PATHOLOGY - Arteriosclerosis
- 2. ARTERIOSCLEROSIS DEF: -hardening of the arteries -generic term reflecting arterial wall thickening and loss of elasticity THREE GENERAL PATTERNS: 1. Arteriolosclerosis 2. Monckeberg medial sclerosis 3. Atherosclerosis
- 3. 1. Arteriolosclerosis -affects small arteries and arterioles -anatomic variants: a. hyaline b. hyperplastic
- 4. 2. Monckeberg medial sclerosis -has calcific deposits in muscular arteries that may undergo metaplasia to bone -lesions do not encroach vessel lumen thus NOT CLINICALLY SIGNIFICANT
- 5. 3. Atherosclerosis -most frequent and clinically important pattern -characterized by intimal lesions called ATHEROMAS that protrude into the vessel lumen -consists of a raised lesion: a. Grumuous Core ŌĆō made of lipid, (cholesterol or cholesterol ester) yellow, soft b. Fibrous Cap ŌĆō white
- 6. 3. Atherosclerosis EPIDEMIOLOGY -Risk factors have a multiplicative effect -Constitutional Risk Factors in IHD a. Age ŌĆō clinically manifests middle age or later b. Gender ŌĆō premenopausal women are relatively protected due to favorable influence of estrogen -but clinical trials have failed to demonstrate any utility of hormonal therapy for vascular diseases prevention a. Genetics ŌĆō MOST SIGNIFICANT INDEPENDENT RISK FACTOR
- 7. 3. Atherosclerosis EPIDEMIOLOGY -Modifiable Risk Factors in IHD a. Hyperlipidemia ŌĆō esp. hypercholesterolemia, increased LDL, decreased HDL, increased lipoprotein a *STATINS ŌĆō a class of drugs that lower circulating cholesterol levels by inhibiting HMG-Coa reductase, the rate-limiting enzyme in hepatic cholesterol biosynthesis
- 8. 3. Atherosclerosis EPIDEMIOLOGY -Modifiable Risk Factors in IHD b. Hypertension ŌĆō both systolic and diastolic components are important - MOST IMPORTANT CAUSE OF LEFT VENTRICULAR HYPERTROPHY c. Cigarette smoking ŌĆō prolonged smoking of one pack of cigarettes or more daily doubles the death rate from IHD
- 9. 3. Atherosclerosis EPIDEMIOLOGY -Modifiable Risk Factors in IHD d. Diabetes mellitus ŌĆō induces hypercholesterolemia
- 10. 3. Atherosclerosis EPIDEMIOLOGY -Additional Risk Factors a. Inflammation ŌĆō present during all stages of atherogenesis and is intimately linked with atherosclerotic plaque formation and rupture *C-reactive Protein (CRP) has emerged as one of the simplest and most sensitive inflammatory markers; decreased by STATINS
- 11. 3. Atherosclerosis EPIDEMIOLOGY -Additional Risk Factors b. Hyperhomocysteinemia ŌĆō seen in CAD, PAD, stroke and venous thrombosis -elevated homocysteine levels can be caused by low folate and Vitamin B12 intake c. Metabolic syndrome
- 12. 3. Atherosclerosis EPIDEMIOLOGY -Additional Risk Factors d. Lipoprotein (a) ŌĆō an altered form of LDL, associated with CAD and CVD e. Factors affecting Hemostasis f. Other Factors ŌĆō lack of exercise; competitive stressful lifestyle (type A personality); obesity
- 13. 3. Atherosclerosis PATHOGENESIS Hypotheses: a. Intimal Cellular Proliferation b. Repetitive Formation and Organization of Thrombi c. Response-To-Injury -views atherosclerosis as a chronic inflammatory and healing response of the arterial wall to injury -lesion progression occurs through the interaction of modified lipoproteins, monocyte-derived macrophages, and T-lymphocytes with the normal cellular constituents of the arterial wall
- 14. 3. Atherosclerosis PATHOGENESIS c. Response-To-Injury -PATHOGENIC EVENTS INVOLVED: i. Endothelial Injury -increased vascular permeability -leukocyte adhesion -thrombosis ii. Accumulation of Lipoproteins in vessel wall -usually LDL and its oxidized forms iii. Monocyte adhesion to the endothelium, followed by migration into the intima and transformation into macrophages and foam cells
- 15. 3. Atherosclerosis PATHOGENESIS c. Response-To-Injury -PATHOGENIC EVENTS INVOLVED: iv. Platelet adhesion v. Factor release from activated platelets, macrophages and vascular wall cells, inducing smooth muscle cell recruitment vi. Smooth muscle cell proliferation and ECM production vii. Lipid accumulation -extracellular and within cells (macropahes and smooth muscle cells)
