Physiological changes in pregnancy.ppt
Download as PPT, PDF0 likes39 views
Physiological changes in pregnancy result in profound anatomical, physiological, and biochemical adaptations throughout a woman's body to support the growth of the fetus. These changes include increased blood volume, cardiac output, and blood flow to key organs. Respiratory function also adapts with increased tidal volume and minute ventilation. While these changes are normal and vital for a healthy pregnancy, they can also mimic or worsen underlying health conditions. It is important for healthcare providers to understand these adaptations in order to avoid misinterpreting them as signs of disease during pregnancy.
1 of 19
Download to read offline

















Recommended
physiology pregnancy copy.pptx



physiology pregnancy copy.pptxsushmagupta67
Ěý
Physiological changes in pregnancy include increased cardiac output, intravascular volume, and respiratory rate. The enlarging uterus displaces organs and compresses blood vessels. This leads to decreased lung volumes and increased risk of aspiration due to gastric compression. Anesthetic requirements are reduced due to increased sensitivity and blood flow changes. Proper positioning is important to avoid supine hypotension from vena cava compression.physiology pregnancy copy.pptx



physiology pregnancy copy.pptxsushmagupta67
Ěý
Pregnancy causes significant physiological changes to adapt to the developing fetus and its demands. These include increased blood volume, cardiac output and decreased systemic vascular resistance. Respiratory changes include increased oxygen consumption and minute ventilation. Gastrointestinal changes like delayed gastric emptying increase aspiration risk. Neurological changes enhance sensitivity to local anesthetics. Renal blood flow increases while liver function tests may be elevated. Understanding these changes is important for safe anesthesia care during pregnancy and delivery.Physiological changes during pregnancy



Physiological changes during pregnancyNaila Memon
Ěý
Physiological changes during pregnancy can be extensive. The uterus grows dramatically in size and the cervix softens. The breasts enlarge and darken. Throughout pregnancy, the body retains more fluid and blood volume increases. Respiration increases to support higher oxygen needs. The heart works harder pumping more blood. The kidneys and liver increase in size. Many hormonal changes prepare the body for childbirth and nurturing a baby.1 Physiology of Pregnan women Unit1-1.pptx



1 Physiology of Pregnan women Unit1-1.pptxeyaluayssa10q
Ěý
Pregnanant womans ethiopia as well as in the world accounts half of the total population Cvs respi renal physiology in pregnancy



Cvs respi renal physiology in pregnancyDrAnuradhaMSawant
Ěý
This document discusses the physiological changes that occur in the cardiovascular, respiratory, and urinary systems during pregnancy. Some key points:
- Cardiac output increases 30-50% by term due to rises in heart rate, stroke volume, and plasma volume. This supports the metabolic demands of the enlarged uterus and growing fetus.
- Respiratory alkalosis occurs due to progesterone-induced hyperventilation and a drop in carbon dioxide levels. This helps facilitate oxygen transfer from the mother to the fetus.
- Glomerular filtration rate increases up to 50% by the second trimester to support the higher circulating blood volume. This causes increases in urinary frequency.
- The diaphragm is elevatedCVS AND RESPIRATORY PHYSIOLOGY IN PREGNANCY



CVS AND RESPIRATORY PHYSIOLOGY IN PREGNANCYAnuradha Sawant
Ěý
Pregnancy causes significant physiological changes to the cardiovascular, respiratory, and urinary systems. The cardiovascular system undergoes remodeling to support the increased blood volume and cardiac output required to meet metabolic demands. The respiratory system experiences alkalosis due to progesterone-induced hyperventilation. Kidney function is elevated as glomerular filtration rate increases up to 50% by the second trimester to accommodate increased plasma volume.Physiological changes during pregnancy



Physiological changes during pregnancygelaye mandefro
Ěý
Physiological changes during pregnancy include:
1. Enlargement of the uterus, cervix, breasts, and other reproductive organs.
2. Increased blood volume, heart rate, and respiration to support the growing fetus and maternal organs.
3. Hormonal changes like increased progesterone and estrogen from the placenta lead to changes in metabolism, immune function, and other systems throughout the body.Physiological changes in pregnancy.pptx



Physiological changes in pregnancy.pptxfarhafatima11
Ěý
1) Physiological changes in pregnancy include increased weight, blood volume, cardiac output and decreased FRC.
2) Respiratory changes include increased oxygen consumption and minute ventilation but decreased FRC leading to risk of atelectasis.
3) Renal changes involve increased GFR and decreased resorption causing mild glycosuria and proteinuria.
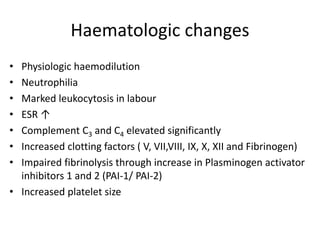
4) Hematological changes result in a hypercoagulable state with increased clotting factors and decreased platelets.Physiology of pregnancy. cardiovascular, respiratory and hematology



