POST ERCP PANCREATITIS- RISK FACTORS / PREVENTION / TREATMENT
- 1. POST ERCP PANCREATITI S FROM BENCH TO BEDSISE By Dr. Darayus P. Gazder Senior Registrar Ziauddin Hospital
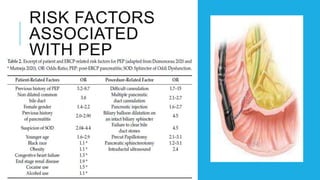
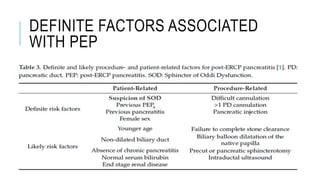
- 2. POST-ERCP PANCREATI TIS (PEP) OVERVIEW Common complication of ERCP Can range from mild to severe Severe cases may involve multi-organ failure and death Post-ERCP Pancreatitis (PEP) is a serious complication of ERCP. It can be mitigated through pharmacological and procedural measures, prompt diagnosis, and early management. Recent research and international guidelines offer evidence-based strategies to reduce PEP risk. Implementing these practices, along with quality assurance and training, will improve patient safety.
- 4. PATHOPHYSIOL OGY OF PEP ŌĆóInterplay of mechanical obstruction and hydrostatic injury ŌĆóEarly activation of pancreatic enzymes causing inflammation ŌĆóObstruction due to: ŌĆó Edema or trauma to the papilla ŌĆó Over-manipulation ŌĆóHydrostatic injury from: ŌĆó Pancreatic duct (PD) injection with contrast agents or water ŌĆó Acinarization ŌĆóOther causes: ŌĆó Perforation of PD side branch with guidewire ŌĆó Use of electrocautery ŌĆó Possible allergic reaction to contrast agent
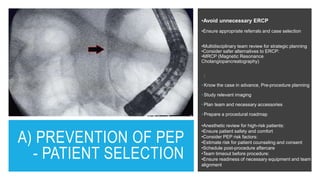
- 8. A) PREVENTION OF PEP - PATIENT SELECTION ŌĆóAvoid unnecessary ERCP ŌĆóEnsure appropriate referrals and case selection ŌĆóMultidisciplinary team review for strategic planning ŌĆóConsider safer alternatives to ERCP: ŌĆóMRCP (Magnetic Resonance Cholangiopancreatography) : ŌĆó Know the case in advance, Pre-procedure planning ŌĆó Study relevant imaging ŌĆó Plan team and necessary accessories ŌĆó Prepare a procedural roadmap ŌĆóAnesthetic review for high-risk patients: ŌĆóEnsure patient safety and comfort ŌĆóConsider PEP risk factors: ŌĆóEstimate risk for patient counseling and consent ŌĆóSchedule post-procedure aftercare ŌĆóTeam timeout before procedure: ŌĆóEnsure readiness of necessary equipment and team alignment
- 9. B) MEDICAL PROPHYLAXIS OF PEP NSAIDs: ŌĆó Effective for PEP prophylaxis (NNT: 8-21) ŌĆó Rectal diclofenac most effective ŌĆó Pre-ERCP NSAIDs more effective than post-ERCP ŌĆó Not recommended in late pregnancy or with NSAID allergies Intravenous Fluids: ŌĆó Recommended when NSAIDs are contraindicated ŌĆó Effective but caution in fluid overload conditions ŌĆó ESGE hydration protocol: 3 mL/kg/h during ERCP, 20 mL/kg bolus post-ERCP, 3 mL/kg/h for 8 hours after Glyceryl Trinitrate (GTN): ŌĆó Reduces sphincter of Oddi contractility ŌĆó Effective in reducing overall PEP incidence ŌĆó Recommended for NSAID-allergic patients or without pancreatic stenting ŌĆó Use with caution due to potential hypotension and headache Other Agents: ŌĆó Somatostatin: Some evidence of risk reduction, not currently recommended by ESGE ŌĆó Protease inhibitors and topical epinephrine not recommended due to uncertain efficacy
