Neonatal sepsis coaching for nursing students.pptx
- 1. Emergency Obstetric and Newborn Care Neonatal sepsis
- 2. Learning objectives ’éŚ At the end of this session, the participant should be able to: ’éŚ define neonatal sepsis ’éŚ Recognize infant who is at risk ’éŚ Assess the infant with severe neonatal sepsis ’éŚ classify a young infant for very severe disease and local bacterial infection ’éŚ Manage the infant ’éŚ Counsel the mother
- 3. Definition ’éŚNeonatal sepsis can be defined as bacterial infection occurring in the first 28 days of life ’éŚInfection can be generalized or localized
- 4. Magnitude of the problem Neonatal sepsis is very common Neonatal causes of mortality Birth Asphyxia 27% Neonatal Sepsis 14% Congenital Abnormalities 11% Diarrohea 2% Others 7% Preterm Birth Complications 39% Source:Adapted from the Child Health Epidemiologic Reference Group Lancet Publication May 12, 2010
- 5. Why neonates are prone to infection ’éŚ Decreased humeral immunity ’éŚ Decreased cellular immunity ’éŚ Decreased white cell activity ’éŚ Deficient complement system ’éŚ Reduced IgA ’éŚ Thin skin ’éŚ Risk factors ’éŚ PROM ’éŚ Maternal infection ’éŚ Antepartum haemorrhage ’éŚ Prematurity ’éŚ Respiratory distress syndrome.
- 6. Diagnosis ’éŚThe clinical signs of infection in the newborn are often non specific and difficult to recognize. ’éŚThe findings listed below can be caused by other problems besides infection.
- 7. How to recognize neonatal sepsis ’éŚ Not specific ’éŚ Newborn infant with sepsis may present with any of the following: ’éŚ Generalized clinical signs ’éŚ Convulsions ’éŚ Lethargic or unconscious ’éŚ Not feeding well ’éŚ Fast breathing (60 breaths per minute or more) ’éŚ Periods of not breathing ’éŚ Fever (37.5 C or above or feels hot) or low body temperature (less than 35.5 C or feels cold) ’éŚ Jaundice
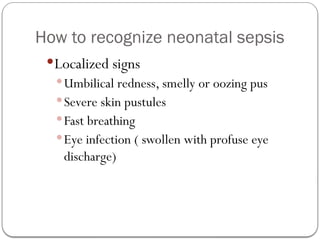
- 8. How to recognize neonatal sepsis ’éŚLocalized signs ’éŚUmbilical redness, smelly or oozing pus ’éŚSevere skin pustules ’éŚFast breathing ’éŚEye infection ( swollen with profuse eye discharge)
- 9. Other signs of severe sepsis ’éŚ Difficulty waking up the baby ’éŚ Rapid or slow breathing; indrawing of chest with breathing ’éŚ Periods of apnoea lasting more than 20 seconds ’éŚ Pale, grey or blue colour (blue tongue or lips is serious) ’éŚ Limp or rigid limbs ’éŚ Jaundice ’éŚ Distended abdomen
- 10. Classify illness ’éŚClassify (IMNCI classification): ’éŚVery severe disease or ’éŚLocal bacterial infection ’éŚ Bacterial infections can progress rapidly in young infants. ’éŚClassify (other classification) ’éŚSevere neonatal sepsis
- 11. Management of neonatal sepsis ’éŚEnsure patent Airway, ’éŚProvide oxygen if indicated* ’éŚUse bag and mask if not breathing well ’éŚGive first dose of Crystalline penicillin 100,000 IU/kg stat and 12 hourly and Gentamycin 5mg/kg stat and once daily. If preterm < 2kg give Gentamycin 4mg/kg stat and once daily
- 12. Management of neonatal sepsis ’éŚGive small frequent feeds if possible to prevent low blood sugar ’éŚIf too ill to feed use NG tube starting with 60mls/kg/day divided into 12 feeds. ’éŚArrange for URGENT referral to next level ’éŚStabilize and refer to next level ’éŚKeep the Infant warm on the way to the Hospital
- 13. Management of neonatal sepsis ’éŚ Local bacterial infection: ’éŚ Umbilical infection ’éŚ Examine the cord and abdomen. Look for: ’éŚ Moist cord ’éŚ Drainage of pus with a bad smell ’éŚ Red, swollen, inflamed skin around the umbilicus ’éŚ Distended abdomen (a sign that the baby is developing very severe disease) ’éŚ Classify (IMNCI) ’éŚ Serious umbilical cord infection ’éŚ Localized umbilical cord infection
- 14. Management of neonatal sepsis ’éŚ Classify: Serious umbilical cord infection if: ’éŚ There is pus discharge from the umbilicus, delayed cord separation or healing plus redness of skin and swelling which extends more than 1 cm around the umbilicus. ’éŚ The skin around the umbilicus may also be hardened. ’éŚ If baby has signs of sepsis such as a distended abdomen, the infection is very serious. ’éŚ Treat: Serious umbilical cord infection in the same manner as very severe disease
- 15. Management of neonatal sepsis ’éŚ Classify: Localized umbilical cord infection (non serious) if; ’éŚ The umbilicus has no pus discharge or foul smell. ’éŚ Redness and swelling around the skin of the umbilicus does not extend more than 1 cm. ’éŚ The baby has no danger signs. ’éŚ Treat localized bacterial infection: ’éŚ Give an appropriate oral antibiotic.(Amoxycillin) ’éŚ Teach the mother to treat local infections at home (cord care). ’éŚ Advise mother to give home care for the young infant. ’éŚ Follow-up in 2 days ’éŚ Teach mother about danger signs ’éŚ Advise mother when to return immediately.