Physiology of pregnancy. cardiovascular, respiratory and hematologykr
Ěý
The document discusses the physiological changes that occur during pregnancy across multiple body systems. Key changes include an increase in cardiac output and blood volume to support the developing fetus. This leads to displacement of the heart and enlargement of the cardiac silhouette on chest x-rays. Shortness of breath is normal due to respiratory changes. Increased iron needs occur due to a rise in red blood cell and plasma volume. The document also provides guidance on diagnosing and managing anemia during pregnancy.Maternal physiology



Maternal physiologyArthi Rajasankar
Ěý
The document summarizes normal physiological changes during pregnancy across multiple body systems. Key changes include increased blood volume, cardiac output, and kidney function by the third trimester. Respiratory changes include decreased functional residual capacity and increased oxygen consumption. Regional anesthesia is affected by decreased drug requirements and difficult positioning due to changes in the back and abdomen. Overall, the document outlines the extensive anatomical and physiological adaptations required to support fetal growth and development during pregnancy.LESSON-1-High-Risk-Pregnancy.ppt



LESSON-1-High-Risk-Pregnancy.pptMaJeaneeneRimando
Ěý
This document discusses factors that can place a pregnancy at high risk and identifies various medical conditions that contribute to high risk pregnancies. It is divided into four main categories that can increase risk: existing health conditions, age, lifestyle factors, and conditions of pregnancy. Several existing health conditions are explained in more detail, including cardiovascular, hematologic, renal/urinary, respiratory, and rheumatic disorders. Complications associated with each condition for both the woman and fetus are provided.Maternal Physiology Lecture



Maternal Physiology LectureChukwuma Onyeije, MD, FACOG
Ěý
This document summarizes the normal physiological changes that occur in various maternal body systems during pregnancy. It describes how the cardiovascular, respiratory, renal, hematologic, gastrointestinal and reproductive systems adapt to accommodate the growing fetus. Key changes include increased blood volume, heart rate and kidney function as well as common symptoms like nausea and backache. Understanding these changes is important for identifying complications and educating patients about normal pregnancy.physiologicalchangesduringpregnancy-120719105010-phpapp02.pdf



physiologicalchangesduringpregnancy-120719105010-phpapp02.pdfSubi Babu
Ěý
Physiological changes during pregnancy can be extensive. The document summarizes several key changes:
1) The uterus grows enormously in size and weight to accommodate the growing fetus. Other genital organs like the cervix and breasts also see significant changes to support pregnancy and birth.
2) Extensive changes occur in many body systems like the cardiovascular, respiratory, urinary and endocrine systems to support the nutritional and oxygen needs of the mother and fetus. This includes increases in blood volume, cardiac output, kidney size and lung capacity.
3) Hormonal changes are also profound, with high levels of progesterone, estrogen and other placental hormones influencing many processes and organs across the body to sustain the pregnancy.Physiological Changes In Pregnancy



Physiological Changes In PregnancyShailendra Veerarajapura
Ěý
Physiological changes in pregnancy affect many body systems. The cardiovascular system adapts to support the growing fetus through increased blood volume, cardiac output, and stroke volume. The respiratory system increases minute ventilation and oxygen consumption while functional residual capacity decreases. The placenta allows passage of most anesthetic drugs from mother to fetus through passive diffusion. Anesthesiologists must consider these physiological alterations when planning anesthetic care for pregnant patients.Dialysis in pregnancy 



Dialysis in pregnancy hayam mansour
Ěý
This document discusses the management of pregnant women on hemodialysis. It notes that physiological changes during pregnancy can impact kidney function, but intensive hemodialysis of more than 20 hours per week is recommended to reduce risks. Close monitoring of blood pressure, nutrition, mineral levels, anemia and fetal growth is important. Hemodialysis prescription should be tailored to each patient's needs, with adjustments to dialysate composition and blood flow. Vaginal delivery at 38 weeks is typically recommended unless complications arise. A multidisciplinary team of nephrologists, obstetricians and dietitians helps optimize outcomes for these high-risk pregnancies.MATERNAL-PHY-edited.pptx



MATERNAL-PHY-edited.pptxastakghising
Ěý
The document provides an overview of the physiological changes that occur throughout the maternal body during pregnancy. Key changes discussed include:
- Uterine growth and changes to support fetal development.
- Increased cardiac output, blood volume, and vascular changes to support nutrient/waste exchange between mother and fetus.
- Respiratory changes like increased tidal volume to support oxygen demands.
- Renal changes like increased GFR and kidney size to excrete wastes and support calcium/electrolyte balance.
- Metabolic changes to support fetal growth including increased lipids, proteins, and iron.
- Skin changes like line striae and pigmentation due to hormonal influences.
- Central nervousPhysiological changes in pregnancy



