Neurological Medications.ppt
- 1. Neurological Medications ’ü» Review of central Nervous System ’ü» Description- Class ’ü» Medications ’ü» Side effects ’ü» Implementation
- 2. Central Nervous System ’ü» CNS- control center for the entire system, consists of the brain and spinal cord. Concerned with regulation and coordination of body activities ’ü» Peripheral nervous system- contains the nerves (afferent and efferent) which connect the CNS to all other parts of the body. It is divided into the motor nervous system which contains all the nerve fibers that run between the CNS and skeletal muscles and the Autonomic Nervous System which consists of all the nerve fibers that run between the CNS and smooth muscle, cardiac muscle, and glands. The ANS produces a response only in involuntary muscles and glands
- 3. Autonomic Nervous System ’ü» Two divisions: (Involuntary) ’ü» Sympathetic Nervous System- consists of ganglia and nerves that supply the involuntary muscles ’ü» Parasympathetic Nervous System- promotes normal functioning of digestion, urination, defecation, and heart beats at normal resting state.
- 4. Adrenergic Drugs ’ü» Mimic the activity of the sympathetic nervous system. ’ü» Used to treat hypotensive episodes, bronchial asthma, cardiac arrest, heart block, ventricular arrhythmias, allergic reactions. Topically relieve nasal congestion ’ü» Common adverse reactions include cardiac arrhythmias, > B/P, and HA. Do not produce slowed reaction to stimulus ’ü» Dobutamine, Levophed (norepinephrine) epinephrine, Triaminic
- 5. Adrenergic Drugs ’ü» Adverse Reactions cardiac arrhythmias such as bradycardia and tachycardia, HA, insomnia, nervousness, and increase in blood pressure. Management depends on drug used. Adrenergic drugs are potentially dangerous and great care must be taken. Observe pt and report ASAP.
- 6. Adrenergic Blocking Agents ’ü» Alpha-adrenergic blocking agent- block effects of alpha receptors thereby inhibiting the normal excitatory response of epi and norepi. ’ü» Used to treat hypertension associated with pheochromocytoma- a tumor of the adrenal gland that produces excess amounts of epi and norepi.
- 7. Beta-Adrenergic Blocking Agent ’ü» Block beta receptors, resulting in a decrease in heart rate. (Tenormin, Inderal) ’ü» Used to treat hypertension, arrhythmias, angina pectoris, and glaucoma. ’ü» Adverse reactions include bradycardia, dizziness, vertigo, and brochospasm ’ü» Labetalol- used to treat hypertension. Only drug considered alpha/beta adrenergic blocking. s/e include Ha, fatigue, skin rash ’ü» On initial dose of drug, take B/P and pulse in both arms. ’ü» If B/P significantly drops, withhold dose and contact the physician
- 8. Antiadrenergic Agent ’ü» Inhibit the release of norepinephrine from certain nerve endings, they also suppress the activity of the SNS. ’ü» Used to treat hypertension and arrhythmias ’ü» Adverse reactions include < B/P, arrhymthmias and headache ’ü» Take blood pressure each time before drug is given
- 9. Cholinergic drugs ’ü» Mimic the activity of the parasympathetic system, also called parasympathomimetic drugs) blocks acetylcholine breakdown important in nerve transduction ’ü» Used to treat myasthenia gravis and glaucoma, and to induce voiding in pts with urinary retention (mestinon, prostigmin)) ’ü» Adverse reactions include nausea, diarrhea, abd cramping, skin flushing, arrhythmias, and muscle weakness
- 10. Myasthenia Gravis ’ü» Disease characterized by great muscle weakness (without atrophy) and progressive fatigability ’ü» S/S muscles of face and neck involved, those of trunk and extremities secondary. Onset gradual, worsen in evening. Pt c/o of difficulty chewing, swallowing, and talking. Expressionless faces and ptosis usually present
