Normocytic normochromic anaemia Hemolytic anaemia
- 1. HEMOLYTIC ANAEMIA Dr. OM JHA
- 2. Introduction ŌĆó Characterized by: ŌĆō Premature RBC destruction (less than the normal 120-day lifespan). ŌĆō Elevated erythropoietin with increased erythropoiesis. ŌĆō Increased hemoglobin catabolites (e.g., bilirubin) ŌĆó Excess serum bilirubin is unconjugated. ŌĆó Ultimate levels of hyperbilirubinemia depend on: ŌĆō liver functional capacity ŌĆō Rate of hemolysis ŌĆó Normal liver ’āĀ severe jaundice ’āĀ rarely.
- 3. ContdŌĆ” ŌĆó BM erythropoiesis ’āĀ unable to compensate for degree of destruction of red cells ’āĀ Anaemia develops. ŌĆó Clinical and lab findings indicates: ŌĆō Accelerated destruction of red cells. ŌĆō Compensatory marrow regeneration. ŌĆó Mild hemolysis ’āĀ compensatory BM function adequate ’āĀ No manifestation of anaemia ’āĀ Compensated hemolytic anaemia.
- 4. Classification ŌĆó Location of hemolysis: Intravascular and extravascular. ŌĆó Source of defect causing hemolysis: Intracorpuscular defect and extracorpuscular defect ŌĆó Mode of onset: Hereditary and acquired disorders. ŌĆó Underlying mechanisms of hemolysis: Immune or Non-immune.
- 6. Contd..
- 7. Red Cells Destruction Extra-vascular Hemolysis ŌĆó Normal site of destruction of old RBCs: Spleen (80- 90%). ŌĆó In HA’āĀ This mechanism ’āĀ Exaggerated. Intra-vascular Hemolysis ŌĆó RBCs in circulation ’āĀ get destroyed ’āĀ release of Hb in plasma. ŌĆó Main pathway of: PNH.
- 10. Extravascular hemolysis ŌĆó Occurs in macrophages of the spleen (and other organs). ŌĆó Predisposing factors: ŌĆō RBC membrane injury ŌĆō Reduced deformability ŌĆō Opsonization ŌĆó Principal clinical features are: ŌĆō Anemia, splenomegaly, and jaundice ŌĆō Modest reductions in haptoglobin ŌĆó a serum protein that binds hemoglobin
- 11. ContdŌĆ” ŌĆó Increased unconjugated bilirubin: jaundice. ŌĆó Increased stercobilinogen: dark colored stool. ŌĆó Increased urobilinogen: high colored urine. ŌĆó Increased iron store: iron released from heme stored in BM.
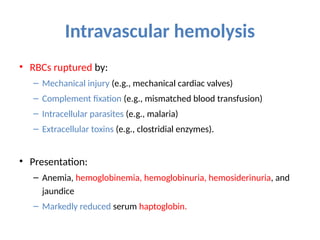
- 12. Intravascular hemolysis ŌĆó RBCs ruptured by: ŌĆō Mechanical injury (e.g., mechanical cardiac valves) ŌĆō Complement fixation (e.g., mismatched blood transfusion) ŌĆō Intracellular parasites (e.g., malaria) ŌĆō Extracellular toxins (e.g., clostridial enzymes). ŌĆó Presentation: ŌĆō Anemia, hemoglobinemia, hemoglobinuria, hemosiderinuria, and jaundice ŌĆō Markedly reduced serum haptoglobin.
- 13. ContdŌĆ” ŌĆó Characteristic findings of intra-vascular hemolysis: ŌĆō Hemoglobinemia ŌĆō Haemoglobinuria ŌĆō Haemosiderinuria ŌĆō S. Heptoglobin: decreased
- 14. Laboratory Findings ŌĆó Increase S. Bilirubun (Unconjugated). ŌĆó Increase Urine Urobilinogen. ŌĆó Increase rate of Bilirubin production. ŌĆó Increase S. LDH. ŌĆó Decrease life span of red cells. ŌĆó Decrease Heptoglobin.