- 16. 3. Atherosclerosis PATHOGENESIS MAJOR MECHANISMS +Endothelial Cell Injury -results in intimal thickening -early human lesions begin at sites of morphologically intact endothelium, THUS, endothelial dysfunction underlies human atherosclerosis -can be caused by: -hypertension -hyperlipidemia -toxins from cigarette smoke -infectious agents -inflammatory cytokines -homocysteine
- 17. 3. Atherosclerosis PATHOGENESIS MAJOR MECHANISMS +Endothelial Cell Injury 2 MOST IMPORTANT CAUSES OF ENDOTHELIAL DYSFUNCTION -hemodynamic disturbances -hypercholesterolemia
- 18. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Hemodynamic Disturbances -plaques tend to occur at areas of disturbed flow patterns: a. Ostia of exiting vessels b. Branch points c. Along the Posterior wall of the abdominal aorta
- 19. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Hemodynamic Disturbances -nonturbulent laminar flow in normal vasculature leads to the induction of endothelial genes whose products protect against atherosclerosis e.g. SUPEROXIDE DISMUTASE
- 20. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Lipids -Lipoprotein abnormalities present in many MI survivors: -Increased LDL -Decreased HDL - Increased Lipoprotein (a) -DOMINANT LIPIDS IN ATHEROMATOUS PLAQUES ARE: -Cholesterol -Cholesterol Esters
- 21. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Lipids -Lowering serum cholesterol by diet or drugs slows the rate of progression of atherosclerosis, causes regression of some plaques, and reduces the risk of cardiovascular events
- 22. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Lipids -Mechanisms by which HYPERLIPIDEMIA contributes to ATHEROGENESIS: -impair endothelial cell function by increasing local oxygen free radical production -accumulate lipoproteins within the intima, which are then oxidized by oxygen free radicals
- 23. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Lipids -Oxidized LDL is ingested by macrophages through a SCAVENGER RECEPTOR, distinct from LDL receptor -MACROPHAGES become FOAM CELLS after accumulation of Oxidized LDL within the phagocyte
- 24. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Inflammation -dysfunctional arterial endothelial cells express adhesion molecules that encourage leukocyte adhesion -VCAM1 ŌĆō binds monocytes and T cells -Monocyte recruitment and differentiation is theoretically protective because they remove harmful lipid particles, but the presence of OXIDIZED LDL AUGMENTS Macrophage activation and cytokine production
- 25. 3. Atherosclerosis PATHOGENESIS +Endothelial Cell Injury *Infection -Microorganisms detected in atherosclerotic plaques: -Herpesvirus -Cytomegalovirus -Chlamydiae pneumoniae
- 26. 3. Atherosclerosis PATHOGENESIS +Smooth Muscle Proliferation -intimal smooth muscle cell proliferation and ECM deposition convert a fatty streak into a mature atheroma *FATTY STREAK = EARLIEST LESION -Growth Factors involved: -PDGF -FGF -TGF-a
- 27. 3. Atherosclerosis PATHOGENESIS +Smooth Muscle Proliferation -Smooth muscle cells synthesize ECM that stabilizes atherosclerotic plaques - Active Inflammatory cells in atheromas can cause intimal smooth muscle cell apoptosis, and increase ECM catabolism leading to unstable plaques
- 28. 3. Atherosclerosis MORPHOLOGY *FATTY STREAKS -EARLIEST LESIONS IN ATHEROSCLEROSIS -begin as minute, flat yellow spots and then colaesce -not significantly raised and do not cause flow disturbance -virtually in all children older than 10 years -coronary fat streaks begin to form in adolescence, at the same anatomic sites that later tend to develop plaques
- 29. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -KEY PROCESSES: Intimal Thickening & Lipid Accumulation -Gross: -Color: White or Yellow (Ulcerated Plaques: Red- brown) -Size: 0.3-1.5 cm in diameter (can coalesce) -In humans, the ABDOMINAL AORTA affected MORE than THORACIC AORTA