Physiological changes in pregnancyKirty Nanda
Ěý
The document summarizes various anatomical, physiological, and biochemical changes that occur during pregnancy across multiple body systems. Key anatomical changes include uterine enlargement, breast changes, skin changes like lineae nigra and striae gravidarum. Physiological changes impact the cardiovascular, respiratory, renal and endocrine systems to support the nutritional and oxygen needs of the growing fetus. Hematological changes include increased blood volume and mild anemia. Biochemical changes involve iron metabolism and increased production of hormones like estrogen, progesterone, human placental lactogen and relaxin.Hypertensive disorders in Pregnancy



Hypertensive disorders in PregnancyTasbeeh ur Rahman
Ěý
A comprehensive overview of hypertensive disorders in pregnancy with its complications and management. Mainly focused on gestational hypertension, preeclampsia and eclampsia.Utero placental circulation and maternal to fetal transfer of drugs.pptx



Utero placental circulation and maternal to fetal transfer of drugs.pptxSaujanya Jung Pandey
Ěý
Utero placental circulation and maternal to fetal transfer of drugsUtero placental circulation and maternal to fetal transfer of drugs.pptx



Utero placental circulation and maternal to fetal transfer of drugs.pptxSaujanya Jung Pandey
Ěý
Utero placental circulation and maternal to fetal transfer of drugsMaternal physiology in pregnancy



Maternal physiology in pregnancyDr. Ram Lochan Yadav, M.D.
Ěý
This document discusses the extensive physiological and anatomical changes that occur during normal human pregnancy. It provides details on adaptations in multiple organ systems to support the growth and development of the fetus. The main changes include increased blood volume and cardiac output, anatomical changes to the uterus and cervix, hormonal changes involving hCG and estrogen, and metabolic adaptations to provide optimal nutrition for the fetus. All major body systems are impacted in ways that precisely meet the needs of pregnancy.HYPERTENSION DURING PREGNANCY SECOND SEMESTER



HYPERTENSION DURING PREGNANCY SECOND SEMESTERHannaDadacay
Ěý
This document discusses hypertension during pregnancy. It begins by defining high blood pressure and the different types of hypertension that can occur during pregnancy, including chronic hypertension, gestational hypertension, and preeclampsia. Mothers with hypertension during pregnancy are at higher risk for complications. The document then covers risk factors, symptoms, diagnostics, potential complications, treatment including medications like magnesium sulfate, and nursing considerations for managing hypertension during pregnancy.Cardiovascular changes in pregnancy



Cardiovascular changes in pregnancyNishant Thakur
Ěý
The cardiovascular system undergoes several changes during pregnancy to support the increased metabolic demands of the mother and fetus. The heart is pushed upward and outward by the enlarged uterus, increasing the cardiac silhouette. Cardiac output increases by 40-50% by 30-34 weeks due to higher blood volume, stroke volume, and heart rate. Blood pressure decreases slightly despite increased cardiac output due to lower systemic vascular resistance from progesterone and other hormones. Venous pressure, especially in the legs, increases significantly due to pressure from the gravid uterus. These cardiovascular changes help increase blood flow to the uterus and other organs to support the nutritional needs of the growing fetus.Renal physiology in pregnancy



Renal physiology in pregnancyNandinii Ramasenderan
Ěý
The document provides an overview of renal physiology and function, including:
- The components and basic functions of the nephron, including filtration, reabsorption, and secretion in different parts of the nephron.
- Hormonal regulation of kidney function including renin, aldosterone, antidiuretic hormone, and erythropoietin.
- Changes in kidney anatomy and function that occur during pregnancy, including increased blood flow, glomerular filtration rate, and effects of progesterone on vasodilation and sodium retention.
- Considerations for managing pregnancy in women with chronic kidney disease, including risks of deterioration and importance of multidisciplinary management and monitoring.Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxdribnibrahem164
Ěý
neurological complications of infective endocarditisIMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINE



IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINERelianceNwosu
Ěý
This presentation emphasizes the role of immunodiagnostics and Immunotherapy. More Related Content
Similar to Physiological changes in pregnancy.ppt (20)
Cvs respi renal physiology in pregnancy



Cvs respi renal physiology in pregnancyDrAnuradhaMSawant
Ěý
This document discusses the physiological changes that occur in the cardiovascular, respiratory, and urinary systems during pregnancy. Some key points:
- Cardiac output increases 30-50% by term due to rises in heart rate, stroke volume, and plasma volume. This supports the metabolic demands of the enlarged uterus and growing fetus.
- Respiratory alkalosis occurs due to progesterone-induced hyperventilation and a drop in carbon dioxide levels. This helps facilitate oxygen transfer from the mother to the fetus.
- Glomerular filtration rate increases up to 50% by the second trimester to support the higher circulating blood volume. This causes increases in urinary frequency.
- The diaphragm is elevatedCVS AND RESPIRATORY PHYSIOLOGY IN PREGNANCY



