Peripheral nerve injuries by Dr.Harishma R.pdf
- 2. • These are formed from nerves arising from the spinal cord (spinal nerves). • There are 31 pairs of spinal nerves in the body, each representing a segment of the spinal cord. • Through direct branching or through a network of nerves (plexus), give rise to peripheral nerves. • Peripheral nerves are mixed nerves carrying motor, sensory and autonomous supply to the limbs. PERIPHERAL NERVE
- 3. STRUCTURE OF A PERIPHERAL NERVE • An individual nerve fi bre is enclosed in a collagen connective tissue known as endoneurium. • A bundle of such nerve fi bres are further bound together by fi brous tissue to form a fasciculus. The binding fi brous tissue is known as perineurium. • A number of fasciculi are bound together by a fi brous tissue sheath known as epineurium. • An individual nerve, therefore, is a bundle of a number of fasciculi.
- 4. A p a tient with a nerve injury commonly presents with compl a ints of In a bility To Move A P a rt Of The Limb We a kness Numbness. History
- 5. CAUSE History OBVIOUS • penetr a ting wound a long the course of a peripher a l nerve • nerve injury m a y occur during a n oper a tion a s a result of stretching or direct injury NOT OBVIOUS • History of injection in the proximity of the nerve. • Neurotoxic drugs such a s quinine a nd tetr a cyclines. • Medic a l c a uses - leprosy, di a betes
- 6. MECHANISM OF INJURY MCC - Fractures and dislocations Mechanisms by which a nerve may be damaged are: • Direct Injury • Infections • Mechanical Injury • Cooling And Freezing • Thermal Injury • Electrical Injury • Ischaemic Injury • Toxic Agents • Radiation
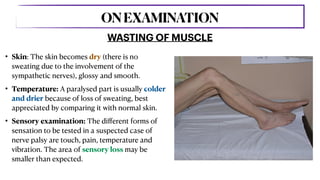
- 7. • Skin: The skin becomes dry (there is no sweating due to the involvement of the sympathetic nerves), glossy and smooth. • Temperature: A paralysed part is usually colder and drier because of loss of sweating, best appreciated by comparing it with normal skin. • Sensory examination: The di ff erent forms of sensation to be tested in a suspected case of nerve palsy are touch, pain, temperature and vibration. The area of sensory loss may be smaller than expected. WASTING OF MUSCLE ONEXAMINATION
- 8. • Re fl exes: Re fl exes are absent in cases of peripheral nerve injuries. • Sweat test: This is a test to detect sympathetic function in the skin supplied by a nerve. Sympathetic fi bres are among the most resistant to mechanical trauma. Sweating can be determined by the starch test or ninhydrin print test. In these tests, the extremity is dusted with an agent that changes colour on coming in contact with sweat. WASTING OF MUSCLE ONEXAMINATION
- 9. • Motor examination: The muscles which are exclusively supplied by a particular nerve are most suitable for motor examination. The tests are nothing but manoeuvres to make a muscle contract. The contraction of the muscle must be appreciated, wherever possible, by feeling its belly or its tendon getting taut. WASTING OF MUSCLE ONEXAMINATION
- 10. We Will Discuss Individual Nerve Injury…
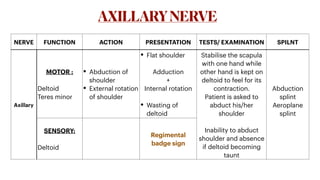
- 11. NERVE FUNCTION ACTION PRESENTATION TESTS/ EXAMINATION SPILNT Axillary MOTOR : Deltoid Teres minor • Abduction of shoulder • External rotation of shoulder • Flat shoulder Adduction + Internal rotation • Wasting of deltoid Stabilise the scapula with one hand while other hand is kept on deltoid to feel for its contraction. Patient is asked to abduct his/her shoulder Inability to abduct shoulder and absence if deltoid becoming taunt Abduction splint Aeroplane splint SENSORY: Deltoid Regimental badge sign AXILLARYNERVE
- 12. AXILLARYNERVE
- 13. NERVE FUNCTION ACTION PRESENTATION Musculocutaneous MOTOR Coracobrachialis Brachialis Biceps brachii • Flexion of the arm at elbow • Supination of the forearm Weak f lexion at shoulder Weak supination Wasting of biceps SENSORY: Lat. aspect of forearm Sensory loss along the lateral side of the forearm MUSCULOCUTANEOUSNERVE
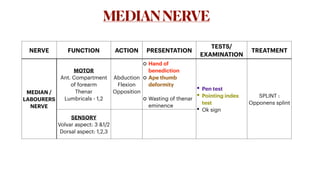
- 14. NERVE FUNCTION ACTION PRESENTATION TESTS/ EXAMINATION TREATMENT MEDIAN / LABOURERS NERVE MOTOR Ant. Compartment of forearm Thenar Lumbricals - 1,2 Abduction Flexion Opposition Hand of benediction Ape thumb deformity Wasting of thenar eminence • Pen test • Pointing index test • Ok sign SPLINT : Opponens splint SENSORY Volvar aspect: 3 &1/2 Dorsal aspect: 1,2,3 MEDIANNERVE
- 16. NERVE MUSCLES SUPPLIED ACTION PRESENTATION TESTS/ EXAMINATION SPLINT ULNAR/ MUSICIAN NERVE MOTOR: Hypothenar Lumbricals 3,4 Flexor carpi ulnaris Flexor digitorum profundus Palmar and dorsal interossei • Finger adduction and abduction other than thumb • Thumb adduction • Flexion of 4,5 digits • Flexion of wrist and adduction Claw hand deformity Wasting of hypothenar eminence and intrinsic muscles of hand 1. Card test 2. Egawa tes 3. Book test Knuckle bender splint SENSORY: Medial 1 1/2 ULNARNERVE
