Neonatal jaundice with abo incompatibility, physiological jaundice
- 2. Definition Jaundice = visible manifestation in skin and sclera of elevated serum bilirubin Visible in adults at STB > 2mg/dl In neonates if STB> 5 mg/dl
- 3. Incidence Chemical hyperbilirubinemia (> 2mg/dl) universal in newborns during 1st week. Some degree of Jaundice > 60-70% of term newborns and 80% of preterm newborns. Ref: NNF teaching aids on newborn care
- 4. Bilirubin physiology bilirubin Ligandin (Y-acceptor) UGT Bilirubin MG, Bilirubin DG Bile Small Bowel EH circulation Stercobilin (gut bacteria) β-glucuronidase excreted Deconjugated
- 5. Physiological Mechanisms Of Neonatal Jaundice Increased synthesis Less efficient binding and transport Less efficient hepatic conjugation and excretion Enhanced absorption via enterohepatic circulation
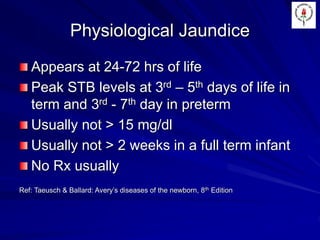
- 6. Physiological Jaundice Appears at 24-72 hrs of life Peak STB levels at 3rd – 5th days of life in term and 3rd - 7th day in preterm Usually not > 15 mg/dl Usually not > 2 weeks in a full term infant No Rx usually Ref: Taeusch & Ballard: Avery’s diseases of the newborn, 8th Edition
- 7. Pathological Jaundice - Clinical Criteria Clinical jaundice in 1st 24 hours STB > 17 mg/dl Rate of rise > 0.2 mg/dl/h or 5mg/dl/d Direct serum bilirubin > 2 mg/dl Clinical jaundice > 2 weeks in a full term infant Ref: Taeusch & Ballard, Avery’s disease of the newborn, 8th Edition
- 8. Clinical Assessment Extent Important basic assessments Clinical clues to causes Presence of complications of jaundice
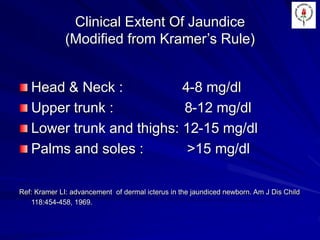
- 9. Clinical Extent Of Jaundice (Modified from Kramer’s Rule) Head & Neck : 4-8 mg/dl Upper trunk : 8-12 mg/dl Lower trunk and thighs: 12-15 mg/dl Palms and soles : >15 mg/dl Ref: Kramer LI: advancement of dermal icterus in the jaundiced newborn. Am J Dis Child 118:454-458, 1969.
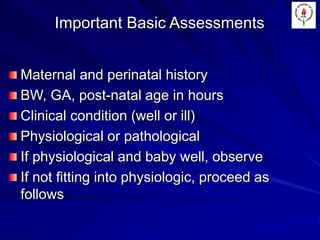
- 10. Important Basic Assessments Maternal and perinatal history BW, GA, post-natal age in hours Clinical condition (well or ill) Physiological or pathological If physiological and baby well, observe If not fitting into physiologic, proceed as follows
- 11. Clinical Clues to Causes - 1 Cephalhematoma or subgaleal hematoma Plethoric look Evidence of sepsis – purulent skin rash, infected umbilicus, conjunctivitis, hypothermia, refusal of feeds, respiratory distress, seizures, sclerema etc
- 12. Clinical Clues to Causes - 2 Stigmata of TORCH infections – rashes, cataracts, hepatosplenomegaly Hepatomegaly with palpable enlarged GB Evidence of ICH – seizures, apnea, refusal of feeds, impaired consciousness Evidence of GI abnormalities – abdominal distension, markedly visible peristalsis etc
- 13. Clinical Clues to Causes - 3 Evidence of hypothyroidism – hypothermia, LGA, sluggish at feeds, umbilical hernia Evidence of Trisomy 21 – Mongolian slant, Simian crease, thick protruding tongue, sluggish feeding, etc
- 14. Clinical Clues - Breast milk jaundice Presents as prolonged physiological jaundice or appears de-novo after 1st week In exclusively BF babies Maximum between 10-14 days STB > 15 mg/dl, BF cessation for 48 hours > dramatic fall > no rise thereafter For higher levels > phototherapy Exact cause not understood
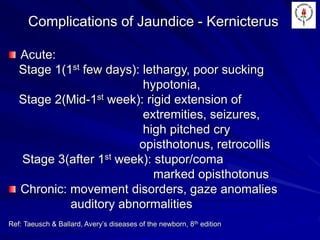
- 15. Complications of Jaundice - Kernicterus Acute: Stage 1(1st few days): lethargy, poor sucking hypotonia, Stage 2(Mid-1st week): rigid extension of extremities, seizures, high pitched cry opisthotonus, retrocollis Stage 3(after 1st week): stupor/coma marked opisthotonus Chronic: movement disorders, gaze anomalies auditory abnormalities Ref: Taeusch & Ballard, Avery’s diseases of the newborn, 8th edition