CVS AND RESPIRATORY PHYSIOLOGY IN PREGNANCYAnuradha Sawant
Ěý
Pregnancy causes significant physiological changes to the cardiovascular, respiratory, and urinary systems. The cardiovascular system undergoes remodeling to support the increased blood volume and cardiac output required to meet metabolic demands. The respiratory system experiences alkalosis due to progesterone-induced hyperventilation. Kidney function is elevated as glomerular filtration rate increases up to 50% by the second trimester to accommodate increased plasma volume.Physiological changes during pregnancy



Physiological changes during pregnancygelaye mandefro
Ěý
Physiological changes during pregnancy include:
1. Enlargement of the uterus, cervix, breasts, and other reproductive organs.
2. Increased blood volume, heart rate, and respiration to support the growing fetus and maternal organs.
3. Hormonal changes like increased progesterone and estrogen from the placenta lead to changes in metabolism, immune function, and other systems throughout the body.Physiological changes in pregnancy.pptx



Physiological changes in pregnancy.pptxfarhafatima11
Ěý
1) Physiological changes in pregnancy include increased weight, blood volume, cardiac output and decreased FRC.
2) Respiratory changes include increased oxygen consumption and minute ventilation but decreased FRC leading to risk of atelectasis.
3) Renal changes involve increased GFR and decreased resorption causing mild glycosuria and proteinuria.
4) Hematological changes result in a hypercoagulable state with increased clotting factors and decreased platelets.Physiology of pregnancy. cardiovascular, respiratory and hematology



Physiology of pregnancy. cardiovascular, respiratory and hematologykr
Ěý
The document discusses the physiological changes that occur during pregnancy across multiple body systems. Key changes include an increase in cardiac output and blood volume to support the developing fetus. This leads to displacement of the heart and enlargement of the cardiac silhouette on chest x-rays. Shortness of breath is normal due to respiratory changes. Increased iron needs occur due to a rise in red blood cell and plasma volume. The document also provides guidance on diagnosing and managing anemia during pregnancy.Maternal physiology



Maternal physiologyArthi Rajasankar
Ěý
The document summarizes normal physiological changes during pregnancy across multiple body systems. Key changes include increased blood volume, cardiac output, and kidney function by the third trimester. Respiratory changes include decreased functional residual capacity and increased oxygen consumption. Regional anesthesia is affected by decreased drug requirements and difficult positioning due to changes in the back and abdomen. Overall, the document outlines the extensive anatomical and physiological adaptations required to support fetal growth and development during pregnancy.LESSON-1-High-Risk-Pregnancy.ppt



LESSON-1-High-Risk-Pregnancy.pptMaJeaneeneRimando
Ěý
This document discusses factors that can place a pregnancy at high risk and identifies various medical conditions that contribute to high risk pregnancies. It is divided into four main categories that can increase risk: existing health conditions, age, lifestyle factors, and conditions of pregnancy. Several existing health conditions are explained in more detail, including cardiovascular, hematologic, renal/urinary, respiratory, and rheumatic disorders. Complications associated with each condition for both the woman and fetus are provided.Maternal Physiology Lecture



Maternal Physiology LectureChukwuma Onyeije, MD, FACOG
Ěý
This document summarizes the normal physiological changes that occur in various maternal body systems during pregnancy. It describes how the cardiovascular, respiratory, renal, hematologic, gastrointestinal and reproductive systems adapt to accommodate the growing fetus. Key changes include increased blood volume, heart rate and kidney function as well as common symptoms like nausea and backache. Understanding these changes is important for identifying complications and educating patients about normal pregnancy.physiologicalchangesduringpregnancy-120719105010-phpapp02.pdf



physiologicalchangesduringpregnancy-120719105010-phpapp02.pdfSubi Babu
Ěý
Physiological changes during pregnancy can be extensive. The document summarizes several key changes:
1) The uterus grows enormously in size and weight to accommodate the growing fetus. Other genital organs like the cervix and breasts also see significant changes to support pregnancy and birth.
2) Extensive changes occur in many body systems like the cardiovascular, respiratory, urinary and endocrine systems to support the nutritional and oxygen needs of the mother and fetus. This includes increases in blood volume, cardiac output, kidney size and lung capacity.
3) Hormonal changes are also profound, with high levels of progesterone, estrogen and other placental hormones influencing many processes and organs across the body to sustain the pregnancy.Physiological Changes In Pregnancy



Physiological Changes In PregnancyShailendra Veerarajapura
Ěý
Physiological changes in pregnancy affect many body systems. The cardiovascular system adapts to support the growing fetus through increased blood volume, cardiac output, and stroke volume. The respiratory system increases minute ventilation and oxygen consumption while functional residual capacity decreases. The placenta allows passage of most anesthetic drugs from mother to fetus through passive diffusion. Anesthesiologists must consider these physiological alterations when planning anesthetic care for pregnant patients.Dialysis in pregnancy 



