;21:310-314.
- #14: According to the International Diabetes Foundation (IDF) definition of the metabolic syndrome, central obesity (defined by waist circumference) is an essential component for diagnosis of the syndrome. The IDF definition recognizes ethnic-specific values for waist circumference, as shown on this slide. The IDF consensus group acknowledged that these are pragmatic cut-points taken from various different data sources, and that better data will be needed to link these to risk. The IDF points out that although a higher cut-point is currently used for all ethnic groups in the United States for clinical diagnosis, it is strongly recommended that for epidemiological studies and, wherever possible, for case detection, ethnic group-specific cut-points should be used for people of the same ethnic group wherever they are found. Thus the criteria recommended for Japan would also be used in expatriate Japanese communities, as would those for South Asian males and females regardless of place and country of residence. International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. 2005. Tan CE, Ma S, Wai D, et al. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182-1186.
- #15: To measure waist circumference, 1) locate the upper hip bone and the top of the right iliac crest, 2) place the measuring tape in a horizontal plane around the abdomen at the iliac crest, 3) ensure that the tape is snug but does not compress the skin, 4) the tape should be parallel to floor, and 5) record the measurement at the end of a normal expiration. Men are at increased relative risk if they have a waist circumference greater than 40 inches (102 cm); women are at an increased relative risk if they have a waist circumference greater than 35 inches (88 cm). There are ethnic- and age-related differences in body fat distribution that may affect the predictive validity of waist circumference as a surrogate for abdominal fat. Heterogeneity of composition of abdominal tissues, in particular adipose tissue and skeletal muscle, and their location-specific and changing relations with metabolic factors and CV risk factors in different ethnic groups do not allow a simple definition of abdominal obesity that could be applied uniformly. In particular, Asians appear to have higher morbidity at lower cutoff points for waist circumference than do white Caucasians. National Institutes of Health, National Heart, Lung, and Blood Institute, NHLBI Obesity Education Initiative, North American Association for the Study of Obesity. The practical guide to the identification, evaluation, and treatment of overweight and obesity in adults. NIH Publication Number 00-4084. October 2000. Misra A, Wasir JS, Vikram NK. Waist circumference criteria for the diagnosis of abdominal obesity are not applicable uniformly to all populations and ethnic groups. Nutrition. 2005;21:969-976.
































![? Insulin resistance is the primary Patho-physiologic mechanism for the
metabolic syndrome.
? Several drug classes [biguanides, thiazolidinediones (TZDs)] increase insulin
sensitivity.
? Both metformin and TZDs enhance insulin action in the liver and suppress
endogenous glucose production. TZDs, but not metformin, also improve
insulin-mediated glucose uptake in muscle and adipose tissue.
? Benefits of both drugs have also been seen in patients with NAFLD and PCOS,
and the drugs have been shown to reduce markers of inflammation and small
dense LDL.
INSULIN RESISTANCE](https://image.slidesharecdn.com/metabolicsyndrome-240921044746-5feced29/85/metabolic-syndrome-and-its-clinical-implications-33-320.jpg)

