Percutaneous closure of atrial septal defect 3
- 1. Presented by: Dr. Ibdah
- 2. ’üĮ 65 year old patient ,female ’üĮ c/o : SOB, occasional palpitations ’üĮ TEE: ASD II , Left to Right Shunt. Diameter of defect 14 mm . RV dilated with signs of volume overloading ’üĮ Right heart Catheterization: PA sys 36mmHg PVR 61 dyn/cm5 ’üĮ Balloon sizing :
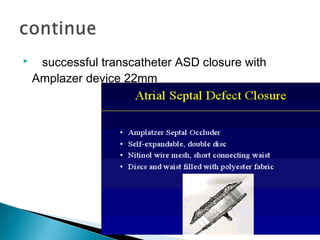
- 4. ’üĮ successful transcatheter ASD closure with Amplazer device 22mm
- 5. ’üĮ Common 3-10% of CHD ’üĮ Classification: ASD I, ASD II 70%, sinus venosus ’üĮ Female > Male ’üĮ Pathophsiology : initially left to right shunt ’üĮ Clinical features and diagnostic evaluation: are not the scope of this presentation!
- 6. ’üĮ Three questions crystallize the debate : 1. Who should have their ASD closed? 2. When should it be closed? 3. How should it be closed?
- 7. ’üĮ Any patient with dilated RV or RA by Echo,MRT or CT ’üĮ any ASD ( in the absence of of advanced pulmonary HTN) with one or more of following: 1. ASD > 10 mm on TEE 2. Qp:Qs > 1.5:1
- 8. ’üĮ Yes close it and yes do it as soon as possible ! ’üĮ Is the age matter ? The answer is NO
- 9. ’üĮ The defect too small ’āĀfollow them periodically ’üĮ Severe pulmonary arterial HTN ; do not close ! ASD acts here as ``pop-off`` valve ’üĮ Pregnancy ’āĀ defer 6 months after delivery ’üĮ Severe LV dysfunction . Again ASD functioning as`` pop-off`` valve
- 11. ’āś Device closure is a safe and effective procedure in experienced hands ’āś Advantages of device closure : less hospital stay, avoidance surgical wounds, same hemodynamic benefit as by surgery ’āś Drawbacks: large defect > 36 mm, septal rim less than 5 mm, proximity of defect to AV ,CS,IVC,SVC
- 12. Successful closure achieved in 95 % of Pt. ’üĮ Tachyarrhythmia 1-4%’āĀ follow up , ablation ’üĮ Brady arrhythmia ’āĀ Pacing ’üĮ Device migration and erosion : catastrophic but rare 0,1 %related to operator experience and over sizing ’üĮ Right heart failure or progressive pulmonary HTN ; related to the age of patient at the time of closure ’üĮ Thrombosis 1.2 %: maximal at 4 weeks ,rare with dual therapy era ’üĮ Nickel allergy ! Chest pain at next day ’āĀ do skin test if positive ’āĀ remove the device
- 13. ’üĮ Small: common after catheter closure ,close spontaneously after 1 year ’üĮ Large : false measurement, dehisced ASD device
- 14. ’üĮ Dual antiplatelet therapy 6 months ’üĮ TTE next day . ’üĮ TEE in 1,6 and in 12 months ’üĮ IE-prophylaxis for 6 months
- 15. ’üĮ Majority of ASD II are device closable ’üĮ Safe and effective procedure ’üĮ need for excellent pre-procedure work up
- 16. Thank you for your attention