Dialysis in pregnancy hayam mansour
Ěý
This document discusses the management of pregnant women on hemodialysis. It notes that physiological changes during pregnancy can impact kidney function, but intensive hemodialysis of more than 20 hours per week is recommended to reduce risks. Close monitoring of blood pressure, nutrition, mineral levels, anemia and fetal growth is important. Hemodialysis prescription should be tailored to each patient's needs, with adjustments to dialysate composition and blood flow. Vaginal delivery at 38 weeks is typically recommended unless complications arise. A multidisciplinary team of nephrologists, obstetricians and dietitians helps optimize outcomes for these high-risk pregnancies.MATERNAL-PHY-edited.pptx



MATERNAL-PHY-edited.pptxastakghising
Ěý
The document provides an overview of the physiological changes that occur throughout the maternal body during pregnancy. Key changes discussed include:
- Uterine growth and changes to support fetal development.
- Increased cardiac output, blood volume, and vascular changes to support nutrient/waste exchange between mother and fetus.
- Respiratory changes like increased tidal volume to support oxygen demands.
- Renal changes like increased GFR and kidney size to excrete wastes and support calcium/electrolyte balance.
- Metabolic changes to support fetal growth including increased lipids, proteins, and iron.
- Skin changes like line striae and pigmentation due to hormonal influences.
- Central nervousPhysiological changes in pregnancy



Physiological changes in pregnancyKirty Nanda
Ěý
The document summarizes various anatomical, physiological, and biochemical changes that occur during pregnancy across multiple body systems. Key anatomical changes include uterine enlargement, breast changes, skin changes like lineae nigra and striae gravidarum. Physiological changes impact the cardiovascular, respiratory, renal and endocrine systems to support the nutritional and oxygen needs of the growing fetus. Hematological changes include increased blood volume and mild anemia. Biochemical changes involve iron metabolism and increased production of hormones like estrogen, progesterone, human placental lactogen and relaxin.Hypertensive disorders in Pregnancy



Hypertensive disorders in PregnancyTasbeeh ur Rahman
Ěý
A comprehensive overview of hypertensive disorders in pregnancy with its complications and management. Mainly focused on gestational hypertension, preeclampsia and eclampsia.Utero placental circulation and maternal to fetal transfer of drugs.pptx



Utero placental circulation and maternal to fetal transfer of drugs.pptxSaujanya Jung Pandey
Ěý
Utero placental circulation and maternal to fetal transfer of drugsUtero placental circulation and maternal to fetal transfer of drugs.pptx



Utero placental circulation and maternal to fetal transfer of drugs.pptxSaujanya Jung Pandey
Ěý
Utero placental circulation and maternal to fetal transfer of drugsMaternal physiology in pregnancy



Maternal physiology in pregnancyDr. Ram Lochan Yadav, M.D.
Ěý
This document discusses the extensive physiological and anatomical changes that occur during normal human pregnancy. It provides details on adaptations in multiple organ systems to support the growth and development of the fetus. The main changes include increased blood volume and cardiac output, anatomical changes to the uterus and cervix, hormonal changes involving hCG and estrogen, and metabolic adaptations to provide optimal nutrition for the fetus. All major body systems are impacted in ways that precisely meet the needs of pregnancy.HYPERTENSION DURING PREGNANCY SECOND SEMESTER



HYPERTENSION DURING PREGNANCY SECOND SEMESTERHannaDadacay
Ěý
This document discusses hypertension during pregnancy. It begins by defining high blood pressure and the different types of hypertension that can occur during pregnancy, including chronic hypertension, gestational hypertension, and preeclampsia. Mothers with hypertension during pregnancy are at higher risk for complications. The document then covers risk factors, symptoms, diagnostics, potential complications, treatment including medications like magnesium sulfate, and nursing considerations for managing hypertension during pregnancy.Cardiovascular changes in pregnancy



Cardiovascular changes in pregnancyNishant Thakur
Ěý
The cardiovascular system undergoes several changes during pregnancy to support the increased metabolic demands of the mother and fetus. The heart is pushed upward and outward by the enlarged uterus, increasing the cardiac silhouette. Cardiac output increases by 40-50% by 30-34 weeks due to higher blood volume, stroke volume, and heart rate. Blood pressure decreases slightly despite increased cardiac output due to lower systemic vascular resistance from progesterone and other hormones. Venous pressure, especially in the legs, increases significantly due to pressure from the gravid uterus. These cardiovascular changes help increase blood flow to the uterus and other organs to support the nutritional needs of the growing fetus.Renal physiology in pregnancy



Renal physiology in pregnancyNandinii Ramasenderan
Ěý
The document provides an overview of renal physiology and function, including:
- The components and basic functions of the nephron, including filtration, reabsorption, and secretion in different parts of the nephron.
- Hormonal regulation of kidney function including renin, aldosterone, antidiuretic hormone, and erythropoietin.
- Changes in kidney anatomy and function that occur during pregnancy, including increased blood flow, glomerular filtration rate, and effects of progesterone on vasodilation and sodium retention.
- Considerations for managing pregnancy in women with chronic kidney disease, including risks of deterioration and importance of multidisciplinary management and monitoring.Recently uploaded (20)
Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxdribnibrahem164
Ěý
neurological complications of infective endocarditisIMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINE



IMMUNO-ONCOLOGY DESCOVERING THE IMPORTANCE OF CLINICAL IMUNOLOGY IN MEDICINERelianceNwosu
Ěý
This presentation emphasizes the role of immunodiagnostics and Immunotherapy. Syncope in dentistry.pptx



Syncope in dentistry.pptxDr Kingshika Joylin
Ěý
This presentation provides an overview of syncope, a common medical emergency in dental practice. Created during my internship, this presentation aims to educate dental students on the causes, symptoms, diagnosis and management of syncope with a focus on dental specific considerations.
Patient-Centred Care in Cytopenic Myelofibrosis: Collaborative Conversations ...