- 19. NERVE MUSCLES SUPPLIED ACTION PRESENTATION SPLINT RADIAL NERVE MOTOR: Post. Compartment of arm - triceps brachia Post. Compartment of forearm Wrist extensors Finger extensors Brachioradials Supinator Extension of elbow, wrist and f ingers • Wrist drop • Finger drop • Thumb drop • Wasting of triceps and post. Compartment of forearm Cock up SENSORY: Lower post. Arm, post. Forearm, lat. 2/3 dorsum of hand, proximal dorsal aspect of lat. 3 1/2 f ingers RADIALNERVE
- 21. MUSCLES SUPPLIED : Serratus anterior muscle LONGTHORACICNERVEPALSY • Winging of scapula • The vertebral border of the scapula becomes prominent when the patient tries to push against a wall.
- 22. NERVE BRANCHES MUSCLES SUPPLIED ACTION PRESENTATION SPLINT SCIATIC Common peroneal nerve Extensors Evertors of foot Evertion of foot High step gait Foot drop / ankle foot orthosis splint Tibial nerve Plantar Flexors of foot Plantar f lexion of foot SCIATICNERVEINJURY
- 24. Neurapraxia • It is a physiological disruption of conduction in the nerve fi bre. • No structural changes occur. • Recovery occurs spontaneously within a few weeks, and is complete. Axonotmesis • The axons are damaged but the internal architecture of the nerve is preserved. Wallerian degeneration occurs. • Recovery may occur spontaneously but may take many months. • Complete recovery may not occur. Neurotmesis • The structure of a nerve is damaged by actual cutting or scarring of a segment. • Wallerian degeneration occurs. • Spontaneous recovery is not possible, and nerve repair is required.
- 26. Nerve degeneration Dist a l to the point of injury - second a ry or W a lleri a n degener a tion The proxim a l p a rt - prim a ry or retrogr a de degener a tion upto a single node.
- 27. Nerve Regeneration As regeneration begins, the axonal stump from the proximal segment begins to grow distally. The r a te of recovery of a xon is 1 mm per d a y • If the, the axonal sprout may readily pass along its primary course and re-innervate the end- organ. • motor march • The sprouts, as many as 100 from one axonal stump, may migrate aimlessly throughout the damaged area into the epineural, perineural or adjacent tissues to form an end-neuroma or a neuroma in continuity Endoneural Tube With Its Contained Schwann Cells Is Intact Endoneural Tube Is Interrupted
- 28. SIGNSOFREGENERATION Whenever a c a se of nerve injury is seen some time a fter the injury or following a rep a ir, signs of regener a tion of the nerve should be looked for during ex a min a tion • Tinel's sign • Motor examination • Electrodiagnostic test
- 29. Electromyography • Electromyography (EMG) is a graphic recording of the electrical activity of a muscle at rest and during activity. • Electromyography is useful in deciding the following: a)  Whether or not a nerve injury is present b)  Whether it is a complete or incomplete nerve injury c) Whether any regeneration occurring d) Level of nerve injury ELECTRODIAGNOSTIC STUDIES DIAGNOSIS
- 30. Nerve conduction studies • It is a measure of the velocity of conduction of impulse in a nerve. • A stimulating electrode is applied over a point on the nerve trunk and the response is picked up by an electrode at a distance or directly over the muscle. • The normal nerve conduction velocity of motor nerve is 70 metres/second. • This conduction study helps in the following: a)  Whether a nerve injury is present 
 b)  Whether it is a complete or partial nerve injury 
 c)  Compressive lesion ELECTRODIAGNOSTIC STUDIES DIAGNOSIS
- 31. TREATMENT Conserv a tive or Oper a tive CONSERVATIVE TREATMENT The aim of conservative treatment is to preserve the mobility of the a ff ected limb while the nerve recovers. The following are the essential components of conservative treatment: • Splintage of the paralysed limb • Preserve mobility of the joints • Care of the skin and nails • Physiotherapy: Physiotherapeutic measures consist of (i) massage of the paralysed muscles; (ii) passive exercises to the limb; (iii) building up of the recovering muscles; and (iv) developing the una ff ected or partially a ff ected muscles. • Relief of pain
- 32. Operative procedures for nerve injuries consist of nerve repair, neurolysis, and tendon transfers. OPERATIVE TREATMENT Nerve rep a ir It may be performed within a few days of injury (primary repair) or later (secondary repair). Primary repair: • It is indicated when the nerve is cut by a sharp object, and the patient reports early (immediate primary repair is the best) • In case the wound is contaminated or the patient reports late, a delayed primary repair is better. In this, in the fi rst stage, the wound is debrided and the two nerve ends approximated with one or two fi ne silk sutures so as to prevent retraction of the cut ends. This also makes identi fi cation of the cut ends easy at a later date. • After two weeks, once the wound heals, a de fi nitive repair is done. Some surgeons routinely perform a delayed primary repair because they feel that the epineurium gets thickened in two weeks and sutures hold better.
