Pancreatitis
- 1. Pancreatitis
- 2. Overview âĒ Pancreatitis is an inflammation of the gland parenchyma of the pancreas. âĒ It is divided into acute and chronic pancreatitis for clinical purpose.
- 3. Acute Pancreatitis ï A disorder of exocrine pancreas, associated with reversible pancreatic parenchyma cell injury with local and systemic inflammatory responses. ï Acute nonbacterial inflammatory condition caused by activation, interstitial liberation and auto-digestion of pancreas presenting as abdominal pain, associated with raised pancreatic enzyme levels in the blood or urine as a result of pancreatic inflammation. ï Mild or severe âĒ Mild acute pancreatitis is characterized by interstitial edema of the gland and minimal organ dysfunction. The mortality from which is around 1%. âĒ Severe acute pancreatitis is characterized by pancreatic necrosis, a severe systemic inflammatory response and often multi- organ failure. The mortality varies from 20-50%.
- 4. Aetiology of Acute Pancreatitis
- 5. Pathogenesis âĒ Autodigestion results from inappropriate release and activation of pancreatic enzymes is the final common pathway leading to pancreatitis.
- 7. Clinical Presentation âĒ Pain is the cardinal symptom. S- Diffuse, upper abdominal pain O- Sudden C- Boring pain R- Radiation of pain to the back and chest A- Nausea, vomiting, retching and hiccoughs T- Pain often rapidly escalated in intensity, peaking within about 10-20 min of onset and persists for hours/ days E- Aggravated by breathing with increased chest expansion; relieved by sitting or leaning forward (Muhammedan Prayer Sign) due to shifting forward of abdominal contents and taking pressure off from inflamed pancreas S- Depending on severity, patients may present with shock
- 8. Clinical Presentation âĒ Tachypnea, tachycardia and hypotension- features of shock âĒ Normal body temperature or low grade fever- seen in infective pancreas âĒ Jaundice â infrequently occur due to edema of the head of pancreas âĒ Cyanosis â improper lung perfusion âĒ Mild icterus- biliary obstruction in gallstones pancreatitis âĒ Erythematous skin nodules â due to subcutaneous fact necrosis âĒ Abdominal findings: - Abdominal tenderness, guarding and distension - Mass in epigastrium - Cullenâs sign ( bluish discolouration of the umbilicus) - Grey Turnerâs sign (bluish discolouration of the flanks)
- 10. Ransonâs and Glasgowâs Criteria âĒ Used to predict severity of acute pancreatitis. âĒ It is classified as severe when 3 or more factors are present.
- 11. Acute Physiology and Chronic Health Evaluation (APACHE II)
- 12. Diagnostic criteria âĒ Most often established by the presence of two of the three following criteria: (i) abdominal pain consistent with the disease, (ii) serum amylase and/or lipase greater than three times the upper limit of normal, and/or (iii) characteristic ïŽndings from abdominal imaging. âĒ CT and/or MRI of the pancreas should be reserved for patients ïž in whom the diagnosis is unclear(typical pain with normal enzymes) ïž who fail to improve clinically within the ïŽrst 48â72 h after hospital admission (e.g., persistent pain, fever, nausea, unable to begin oral feeding) ïž to evaluate complications
- 14. Management of Mild Acute Pancreatitis âĒ Conservative Approach âĒ Admit in general ward âĒ Non invasive monitoring âĒ IV fluid administration âĒ A brief period of fasting in patient who is nauseated and in pain; oral fluids, soft diet by 3-4 days once pain and ileus settle down âĒ Analgesia and anti-emetics âĒ Monitoring for any signs of early organ failure âĒ Oxygen supplementation for hypoxemia âĒ CT scan when there is evidence of deterioration âĒ Admission to ICU/HDU when the stable patient meets the prognostic criteria for severe attack of pancreatitis *No antibiotics
- 15. Management of Severe Acute Pancreatitis âĒ Aggressive Approach âĒ Admit in HDU/ICU âĒ Analgesia âĒ Aggressive fluid rehydration âĒ Oxygenation âĒ Invasive monitoring of vital signs, central venous pressure, urine output, blood gases âĒ Frequent monitoring of hematological and biochemical parameters ( including liver and renal function, clotting, serum calcium, blood glucose) âĒ Nasogastric drainage âĒ Antibiotic prophylaxis can be considered (imipenem, cefuroxime) âĒ CT scan essential if organ failure, clinical deterioration or signs of sepsis develop âĒ ERCP within 72 hours for severe gallstone pancreatitis or signs of cholangitis âĒ Supportive therapy for organ failure if it develops (inotropes, ventilatory support, haemofiltration, etc.) âĒ If nutritional support is required, consider enteral (nasogastric feeding)
- 17. Chronic pancreatitis ïA continuing inflammatory disease of the pancreas characterized by irreversible morphological change typically causing pain and/or permanent loss of function. ïAssociated with recurrent inflammation, fibrosis, and injury to the exocrine and endocrine tissues. ïPainful exacerbation or completely painless.