Patient-Centred Care in Cytopenic Myelofibrosis: Collaborative Conversations ...PeerVoice
Ěý
Claire Harrison, DM, FRCP, FRCPath, and Charlie Nicholson, discuss myelofibrosis in this CE activity titled "Patient-Centred Care in Cytopenic Myelofibrosis: Collaborative Conversations on Treatment Goals and Decisions." For the full presentation, please visit us at www.peervoice.com/JJY870.TunesKit Spotify Converter Crack With Registration Code 2025 Free



TunesKit Spotify Converter Crack With Registration Code 2025 Freedfsdsfs386
Ěý
TunesKit Spotify Converter is a software tool that allows users to convert and download Spotify music to various formats, such as MP3, AAC, FLAC, or WAV. It is particularly useful for Spotify users who want to keep their favorite tracks offline and have them in a more accessible format, especially if they wish to listen to them on devices that do not support the Spotify app.
https://shorturl.at/LDQ9c
Copy Above link & paste in New TabEnzyme Induction and Inhibition: Mechanisms, Examples & Clinical Significance



Enzyme Induction and Inhibition: Mechanisms, Examples & Clinical SignificanceSumeetSharma591398
Ěý
This presentation explains the crucial role of enzyme induction and inhibition in drug metabolism. It covers:
✔️ Mechanisms of enzyme regulation in the liver
✔️ Examples of enzyme inducers (Rifampin, Carbamazepine) and inhibitors (Ketoconazole, Grapefruit juice)
✔️ Clinical significance of drug interactions affecting efficacy and toxicity
✔️ Factors like genetics, age, diet, and disease influencing enzyme activity
Ideal for pharmacy, pharmacology, and medical students, this presentation helps in understanding drug metabolism and dosage adjustments for safe medication use.Pediatric Refeeding syndrome: comprehensive overview.pptx



Pediatric Refeeding syndrome: comprehensive overview.pptxGabriel Shamavu
Ěý
Refeeding Syndrome in Severely Malnourished Child, compréhensive summary by Dr SHAMAVU Gabriel The influence of birth companion in mother care and neonatal outcome



The influence of birth companion in mother care and neonatal outcomelksharma10797
Ěý
this content related to birth companionship, role of birth companion in care of mother and neonatal Research Hyopthesis and Research Assumption



Research Hyopthesis and Research AssumptionDr. Binu Babu Nursing Lectures Incredibly Easy
Ěý
Research Hyopthesis and AssumptionE Book Daniya Sanal.pdf#healthy books.com



E Book Daniya Sanal.pdf#healthy books.comDaniyaSanal
Ěý
good health for good life good heart for safe and secure life..the good quality of life will makes good and #haelthy vibes...Union Budget 2025 Healthcare Sector Analysis & Impact (PPT).pdf



Union Budget 2025 Healthcare Sector Analysis & Impact (PPT).pdfAditiAlishetty
Ěý
The Union Budget 2025-26 emphasizes enhancing India's healthcare by allocating â‚ą99,858 crore to the Ministry of Health and Family Welfare, marking a 10% increase from the previous year. Key initiatives include adding 10,000 medical college seats, with a plan to reach 75,000 over five years, and increasing funding for the Pradhan Mantri Ayushman Bharat Health Infrastructure Mission by 41% to â‚ą4,758 crore. However, experts express concerns that the allocation may still fall short of the sector's urgent needs. Dr. Bipin Vibhute, a distinguished Liver and Multi-Organ Transplant Surgeon, is renowned for pioneering free liver transplants for pediatric patients up to 12 years old in Pune. As the Program Director of the Center for Organ Transplants at Sahyadri Hospitals, he has significantly advanced organ transplantation services across Maharashtra.delayed recovery of anaesthesia ppt. delayed



delayed recovery of anaesthesia ppt. delayedSimmons2
Ěý
delayed recovery from anaesthesia
#anaesthesia#delayed recoveryMacafem Reviews 2024 - Macafem for Menopause Symptoms



Macafem Reviews 2024 - Macafem for Menopause SymptomsMacafem Supplement
Ěý
At Macafem, we provide 100% natural support for women navigating menopause. For over 20 years, we've helped women manage symptoms, and in 2024, we're proud to share their heartfelt experiences.Understanding Trauma: Causes, Effects, and Healing Strategies