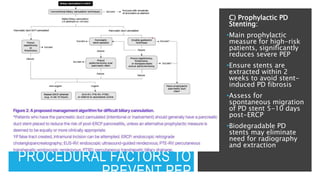
- 10. C) PROCEDURAL FACTORS TO PREVENT PEP A) Difficult Biliary Cannulation: Use wire-guided biliary cannulation for higher success and less PD contrast injection Stable scope position, study papilla morphology, plan cannulation trajectory Define difficult cannulation using ŌĆ£5-5-1ŌĆØ (> 5 minutes - 5 cannulation attempts - 1 unintended pancreas duct cannulation) were proposed by the European Society of Gastrointestinal Endoscopy OR ŌĆ£15-10-2ŌĆØ rule (i.e., 15 min of cannulation attempts, 10 contacts with the papilla and Ōēź2 accidental PD cannulations Early precut-papillotomy or needle-knife fistulotomy reduces PEP (requires expertise) Consider repeating ERCP after 2-4 days if initial attempt fails B) Inadvertent PD Cannulation: ŌĆóUse early pancreatic guidewire-assisted techniques like DGW (Double-guidewire technique) or TPS (transpancreatic biliary septotomy) ŌĆóDGW: Higher successful biliary cannulation rates with no impact on PEP rates ŌĆóTPS: Higher successful biliary cannulation rates with comparable PEP rates to DGW ŌĆóSecure guidewire in PD, consider prophylactic PD stenting post-procedure
- 11. PROCEDURAL FACTORS TO PREVENT PEP C) Prophylactic PD Stenting: ŌĆóMain prophylactic measure for high-risk patients, significantly reduces severe PEP ŌĆóEnsure stents are extracted within 2 weeks to avoid stent- induced PD fibrosis ŌĆóAssess for spontaneous migration of PD stent 5-10 days post-ERCP ŌĆóBiodegradable PD stents may eliminate need for radiography and extraction
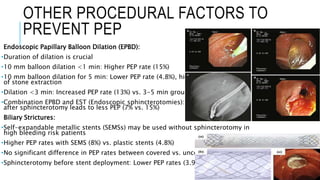
- 12. OTHER PROCEDURAL FACTORS TO PREVENT PEP Endoscopic Papillary Balloon Dilation (EPBD): ŌĆóDuration of dilation is crucial ŌĆó10 mm balloon dilation <1 min: Higher PEP rate (15%) ŌĆó10 mm balloon dilation for 5 min: Lower PEP rate (4.8%), higher success of stone extraction ŌĆóDilation <3 min: Increased PEP rate (13%) vs. 3-5 min group (3%) ŌĆóCombination EPBD and EST (Endoscopic sphincterotomies): 30 s dilation after sphincterotomy leads to less PEP (7% vs. 15%) Biliary Strictures: ŌĆóSelf-expandable metallic stents (SEMSs) may be used without sphincterotomy in high bleeding risk patients ŌĆóHigher PEP rates with SEMS (8%) vs. plastic stents (4.8%) ŌĆóNo significant difference in PEP rates between covered vs. uncovered SEMS ŌĆóSphincterotomy before stent deployment: Lower PEP rates (3.9% vs. 20.6%)
- 13. SUMMARY OF INTERNATIONAL GUIDELINES ON PEP PROPHYLAXIS.
- 14. THANK YOU REFERENCES: 1) Buxbaum JL, Freeman M. American Society for Gastrointestinal Endoscopy guideline on post-ERCP pancreatitis prevention strategies: summary and recommendations. Gastrointestinal endoscopy. 2023 Feb 1;97(2):153-62. 2) Cahyadi O, Tehami N, de-Madaria E, Siau K. Post-ERCP Pancreatitis: Prevention, Diagnosis and Management. Medicina (Kaunas). 2022;58(9):1261. Published 2022 Sep 12. doi:10.3390/medicina58091261