- 11. Implementation ’ü» With Initial drug regimen, always monitor pt responses to drug. Frequently increased or decreased early in therapy. ’ü» Monitor for signs and symptoms of drug overdose ( may be difficult to regulate) ’ü» Elderly do not tolerate high doses of these drugs. ’ü» Drug underdose- may have rapid fatigability and drooping of the eyelids
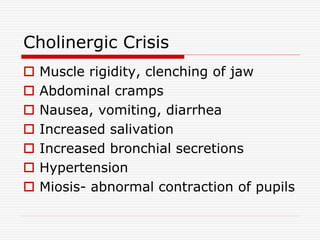
- 12. Cholinergic Crisis ’ü» Muscle rigidity, clenching of jaw ’ü» Abdominal cramps ’ü» Nausea, vomiting, diarrhea ’ü» Increased salivation ’ü» Increased bronchial secretions ’ü» Hypertension ’ü» Miosis- abnormal contraction of pupils
- 13. Nursing Management ’ü» Assess neuromuscular status including reflexes, muscle strength, and gait ’ü» Monitor pt for sis of overdose (cholinergic crisis) and underdone (myasthenia crisis) ’ü» Instruct pt to always take meds on time to prevent weakness ’ü» Instruct pt to take med before meals for best absorption ’ü» Instruct pt to wear medic-alert bracelet ’ü» Explain that antimyasthenic therapy is lifelong ’ü» Evaluate medication effectiveness based on neuromuscular improvements and muscle strength
- 14. Nursing Management- Glaucoma Instruct pt in instillation of eye drops Prior to instilling drops, check label of bottle to see if drug is for ophthalmic use Eye drops (pilocarpine) adverse reaction may be a temporary loss of vision acurity. Instill the eye drops in the lower conjunctional sac Administer eye drops with the hand holding the eye dropper supported against the patientŌĆÖs forehead. If eye drops are ordered to be left at bedside, nurse must make sure the medication is being used properly and at the right time.
- 15. Cholinergic blocking drugs ’ü» Inhibit the activity of acetylcholine by blocking the cholinergic receptors in the CNS ’ü» Side effects include dry mouth and drying of secretions of resp tract (encourage to take frequent sips of water), >pulse, blurred vision, restlessness, constipation ’ü» Contraindicated in glaucoma pts and COPD ( can develop dry, thick mucous secretions ’ü» Atropine- used preoperatively to reduce secretions of the upper respiratory tract ’ü» Use with elderly during hot weather may result in heat exhaustion (prostration) These drugs decrease sweating
- 16. Anticholinergic Drugs ’ü» Used in treatment of peptic ulcer disease (Quarzan,Robinul) ’ü» Pylorospasm- secondary to lesions of the stomach and duodenum ’ü» Renal colic (pain in region of kidney and toward the thigh) ’ü» Preanesthetic sedation ( Atropine) ’ü» Third degree Heart block (Atropine) ŌĆō always place on a cardiac monitor ’ü» If while taking an anticholinergic, experiences photophobia, place in semi darkened room ’ü» May be used as antidote for cholinergic toxicity (Cogentin and atropine)
- 17. Nursing Management ’ü» Monitor Vital signs ’ü» Assess for rigidity and tremors ’ü» Instruct pt to check with physician before taking any OTC meds ’ü» Instruct pt to minimize dry mouth by increasing fluid intake and by using ice chips , hard candy, and gum ’ü» Increase fluid and fiber to prevent constipation ’ü» Routine eye exams to assess for intraocular pressure
- 18. Anticoagulants ’ü» Used to prevent clot extension and formation. Do not dissolve clots ’ü» Usually initiated with heparin because of rapid onset of action ’ü» Maintenance therapy consists of warfarin ’ü» Lovenox-low molecular wt heparin may be used after surgery or with prolonged bedrest to prevent DVT
- 19. Antiparkinsonian Medications ’ü» ParkisonŌĆÖs is a progressive disease of the nervous system caused by deficiency of dopamine. ’ü» S/S fine tremors, rigidity of some muscle groups and weakness of others, slurred speech, mask-like facial expression and shuffling, unsteady gait.