Understanding Trauma: Causes, Effects, and Healing StrategiesBecoming Institute
Ěý
Trauma affects millions of people worldwide, shaping their emotional, psychological, and even physical well-being. This presentation delves into the root causes of trauma, its profound effects on mental health, and practical strategies for healing. Whether you are seeking to understand your own experiences or support others on their journey, this guide offers insights into coping mechanisms, therapy approaches, and self-care techniques. Explore how trauma impacts the brain, body, and relationships, and discover pathways to resilience and recovery.
Perfect for mental health advocates, therapists, educators, and anyone looking to foster emotional well-being. Watch now and take the first step toward healing!Introduction-to-the-PuroKalusugan-InitiativeCHD12.pptx



Introduction-to-the-PuroKalusugan-InitiativeCHD12.pptxhepopolomolok2023
Ěý
An introduction to the PuroKalusugan InitiativeRole of Artificial Intelligence in Clinical Microbiology.pptx



Role of Artificial Intelligence in Clinical Microbiology.pptxDr Punith Kumar
Ěý
Artificial Intelligence (AI) is revolutionizing clinical microbiology by enhancing diagnostic accuracy, automating workflows, and improving patient outcomes. This presentation explores the key applications of AI in microbial identification, antimicrobial resistance detection, and laboratory automation. Learn how machine learning, deep learning, and data-driven analytics are transforming the field, leading to faster and more efficient microbiological diagnostics. Whether you're a researcher, clinician, or healthcare professional, this presentation provides valuable insights into the future of AI in microbiology.Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education
Ěý
Co-Chairs, Robert M. Hughes, DO, and Christina Y. Weng, MD, MBA, prepared useful Practice Aids pertaining to retinal vein occlusion for this CME activity titled “Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Specialty Care.” For the full presentation, downloadable Practice Aids, and complete CME information, and to apply for credit, please visit us at https://bit.ly/3NyN81S. CME credit will be available until March 3, 2026.Eye assessment in polytrauma for undergraduates.pptx



Eye assessment in polytrauma for undergraduates.pptxKafrELShiekh University
Ěý
Eye assessment in polytrauma for undergraduates.Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxMohamadAlhes
Ěý
Neurological complications of inflective endocarditis Enzyme Induction and Inhibition: Mechanisms, Examples, and Clinical Significance



Enzyme Induction and Inhibition: Mechanisms, Examples, and Clinical SignificanceSumeetSharma591398
Ěý
This presentation explains the concepts of enzyme induction and enzyme inhibition in drug metabolism. It covers the mechanisms, examples, clinical significance, and factors affecting enzyme activity, with a focus on CYP450 enzymes. Learn how these processes impact drug interactions, efficacy, and toxicity. Essential for pharmacy, pharmacology, and medical students.Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education
Ěý
Enzyme Induction and Inhibition: Mechanisms, Examples, and Clinical Significance



