Post Caesarian Pregnancy
- 2. Introduction ’éŚ Liberalization of primary CS ’éŚ Non recurrent indications ’éŚ Once a caesarean, always a caesarean ’éŚ Quite prevalent
- 3. Effects On Pregnancy And Labor ’éŚ Increases risk of ’üČAbortion ’üČPreterm labor ’üČPregnancy ailments ’üČOperative interference ’üČPlacenta praevia ’üČAdherent placenta ’üČPost partum hemorrhage ’üČPeripartum hysterectomy
- 4. Effects On The Scar ’éŚ Increased risk of scar rupture ’éŚ More risk in classical/ hysterotomy scar than lower segment scar ’éŚ Lower segment scar rupture during labor ’éŚ Classical/ hysterotomy scar ruptures during late pregnancy and labor ’éŚ Impairment of healing can cause early scar rupture
- 5. Lower SEGMENT VS CLASSICAL/ HYSTEROTOMY SCAR Lower Segment Classical /Hysterotomy Apposition Perfect, no pockets of blood Difficult to appose State of uterus during healing The part of uterus remains inert The part contracts and retracts Stretching effect Along the line of scar At right angles to scar Placental implantation Attachment on scar unlikely Placenta more likely to implant on scar Net effect Sound scar Weak scar Chances of rupture 0.2 - 1.5% 4 - 9% Mortality following Maternal and more rupture perinatal death less
- 7. INTEGRITY OF THE SCAR CLASSICAL SCAR : ’éŚ The scar is weak. ’éŚ The scar is more likely to give way during pregnancy with increased risk to the mother and fetus. ’éŚ These cases should be delivered by LSCS LOWER SEGEMENT TRANSVERSE SCAR: Usually heals better. During the course of labour the integrity of the scar need to be assessed. ’éŚ High index of suspicion is essential. ’éŚ Factor that are to be considered while assessing scar are: evidences of Scar Dehiscence during labor.
- 8. PREVIOUS SCAR ’é¦ Dehiscence-separation along the line of the previous scar ’éŚ Rupture ŌĆō when the unscarred tissue is also involved in separation
- 9. Management 1. Elective caesarean section 2. VBAC trial of labor (trial of scar)
- 10. Previous operative notes ’éŚ Indication of caesarean section: ’éŚ (a) Placenta praevia ŌĆō (i) imperfect apposition due to quick surgery and (ii) thrombosis of the placental sinuses. ’éŚ (b) Following prolonged labor-increased chance of sepsis. ’éŚ Technical difficulty in the primary operation leading to tears to involve the branches of uterine vessels.
- 11. Hysterography in interconceptional period: Hysterography, 6 months after the operation, may reveal defect on the scar Pregnancy: (1) Pregnancy occurring soon after operation (2)Pregnancy complication (3)h/o previous vaginal delivery following LSCS (4)Placenta praevia in present pregnancy
- 12. Hospitalization ’éŚ LSCS scar ’āĀ Hospitalization at 38 weeks ’éŚ Classical CS at 34 weeks ’āĀ due to possibility of rupture of scar in pregnancy
- 13. VBAC TRIAL OF LABOUR ’éŚ Proper case selection :- 2/3 of previous CS ’āĀ TOL; 2/3 of TOL ’āĀ VBAC ’éŚ Successful trial results in vaginal delivery of a live fetus without scar rupture ’éŚ A failed trial is said to occur when a emergency caesarean section is required or there is scar rupture
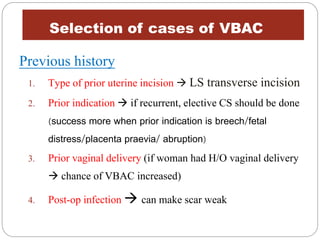
- 14. Selection of cases of VBAC Previous history 1. Type of prior uterine incision ’āĀ LS transverse incision 2. Prior indication ’āĀ if recurrent, elective CS should be done (success more when prior indication is breech/fetal distress/placenta praevia/ abruption) 3. Prior vaginal delivery (if woman had H/O vaginal delivery ’āĀ chance of VBAC increased) 4. Post-op infection ’āĀ can make scar weak