- 15. Clinical Manifestations ŌĆó Clinical signs & symptoms depends upon: ŌĆō Severity of hemolysis. ŌĆō Duration of hemolysis. ŌĆó Manifestaions mostly seen in Chronic HA: ŌĆō Pallor ŌĆō Jaundice ŌĆō Splenomegaly ŌĆō Gall stones ŌĆō Skeletal abnormalities ŌĆō Leg ulcers
- 16. Compensatory Mechanisms To Hemolysis ŌĆó BM Erythroid hyperplasia: ŌĆō Chronic hemolysis --> Anaemia --> Increase in Erythropoietin --> BM erythroid hyperplasia. ŌĆō Reversal of M:E ratio. (2-4:1 --> 1:1-6). ŌĆó Reticulocytosis: ŌĆō BM erythroid hyperplasia --> rise in Reticulocytes. ŌĆō Mild: Hemoglobinopathies. ŌĆō Moderate to marked: IHA, HS, G6PD def.
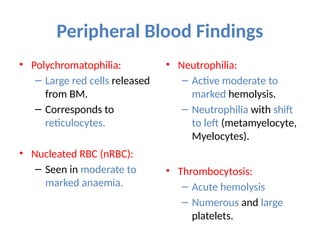
- 17. Peripheral Blood Findings ŌĆó Polychromatophilia: ŌĆō Large red cells released from BM. ŌĆō Corresponds to reticulocytes. ŌĆó Nucleated RBC (nRBC): ŌĆō Seen in moderate to marked anaemia. ŌĆó Neutrophilia: ŌĆō Active moderate to marked hemolysis. ŌĆō Neutrophilia with shift to left (metamyelocyte, Myelocytes). ŌĆó Thrombocytosis: ŌĆō Acute hemolysis ŌĆō Numerous and large platelets.
- 18. Morphologic Red Cell Abnormalities ŌĆó Provide clue to the underlying hemolytic conditions. ŌĆō Spherocytes ŌĆō Sickle cells ŌĆō Target Cells ŌĆō Schistocytes ŌĆō Acanthocytes
- 19. Fig: Marrow aspirate smear from a patient with hemolytic anemia. There is an increased number of maturing erythroid progenitors (normoblasts).
- 20. Structure of RBC Membrane
- 22. Hereditory Spherocytosis ŌĆó D/t cytoskeletal or membrane protein defects. ŌĆó Render RBCs spheroidal and less deformable ŌĆō Vulnerable to splenic sequestration and destruction. ŌĆó AD in 75% of patients.
- 23. Pathogenesis ŌĆó Insufficiency in several different proteins: spectrin, ankyrin, band 3, or band 4.2. ŌĆó Lead to reduced density of membrane skeletal components ŌĆō Reduced stability of the lipid bilayer. ŌĆō Loss of membrane fragments as RBCs age. ŌĆó Reduction in surface area ŌĆō RBCs assume a spheroidal shape. ŌĆó Diminished deformability. ŌĆō Propensity for being trapped and destroyed by splenic macrophages.
- 25. Fig: Reduced membrane stability in HS --> loss of RBC membrane --> formation of microspherocytes --> Ingested by splenic Macrophages.
- 26. Mechanism of Hemolysis in HS
- 27. Morphology ŌĆó Spherocytic RBCs are small and lack central pallor. ŌĆó Reticulocytosis and marrow erythroid hyperplasia. ŌĆó Marked splenic congestion with prominent erythrophagocytosis in the cords of Billroth.
- 28. Contd...
- 29. Clinical Features ŌĆó Diagnosis depends on: family history, hematologic findings, and increased RBC osmotic fragility ŌĆó MCHC increased: d/t cellular dehydration. ŌĆó Characteristic: Anemia, moderate splenomegaly, and jaundice. ŌĆó Clinical course: typically stable due to compensatory increases in erythropoiesis. ŌĆō Increased RBC turnover or diminished erythropoiesis can be problematic.
- 30. Contd... ŌĆó Parvovirus --> transient suppression of erythropoiesis --> Aplastic crisis ŌĆó Events that increase splenic RBC destruction ---> e.g., infectious mononucleosis --> trigger hemolytic crisis. ŌĆó 50% adults: chronic hyperbilirubinemia --> gallstones.
- 31. ???