- 30. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -Commonly involved Vessels (Descending Order): 1. Lower Abdominal Aorta 2. Coronary Arteries 3. Popliteal Arteries 4. Internal Carotid Arteries 5. Circle of Willis
- 31. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -Principal Components (CEL): 1. Cells -smooth muscle cells, macrophages, T cells 2. ECM -collagen, elastic fibers, proteoglycans 3. Lipids -intracellular and extracellular
- 32. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -Configuration: 1. Fibrous cap ŌĆō superficial; made of smooth muscle cells, collagen 2. Shoulder ŌĆō beneath and to the side of the cap; more cellular with macrophages, T cells, smooth muscle cells 3. Necrotic core ŌĆō deep into cap, made of lipid primarily cholesterol and cholesterol esters, debris from dead cells, foam cells, fibrin, thrombus, other plasma proteins
- 33. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -The periphery of the lesions show neovascularization -Plaques enlarge due to: 1. Cell death and degenration 2. Synthesis and degradation of ECM 3. Organization of thrombus -Atheromas often undergo CALCIFICATION
- 34. 3. Atherosclerosis MORPHOLOGY *ATHEROSCLEROTIC PLAQUE -Plaques are susceptible to the following CLINICAL CHANGES: 1. Rupture, ulceration, erosion 2. Hemorrhage into a plaque 3. Atheroembolism 4. Aneurysm formation
- 35. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE -Large Elastic and Large and Medium Muscular arteries are the MAJOR TARGETS of ATHEROSCLEROSIS -Smaller vessels can become occluded, compromising distal tissue perfusion -Ruptured plaque can embolize atherosclerotic debris and cause distal vessel obstruction, or can lead to acute thrombosis -Destruction of the underlying vessel wall can lead to aneurysm formation, which can rupture and/or be a thrombi
- 36. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ATHEROSCLEROTIC STENOSIS -plaques can gradually occlude vessel lumens, compromising blood flow causing ischemic injury -outward remodeling preserves lumen diameter -effects of vascular occlusion depend on arterial supply and metabolic demand of affected tissue
- 37. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ACUTE PLAQUE CHANGE -plaque erosion or rupture is typically promptly followed by partial or complete vascular thrombosis resulting in acute tissue infarction -THREE CATEGORIES OF PLAQUE CHANGES: 1. Rupture/Fissuring ŌĆō exposing thrombogenic constituents 2. Erosion/Ulceration ŌĆō exposing subendothelial basement membrane to blood 3. Hemorrhage into the atheroma
- 38. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ACUTE PLAQUE CHANGE -the precipitating lesion in patients who develop MI or other coronary syndromes is NOT NECESSARILY a severely stenotic and hemodynamically significant lesion BEFORE ITS ACUTE CHANGE
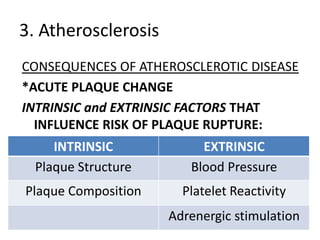
- 39. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ACUTE PLAQUE CHANGE INTRINSIC and EXTRINSIC FACTORS THAT INFLUENCE RISK OF PLAQUE RUPTURE: INTRINSIC EXTRINSIC Plaque Structure Blood Pressure Plaque Composition Platelet Reactivity Adrenergic stimulation
- 40. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ACUTE PLAQUE CHANGE VULNERABLE Plaques: -contain large areas of foam cells and extracellular lipids -with thin fibrous caps *collagen represents the major structural component of the fibrous cap and accounts for its mechanical strength and stability -contain few smooth muscle cells -have clusters of inflammatory cells *STATINS stabilize plaques by reducing plaque inflammation
- 41. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *ACUTE PLAQUE CHANGE -Peak time of onset of acute myocardial infarction is between 6 AM and 12 NOON
- 42. 3. Atherosclerosis CONSEQUENCES OF ATHEROSCLEROTIC DISEASE *THROMBOSIS *VASOCONSTRICTION -compromises lumen size and by increasing local mechanical forces can potentiate plaque disruption -stimulated by: 1. Adrenergic agonists 2. Local platelet contents 3. impaired secretion of cell relaxing factors 4. mediators released from perivascular inflammtory cells