- 15. How many years back was the CS done ?? Min 18 months to heal the scar, so a gap of 18-24 months is necessary
- 16. Present pregnancy 1) No medical / obstetric complication 2) Average sized baby 3) Vertex presentation 4) No CPD
- 17. USG ’ā╝ To assess integrity of scar ’āĀ if myometrial thickness > 3.5mm, decreased risk of rupture ’ā╝ Helps to assess placental location ’ā╝ If placenta implanted over the scar’āĀ high chance of adherent placenta ’āĀ on USG ’āĀ no subplacental sonolucent zone
- 18. Contraindications ’éŚ Previous classical incision ’éŚ Previous two LSCS ’éŚ Pelvis contracted or suspected CPD ’éŚ Previous inverted T/ extension of incision ’éŚ Malpresentations ’éŚ Suspicion of CPD ’éŚ Medical /obstetric complication ’éŚ Multiple pregnancy ’éŚ PatientŌĆÖs refusal to undergo trial
- 19. Elective caesarean section ’üĮ If VBAC is contraindicated / if patient refuses ’üĮ Timing ŌĆó if fetal maturity is sure ’āĀ 39wks ŌĆó if not ’āĀ spontaneous labor awaited ŌĆó previous classical CS ’āĀ 38 wks
- 20. Evidence of scar rupture during labor ’ü▒Abnormal CTG-: late deceleration, most consistent finding ’ü▒ Suprapubic pain ’ü▒ Shoulder tip pain or chest pain or sudden onset of shortness of breath ’ü▒ Acute onset of scar tenderness ’ü▒ Abnormal vaginal bleeding or haematuria ’ü▒ Cessation of uterine contractions which were previously adequate ’ü▒ Maternal shock ’ü▒ Loss of station of presenting part ’ü▒Meconium staining of amniotic fluid
- 21. PROGNOSIS Previous history of classical LSCS or hysterotomy makes the women vulnerable for uterine rupture. this can increase the maternal mortality to 5% and perinatal mortality to 7.5%
- 23. Labor 1) Institutional delivery 2) Continuous CTG monitoring in labor 3) Facilities for performing an emergency CS
- 24. INVESTIGATIONS AND ASSESSMENT ’é¦ Mandatory regular antenatal checkup ’é¦ History of pain or tenderness over scar or any h/o vaginal bleeding ULTRASOUND : 1) To assess integrity of the scar. (Myometrial thickness>3.5mm ’āĀ NORMAL/low risk of uterine rupture 2) To assess placental location (absence of sub placental zone ’āĀ adherent placenta) - Doppler and MRI may be done for confirmation
- 25. ADMISSION AT 38 WEEKS ADMISSION AT 36 WEEKS ELECTIVE HOSPITALIZATION LOWER SEGMENT TRANSVERSE SCAR ELECTIVE C.S. VAGINAL DELIVERY CLASSICAL/ HYSTERECTOM Y SCAR ELECTIVE C.S. AT 38 WEEKS ’āś CASE ASSESSMENT ’āś FORMULATION OF Mode OF DELIVERY
- 26. EMERGENCY HOSPITALIZATION ONSET OF LABOUR SCAR RUPTURE OBSTETRIC COMPLICATIONS
- 27. MANAGEMENT OF LABOUR & DELIVERY ’éŚ Iv-Ringer solution ’éŚ Blood sample ŌĆō Hb%, grouping, cross matching ’éŚ Spontaneous onset of labor desired ’éŚ Monitoring ’éŚ Epidural analgesia ’éŚ Augmentation by oxytocin ŌĆō selectively & judiciously ’éŚ Prophylactic forceps or ventouse ’éŚ Exploration of uterus.
- 28. Delivery ’āśCut short the second stage with outlet forceps/vaccum ’āśLook for excessive bleeding in third stage-sign of scar rupture ’āśIf bleeding is excessive- emergency laparotomy ’āśObserve for 4-6hrs in labour ward
- 29. BENEFITS COMPLICATIONS Decrease in- ’éŚ maternal morbidity ’éŚ hospital stay ’éŚ need for blood transfusion ’éŚ risk of abnormal placentation ’éŚ need for c-section in next pregnancy MATERNAL: ’éŚ Uterine rupture ’éŚ Risk of hysterectomy ’éŚ Infections ’éŚ Maternal morbidity FOETAL: ’éŚ Fetal distress ’éŚ Low APGAR ’éŚ Death
- 30. STERILISATION ŌĆó Increasing risk after each operation ŌĆó During third time CS ’āĀ strerilization should be considered unless there is sufficiently strong reason to withhold it