- 16. Eye infection ’éŚ Red or swollen eyes with profuse pus discharge: ’éŚ Refer the baby, following the Referral Guidelines. ’éŚ For a baby less than 7 days old who has not been treated with antibiotics, treat for eye infection due to gonorrhoea. Give a single dose of antibiotics before referral: ceftriaxone 50mg/kg IM (do not give more than 125 mg) ’éŚ Start frequent eye irrigation with saline ’éŚ Refer the mother for STI screening and treatment for her and partner.
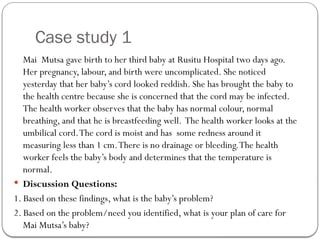
- 17. Case study 1 Mai Mutsa gave birth to her third baby at Rusitu Hospital two days ago. Her pregnancy, labour, and birth were uncomplicated. She noticed yesterday that her babyŌĆÖs cord looked reddish. She has brought the baby to the health centre because she is concerned that the cord may be infected. The health worker observes that the baby has normal colour, normal breathing, and that he is breastfeeding well. The health worker looks at the umbilical cord.The cord is moist and has some redness around it measuring less than 1 cm.There is no drainage or bleeding.The health worker feels the babyŌĆÖs body and determines that the temperature is normal. ’éŚ Discussion Questions: 1. Based on these findings, what is the babyŌĆÖs problem? 2. Based on the problem/need you identified, what is your plan of care for Mai MutsaŌĆÖs baby?
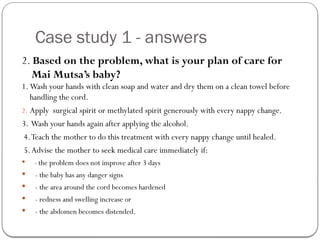
- 18. Case study 1 - answers 1. Based on these findings, what is the babyŌĆÖs problem? ’éŚThe baby has a localized cord infection. He has a moist cord with an offensive odour. ’éŚ The baby does not have a serious cord infection because the skin around the umbilicus is not red or inflamed,there is no drainage,and the baby has no signs of sepsis.
- 19. Case study 1 - answers 2. Based on the problem, what is your plan of care for Mai MutsaŌĆÖs baby? 1. Wash your hands with clean soap and water and dry them on a clean towel before handling the cord. 2. Apply surgical spirit or methylated spirit generously with every nappy change. 3. Wash your hands again after applying the alcohol. 4.Teach the mother to do this treatment with every nappy change until healed. 5.Advise the mother to seek medical care immediately if: ’éŚ - the problem does not improve after 3 days ’éŚ - the baby has any danger signs ’éŚ - the area around the cord becomes hardened ’éŚ - redness and swelling increase or ’éŚ - the abdomen becomes distended.
- 20. Key points ’éŚ Neonatal sepsis is very common ’éŚ Any very ill newborn infant may have neonatal infection ’éŚ Keep the baby warm, feed and counsel the mother ’éŚ Give Xpen and gentamycin before referral of an infant with very severe disease ’éŚ Refer urgently if infant develops danger signs
Editor's Notes
- #3: It is also essential to understand that many newborn emergencies can be prevented through maintaining good maternal health and nutrition, especially during pregnancy, labour, and postpartum. Comprehensive, high-quality care for mothers during pregnancy and childbirth is just as important as care for the baby after birth to ensure that every newborn starts out life with the best possible chance of reaching adulthood.
- #4: Ref:
- #7: The clinical signs of infection in the newborn are often difficult to recognize because they are not specific. The findings listed below can be caused by other problems besides infection.
- #11: * Oxygen may be administered via headbox or nasal prongs
- #15: Localized umbilical cord infection Treat the umbilicus/cord stump as follows: Wash your hands with clean soap and water and dry them on a clean towel before handling the cord. Apply surgical spirit or methylated spirit generously with every nappy change. 3. Wash your hands again after applying the alcohol. 4. Teach the mother to do this treatment with every nappy change till healed. 5. Remind the mother to use careful handwashing before and after caring for the baby. 6. Advise the mother to seek medical care immediately if: - the problem does not improve after 3 days - the baby has any danger signs - the area around the cord becomes hardened - redness and swelling increase or - the abdomen becomes distended.
- #16: Gonococcal ophthalmia neonatorum if a serious eye infection thst may cause blindness if not treated urgently and aggressively. Gonnococcal ophthalmia neonatorum is prevented by applying 1% tetracycline eye ointment within one our following birth