- 33. Secondary repair: It is indicated for the following cases: a)  Nerve lesions presenting some time after injury: Often nerve injuries are missed at the time of injury, or it may not have been possible to treat them early for reason, such as poor general condition of the patient. 
 b)  Syndrome of incomplete interruption: If no de fi nite improvement occurs in 6 weeks in cases with an apparently incomplete nerve injury, nerve exploration, and if required secondary repair should be carried out. 
 c)  Syndrome of irritation: Cases with signs of nerve irritation need exploration and sometimes a secondary repair. 
 d) Failure of conservative treatment: If a nerve injury is treated conservatively and no improvement occurs within 3 weeks, one should proceed to electrodiagnostic studies, and if required, nerve exploration. Nerve rep a ir It may be performed within a few days of injury (primary repair) or later (secondary repair).
- 34. Techniques of nerve repair Nerve suture When the nerve ends can be brought close to each other, they may be sutured by one of the following techniques: • Epineural suture • Epi-perineural suture • Perineural suture • Group fascicular repair Nerve rep a ir c a n be either end-to-end or by using a nerve gr a ft.
- 35. Methods of closing nerve gaps Sometimes, the loss of nerve tissue is so much, that an end-to-end suture cannot be obtained. In such a situation, the following measures are adopted to gain length and achieve an end-to-end suture: • Mobilisation of the nerve on both sides of the lesion. • Relaxation of the nerve by temporarily positioning the joints in a favourable position. • Alteration of the course of the nerve, e.g. the ulnar nerve may be brought in front of the medial epicondyle (anterior transposition). • Stripping the branches from the parent nerve without tearing them. • Sacri fi cing some unimportant branch if it is hampering nerve mobilisation. Techniques of nerve repair Nerve rep a ir c a n be either end-to-end or by using a nerve gr a ft.
- 36. b) Nerve grafting: • When the nerve gap is more than 10 cm or end-to-end suture is likely to result in tension at the suture line, nerve grafting may be done. • In this, an expandable nerve (the sural nerve) is taken and sutured between two ends of the original nerve. • Techniques of nerve repair Nerve rep a ir c a n be either end-to-end or by using a nerve gr a ft.
- 37. Reconstructive surgery: These are operations performed when there is no hope of the recovery of a nerve, usually after 18 months of injury. Operations included in this group are tendon transfers, arthrodesis and muscle transfer. Rarely, an amputation may be justi fi ed for an anaesthetic limb or the one with causalgia. Neurolysis: This term is applied to the operation where the nerve is freed from enveloping scar (perineural fi brosis). This is called external neurolysis. In many cases, the nerve sheath may be dissected longitudinally to relieve the pressure from the fi brous tissue within the nerve (intra-neural fi brosis). This is called internal neurolysis.
- 38. PROGNOSIS The following f a ctors dict a te recovery following a nerve rep a ir: GOOD PROGNOSIS BAD PROGNOSIS Younger Age Older age A primarily motor nerve, like radial nerve, has a better prognosis than a mixed nerve. The more the tension at the suture line,the poorer the prognosis Neuropraxia 18 months since injury only sensory functions can be expected. Early repair The more proximal the injury, the worse the prognosis. The more the crushing and infection, the poorer the prognosis. Associated conditions: Infection, ischaemia
- 39. 

 ந ன்றி … REFERENCE 1. Essential Orthopaedics - 5th edition 2. Schwartz principles of surgery - 11th edition