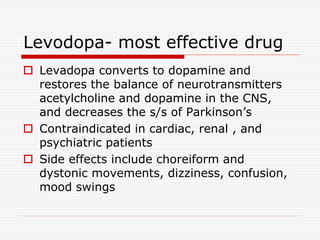
- 20. Levodopa- most effective drug ’ü» Levadopa converts to dopamine and restores the balance of neurotransmitters acetylcholine and dopamine in the CNS, and decreases the s/s of ParkinsonŌĆÖs ’ü» Contraindicated in cardiac, renal , and psychiatric patients ’ü» Side effects include choreiform and dystonic movements, dizziness, confusion, mood swings
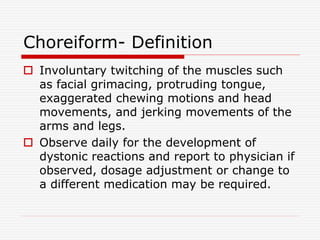
- 21. Choreiform- Definition ’ü» Involuntary twitching of the muscles such as facial grimacing, protruding tongue, exaggerated chewing motions and head movements, and jerking movements of the arms and legs. ’ü» Observe daily for the development of dystonic reactions and report to physician if observed, dosage adjustment or change to a different medication may be required.
- 22. Levadopa- continued ’ü» Some patients with ParkinsonŌĆÖs have difficulty communicating and will not tell the nurse that problems are occurring. ’ü» Carbidopa is given with levadopa either as one medication or as two separate drugs. If given together, teach patient that carbidopa must be given with levadopa.
- 23. Nursing Management ’ü» Assess Vital signs ’ü» Assess for risk of injury ’ü» Instruct pt to take with food of N/V occurs ’ü» Assess daily for dystonic movements ’ü» Instruct pt taking Sinemet to eat reduced protein diet, high-protein foods interfere with medication transport to CNS ’ü» Change positions slowly ’ü» Inform pt urine may change color ’ü» Instruct pt to report side effects and s/s of dyskinesia
- 24. Anticonvulsants ’ü» Seizure- abnormal disturbance in the electrical activity in one or more areas of the brain ’ü» Epilepsy- permanent, recurrent seizure disorder ’ü» Anticonvulsants- act to reduce the excitability of the nerve cells of the brain ( depress abnormal neuronal discharges) and prevent the spread of seizures
- 25. Anticonvulsants ’ü» Phenytoin (Dilantin) ’ü» Side effects are reddened gums that bleed easily, slurred speech, confusion, HA, elevated blood glucose, and depression ’ü» Other anticonvulsants include Tegretol, Depakote, and Neurontin
- 26. Nursing Management ’ü» Monitor serum levels to assess for toxicity ’ü» Instruct pt on importance of good oral hygiene and regular dental exams ’ü» Instruct pt to consult physician before taking other medications ’ü» Oral tube feedings may interfere with the absorption of oral dilantin and diminish the medication's effectiveness, feedings should be scheduled as far as possible from the drug administration
- 27. Benzodiazepines ’ü» Used to treat tonic-clonic seizures and status epileptics ’ü» Valium used to treat status epilepticus ’ü» Includes Klonopin, Tranxene, Valium and Ativan
- 28. Narcotic Analgesics ’ü» Suppress pain impulse but can also suppress respirations ’ü» Includes codeine, Diludid, Demerol, Percocet, Percodan, Darvon, Stadol, Nubain, Ultram, Methodone,Hydrococone, Oxycodone ’ü» Meperidine (Demerol) can increase intracranial pressure in head injuries
- 29. Narcotic Antagonists ’ü» Used to treat respiratory depression from narcotic overdose ’ü» Includes Narcan, revex, and reVia ’ü» Monitor B/P, respiration rate, and pulse every 5 mins, tapering to every 15 mins, then every 30 mins ’ü» Place pt on cardiac monitor ’ü» Have resuscitation equipment available ’ü» Do not leave patient unattended ’ü» Monitor pt closely, when antagonist wears off, may again display s/s of overdose