- 16. Lab Work Up Total,direct and indirect serum bilirubin Blood grouping and Rh typing Hematocrit, Reticulocyte count, PBS Direct Coomb’s test on baby Sepsis screen Liver function and Thyroid tests Torch assay
- 17. Management Aims: 1. To prevent STB from rising 2. To reduce STB level 3. To prevent neurotoxicity
- 18. Prevention of hyperbilirubinemia: 1. Early and frequent feeding 2. Adequate hydration 3. Administration of Anti-D injection to Rh negative mother
- 19. Reduction of STB levels and prevention of neurotoxicity Phototherapy Exchange transfusion
- 20. Phototherapy Phototherapy > unconjugated bilirubin > conjugated photoproducts > bile > stool, also > urine Blue light > 450-460nm wavelength and irradiance of 6-12µW/cm2/nm . The maximal surface area of naked baby exposed Distance - 45 cm. The eyes and genitalia covered . Feeding every 2 hours and frequent change of posture are necessary. Ideally double surface
- 21. Phototherapy Contd. The baby is turned every 2 hrs or after each feed Temp is monitored every 2-4 hrs Weight is taken daily More frequent breast feeds or 10-20% extra IV fluids are provided STB is measured every 12 hrs Phototherapy is discontinued if 2 STB values are < 10 mg/dl
- 22. Phototherapy: adverse effects Increased insensible water loss Loose green stools Hyperthermia / Hypothermia Rashes (erythema) Oxidative injury UV light irradiation Bronze baby syndrome
- 23. Exchange transfusion The most effective and reliable method to reduce STB It decreases the risk of bilirubin encephalopathy by: 1. Reducing total bilirubin load 2. Increasing the binding sites of plasma albumin 3. Shifting bilirubin out of plasma 4. Providing erythrocytes less apt to hemolyze 5. Removes sensitized RBC Ref: Taeusch & Ballard, Avery’s diseases of the newborn
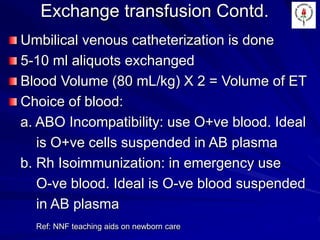
- 24. Exchange transfusion Contd. Umbilical venous catheterization is done 5-10 ml aliquots exchanged Blood Volume (80 mL/kg) X 2 = Volume of ET Choice of blood: a. ABO Incompatibility: use O+ve blood. Ideal is O+ve cells suspended in AB plasma b. Rh Isoimmunization: in emergency use O-ve blood. Ideal is O-ve blood suspended in AB plasma Ref: NNF teaching aids on newborn care
- 25. Maisel’s Chart STB (mg/dl) Birth Wt <24 hrs 24-48 hrs 49-72 hrs >72 hrs <5` All 5-9 All Photothera py if hemolysis 10-14 <2500G -------------- >2500 G Exchange if hemolysis Phototherapy -------------------------------------------------- Investigate if STB > 12 mg/dl 15-19 <2500 g -------------- >2500 g Exchange Transfusion Consider exchange -------------------------------- Phototherapy 20 and More All Exchange Transfusion
- 26. Maisel’s Chart For decision making based on Maisel’s chart, in the presence of following, treat as in next higher bilirubin category: a. Perinatal asphyxia b. Respiratory distress c. Metabolic acidosis d. Hypothermia e. Low serum protein f. Birth weight < 1500 g g. Signs of clinical or CNS deterioration Ref: NNF Teaching aids on newborn care
- 27. Conjugated Hyperbilirubinemia Defined as direct serum bilirubin > 2mg/dl Clues to suspect conjugated hyperbilirubinemia: a. High colored urine b. White / Clay colored stool c. Persistence of jaundice beyond 2 weeks d. Hepato-splenomegaly
- 28. Causes Of Unconjugated Hyperbilirubinemia Idiopathic neonatal hepatitis Inspissated bile syndrome Infections: Hepatitis B, TORCH, Sepsis Biliary tract malformations : EHBA, annular pancreas, choledochal cyst, bile duct stenosis Metabolic disorders: Galactosemia, hereditary fructose intolerance, alpha-1AT deficiency, tyrosinemia, glycogen storage disease IV, hypothyroidism TPN Down’s syndrome Ref: NNF teaching aids on newborn care