Enzyme Induction and Inhibition: Mechanisms, Examples, and Clinical SignificanceSumeetSharma591398
Ěý
Physiological changes in pregnancy.ppt
- 1. Physiological changes in pregnancy
- 2. Maternal adaptations to pregnancy ď‚žProfound anatomical, physiological and biochemical changes occur during pregnancy ď‚žPurpose is to support growth of the fetus and prepare the mother for delivery and lactation ď‚žSome of the adaptations may be considered abnormal if the patient was not pregnant ď‚žNormal adaptations can be misinterpreted as disease ď‚žPregnancy adaptations can unmask or worsen pre-existing disease
- 3. Uterine changes ď‚žProgressive uterine enlargement ď‚— Helps in gestational dating ď‚— Helps in assessing fetal growth ď‚— Occurs in ectopic pregnancy also ď‚— Contributes to pedal edema by occluding venous return ď‚žSupine hypotension ď‚— Due to vena caval compression ď‚— Occurs in women with poor collateral circulation
- 4. Haemodynamic changes Increased intra-vascular volume  Blood volume ○ Increased by 40 - 45% ( appx 1.5 litres)  Plasma volume ○ Increased by 50% ( appx 1.2 litres)  RBC volume ○ Increased by 20 – 30 % ( appx 250 – 400 ml) Increased cardiac output  Increased by 40 – 50% ( appx 1.8 litres / min)
- 5. Haemodynamic changes • Decreased peripheral vascular resistance – Decreased by 20 – 25% • Decreased pulmonary vascular resistance – Decreased by 30 – 35% • Decreased colloid oncotic pressure – Decreased by 10 – 15% from 20.8 mm of Hg to 18 mm of Hg • Increased heart rate – Increased by 15 – 20% • Increased regional blood flow – Uterine 750 ml /min ; Renal 1200 ml / min ; Cutaneous 500ml / min
- 6. Clinical Implications • Increased cardiac workload • Misinterpretation as heart disease • Aggravation of pre-existing disease • Susceptibility to Pulmonary edema – Pre eclampsia – Heart disease
- 7. Symptoms & Signs which mimic Heart disease during pregnancy • Breathlessness • Pedal oedema • Easy fatigability • Palpitations • Orthopnoea • Soft systolic murmurs • Continuous parasternal murmurs • Third heart sound • Displacement of the heart
- 8. Effects of pregnancy on heart disease • Precipitation of cardiac failure – Aggravating factors • Maternal age • Arrhythmias • Anaemia • Pre eclampsia • Multifetal gestation • Activity • Infection • Anxiety • Increased coagulability of blood • Risk of infective endocarditis during labour / termination of pregnancy
- 9. Haematologic changes • Physiologic haemodilution • Neutrophilia • Marked leukocytosis in labour • ESR ↑ • Complement C3 and C4 elevated significantly • Increased clotting factors ( V, VII,VIII, IX, X, XII and Fibrinogen) • Impaired fibrinolysis through increase in Plasminogen activator inhibitors 1 and 2 (PAI-1/ PAI-2) • Increased platelet size
- 10. Clinical implications • Increased demands during pregnancy unmask iron and folic acid deficiency states, and haematologic disorders like haemoglobinopathies • Pregnancy and puerperium are thrombogenic states
- 11. Metabolic changes • Water retention approx 6.5 litres • Increased plasma lipids and lipoproteins – Serum cholestrol ↑ 40% – Serum triglycerides ↑ 50% • Altered plasma proteins – Albumin ↓ to ~ 3 gm% (Non pregnant ~ 4.3 gm%) – Globulin ↑ to ~ 3 gm% (Non pregnant ~ 2.6 gm%) – A:G ratio 1 : 1 (Non pregnant 1.7 : 1) • Altered pH – 7.45 (Non pregnant 7.4) • Altered plasma bicarbonate – 22 m mol /L (Non pregnant 26 m mol /L)
- 12. Respiratory system • Increased awareness of a desire to breathe (Progesterone induced central effect) • Diaphragm rises by ~ 4 cm. Transverse diameter of thoracic cage ↑ by ~ 2 cm • Functional residual capacity ↓ to ~ 1500 ml (Non pregnant ~ 2000 ml) • Respiratory rate unchanged • ↑ tidal volume ~ 700 ml (Non pregnant ~ 500ml) • 40 % ↑ minute ventilation ~ 10.5 L (Non pregnant 7.5 L) • Respiratory alkalosis pCO ~ 28 mm Hg (Non
- 13. Clinical implications • Increased awareness of desire to breathe may be mistaken for dyspnoea • Respiratory adaptations help in meeting oxygen requirements of the fetus • Respiratory alkalosis present in pregnancy • ↑ 2,3 – DPG levels in maternal erythrocytes shifts Oxygen Dissociation Curve to the right, counter- acting the effect of respiratory alkalosis and facilitating oxygen transfer to the fetus • ABG values need to be interpreted in the context of pregnancy
- 14. Urinary system • Dilatation of renal pelvis, calyces and ureters because of hormonal and mechanical influences • GFR ↑ 50% (Non pregnant 120 ml / min) • Renal plasma flow ↑ 45 – 50% • ↓ Serum creatinine & Blood urea levels • Serum osmolality ↓ by ~ 10 m Osm / Kg (Non pregnant 280 – 300 m Osm / Kg)
- 15. Clinical implications • Hydronephrosis and hydroureter during pregnancy should not be mistaken for obstructive uropathy – These changes are more marked on the right side – These changes may take upto 12 weeks to resolve post- partum) • Upper UTIs are more virulent • Nocturia more likely as dependant edema fluid is mobilized and excreted by the kidney • ↑ frequency due to mechanical bladder compression • S. creatinine > 0.8 mg% and Blood urea > 30 mg%
- 16. Gastro – intestinal system • Displacement of organs – Appendix displaced upwards and laterally • ↓ gastric empyting • ↓ tone of gastro-esophageal sphincter • Delayed intestinal transit time • Altered liver function tests – ↑ alkaline phosphatase (Non pregnant 21 – 91 IU/L or 4 – 13 KA units) – ↓ plasma albumin – ↑ plasma globulin • Hyperemia and softening of gums
- 17. Clinical implications • Atypical symptoms and signs of appendicitis during pregnancy. Risk of peritonitis ↑ • Major risk of regurgitation and acid aspiration during GA • ↑ incidence of reflux oesophagitis, constipation and haemmorhoids during pregnancy • Bleeding from gums during pregnancy while brushing
- 18. Endocrine system • ↑ serum Prolactin ~ 150 ng / ml (Non pregnant < 20 ng / ml) • ↑ TBG • ↑ Total T3 (Non pregnant 80 -100 ng / dl) and T4 (Non pregnant 4 -12 μgm /dl) • TSH levels unchanged except for slight decrease in I trimester ( normal range < 5 μIU/ml or < 5 mIU / L) • ↑ BMR by 25 % can be attributed to fetal
- 19. Thank you



