Ophthalmic wound care assessment chart
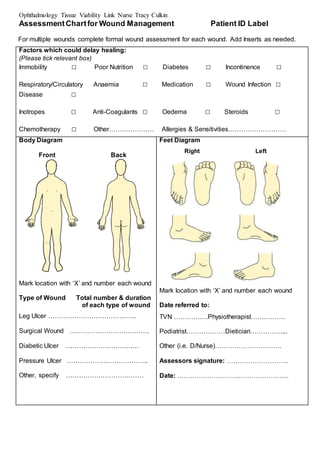
- 1. Ophthalmology Tissue Viability Link Nurse Tracy Culkin AssessmentChartfor Wound Management Patient ID Label For multiple wounds complete formal wound assessment for each wound. Add Inserts as needed. Factors which could delay healing: (Please tick relevant box) Immobility Ō¢Ī Poor Nutrition Ō¢Ī Diabetes Ō¢Ī Incontinence Ō¢Ī Respiratory/Circulatory Anaemia Ō¢Ī Medication Ō¢Ī Wound Infection Ō¢Ī Disease Ō¢Ī Inotropes Ō¢Ī Anti-Coagulants Ō¢Ī Oedema Ō¢Ī Steroids Ō¢Ī Chemotherapy Ō¢Ī OtherŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ” Allergies & SensitivitiesŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ” Body Diagram Front Back Mark location with ŌĆśXŌĆÖ and number each wound Type of Wound Total number & duration of each type of wound Leg Ulcer ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.. Surgical Wound ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”. Diabetic Ulcer ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.ŌĆ” Pressure Ulcer ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.. Other, specify ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ” Feet Diagram Right Left Mark location with ŌĆśXŌĆÖ and number each wound Date referred to: TVN ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.PhysiotherapistŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”. PodiatristŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”DieticianŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”... Other (i.e. D/Nurse)ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”. Assessors signature: ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.. Date: ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”..ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”...
- 2. Ophthalmology Tissue Viability Link Nurse Tracy Culkin Complete on initial assessment and thereafter complete at every dressing change Date of Assessment Number of wound Analgesia required (Refer to local pain assessment tool) Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Regular/ongoing analgesia Pre-dressing only Wound Dimensions (enter size) Length (cm/mm) Width (cm/mm) Depth (cm/mm) Or trace wound circumference Is wound tracking/undermining Photography Tissue type on wound bed ( enter percentages) Necrotic (Black) Sloughy (Yellow/Green) Granulating (Red) Epithelialising (Pink) Hypergranulating (Red) Haematoma Bone/tendon Wound exudate levels/ type (tick all relevant boxes) Low Moderate High * Serous (Straw) Haemoserous (Red/Straw) Purulent (Green/Brown/Yellow)* Peri-wound skin (tick relevant boxes) Macerated (White) Oedematous * Erythema (Red)* Excoriated (Red) Fragile Dry/scaly Healthy/intact Signs of Infection * 1 or more of these signs may indicate possible infection Heat * New slough/necrosis(deteriorating wound bed)* Increasing pain* Increasing exudate* Increasing odour* Friable granulation tissue* Treatment objectives (tick relevant box) Debridement Absorption Hydration Protection Palliative / conservative Reduce bacterial load
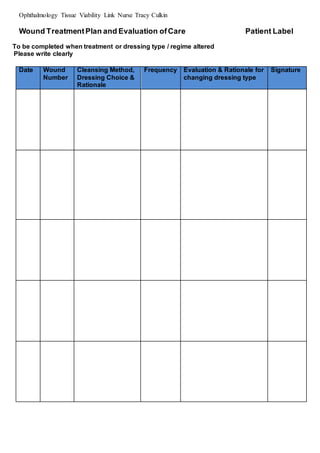
- 3. Ophthalmology Tissue Viability Link Nurse Tracy Culkin Wound TreatmentPlan and Evaluation ofCare Patient Label To be completed when treatment or dressing type / regime altered Please write clearly Date Wound Number Cleansing Method, Dressing Choice & Rationale Frequency Evaluation & Rationale for changing dressing type Signature
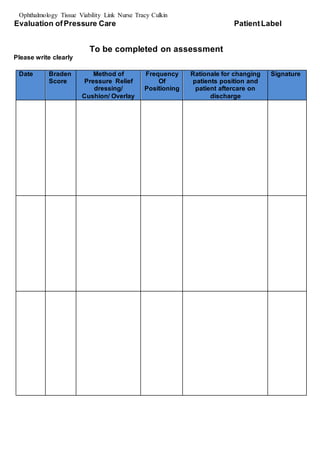
- 4. Ophthalmology Tissue Viability Link Nurse Tracy Culkin Evaluation ofPressure Care PatientLabel To be completed on assessment Please write clearly Date Braden Score Method of Pressure Relief dressing/ Cushion/ Overlay Frequency Of Positioning Rationale for changing patients position and patient aftercare on discharge Signature