- 19. Pathogenesis of Chronic Pancreatitis
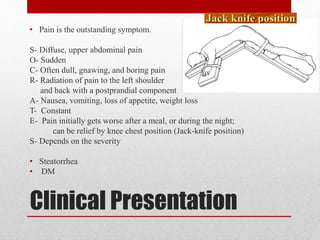
- 20. Clinical Presentation âĒ Pain is the outstanding symptom. S- Diffuse, upper abdominal pain O- Sudden C- Often dull, gnawing, and boring pain R- Radiation of pain to the left shoulder and back with a postprandial component A- Nausea, vomiting, loss of appetite, weight loss T- Constant E- Pain initially gets worse after a meal, or during the night; can be relief by knee chest position (Jack-knife position) S- Depends on the severity âĒ Steatorrhea âĒ DM
- 22. Endoscopic, Radiological or surgical Interventions of Chronic Pancreatitis âĒ Indicated to relieve obstruction and remove mass lesion of the pancreatic duct, bile duct or the duodenum, or in dealing with complications. âĒ To provide pain relief by decompressing an obstructed pancreatic duct.
- 23. Endoscopic, Radiological or surgical Interventions of Chronic Pancreatitis âĒ Endoscopic pancreatic sphincterotomy- papillary stenosis, high sphincter pressure and pancreatic ductal pressure âĒ Stent placement- pancreatic duct stricture and upstream dilatation âĒ Endoscopic retrograde cholangiopancreatography (ERCP)- pancreatic duct stones âĒ Percutaneous or transgastric drainage under endoscopic ultrasound (EUS) or CT guidance-pseudocysts âĒ Pancreatoduodenectomy or Beger procedure (duodenum-preserving resection of the pancreas head) - mass in the head of the pancreas âĒ Longitudinal pancreatojejunostomy or Frey procedure if the pancreatic is markedly dilated. âĒ Distal pancreatectomy- disease limited to the tail of the pancreas âĒ Subtotal or total pancreatectomy- intractable pain and diffuse disease with nondilated ducts âĒ Total pancreatectomy and islet autotransplantation- to avoid long-term morbidity caused by diabetes ; involves harvesting the islets from the resected pancreas and injecting them into the portal system, which then lodges them in the liver.
- 24. Differential Diagnosis of Chronic Pancreatitis âĒ Ampullary Carcinoma âĒ Cholangitis âĒ Cholecystitis âĒ Chronic Gastritis âĒ Community-Acquired Pneumonia âĒ Crohn Disease âĒ Intestinal Perforation âĒ Mesenteric Artery Ischemia âĒ Myocardial Infarction âĒ Pancreatic Cancer âĒ Peptic Ulcer Disease
- 25. Q&A 1. Following are features of acute pancreatitis except A. Shock B. Cullenâs sign C. Grey Turnerâs sign D. Kehr sign 2. The best surgical treatment for chronic pancreatitis with dilated duct is A. Freyâs operation B. Whippleâs operation C. Longitudinal pancreaticojejunostomy D. Distal pancreatectomy
- 26. References âĒ Bailey & Love's short practice of surgery By: Williams, Norman S., and C. J. K. Bulstrode. Hodder Arnold 2008 âĒ Manipal manual of surgery By: Shenoy, K. Rajgopal. CBS Publishers & Distributors, 2000 âĒ Robbins and Cotran pathologic basis of disease By: Robbins, Stanley L.. Saunders/Elsevier 2010 âĒ http://annals.org/data/Journals/AIM/20218/tt2.png
Editor's Notes
- carefully monitored for any signs of early organ failure such as hypotension, vital signs and urinary output.
- 1. D 2. C