Pre hospital rapid sequence intubation
- 1. Pre-hospital Rapid Sequence Intubation Dr Peter Sherren Senior registrar Anaesthesia, Intensive Care and Pre-hospital care The Royal London Hospital and Greater Sydney Area HEMS
- 2. Objectives ŌĆó Why? ŌĆó Who? ŌĆó How? ŌĆó Evidence
- 3. Introduction ŌĆó Controversial/Territorial/Evocative topic! ŌĆó Early appropriate airway control central to good trauma care ŌĆó Why not bring a hospital level of care to the roadside?
- 4. Why? ŌĆó Like haemorrhage, airway compromise is a significant cause of preventable deaths ŌĆó Hypoxia common on scene in trauma. Stochetti et al. J Trauma 1997 ŌĆó Hypoxia and hypercarbia associated with increased morbidity and mortality in TBI. Sherren PB et al. Curr Opin Anesthesiol 2012 ŌĆó ETI is gold standard in hospital ŌĆó Patient and pathology have no respect for geography
- 5. How? - Intubation without drugs or sedation only ŌĆó Successful ETI of trauma pts without drugs ~ mortality 99.8%. Lockey D et al. BMJ 2001. ŌĆó Low success rates in patients with reflexes intact (5-30%) ŌĆó ETI with sedation ŌĆó Still a low success rate ŌĆó ŌåæSecondary brain injury ŌĆó ŌåæMortality
- 6. SOLUTION = RAPID SEQUENCE INTUBATION (RSI)?
- 7. Components of RSI ŌĆó Preoxygenation ŌĆó Premedication ŌĆó Rapid induction of Anaesthesia ŌĆó MILS ┬▒ Cricoid ŌĆó Rapid onset neuromuscular relaxation ŌĆó Ideally no BVM ventilation ŌĆó ETI and confirmation ŌĆó Maintenance of Anaesthesia and paralysis
- 8. Components of RSI ŌĆó Preoxygenation definitive airway control Drug assisted ŌĆó Premedication ŌĆó Rapid induction of Anaesthesia Minimising time from induction to ETI ŌĆó MILS ┬▒ Cricoid ŌĆó Rapid onset neuromuscular relaxation Decreased gastric insufflation ŌĆó Ideally no BVM ventilation ŌĆó ETI and confirmation Decreased risk of hypoxia and aspiration ŌĆó Maintenance of Anaesthesia and paralysis
- 9. Controversies ŌĆó Optional Premedictions ŌĆó Sedate to preoxygenate (midazolam vs ketamine) ŌĆó Opioid (Fentanyl 1-3mcg/kg) to obtund hypertensive response to laryngoscopy and ICP spikes ŌĆó Fluid/blood bolus in hypovolaemic ŌĆó Atropine in paeds ŌĆó Induction agent? (much lower doses in hypovolaemic) ŌĆó Midazolam (0.3mg/kg) ŌĆó Propofol (1.5-2.5mg/kg) ŌĆó Thiopentone (3-5mg/kg) Reconstitution, SVR issues ŌĆó Etomidate (0.3mg/kg) 11╬▓/17╬▒ hydroxylase inhibition ŌĆó Ketamine (1-2mg/kg) CLOSE TO IDEAL AGENT
- 10. Controversies ŌĆó Optional Premedictions ŌĆó Sedate to preoxygenate (midazolam vs ketamine) ŌĆó Opioid (Fentanyl 1-3mcg/kg) to obtund hypertensive response to laryngoscopy and ICP spikes ŌĆó Fluid/blood bolus in hypovolaemic ŌĆó Atropine in paeds ŌĆó Induction agent? (much lower doses in hypovolaemic) ŌĆó Midazolam (0.3mg/kg) ŌĆó Propofol (1.5-2.5mg/kg) ŌĆó Thiopentone (3-5mg/kg) Reconstitution, SVR issues ŌĆó Etomidate (0.3mg/kg) 11╬▓/17╬▒ hydroxylase inhibition ŌĆó Ketamine (1-2mg/kg) CLOSE TO IDEAL AGENT
- 11. Controversies ŌĆó Neuromuscular blockade ŌĆó Suxamethonium (1.5-2mg/kg) ŌĆō Rapid, familiarity and obvious fasciculation end point but dirty drug ŌĆó Rocuronium (1.2mg/kg) ŌĆō Rapid, improved side effect profile and prolonged safe apnoea time ŌĆó Cricoid pressure - poor evidence & Ōåæ Difficult intubation. Harris T et al. Resuscitation 2010
- 12. Bottom line ŌĆó Generally right drug, at the right time, at the right doseŌĆ”ŌĆ”ŌĆ” ŌĆó Pre-hospital=high risk ŌåÆ Simplified evidence based Standard Operating Procedures (SOP) ŌĆó Remove individual practice in high risk environment, improve CRM and reduce human error
- 13. Not controversial ŌĆó Pre-hospital environment is no excuse for low standards of care ŌĆó Rigorous training, simulation, assessment and currencies ŌĆó Trained operator and assistant ŌĆó AAGBI standard of monitoring (ECG, NiBP, SpO2, waveform ETCO2) ŌĆó Quality control/assurance as part of good clinical governance ŌĆó Preoxygenation ŌĆó Non-rebreath mask or BVM ┬▒ PEEP valve ŌĆó Nasal cannula oxygen 15L/min. PreO2 + DAO ŌĆó Consider OPA/NPAx2/SGA
- 14. Still not controversial ŌĆó MILS - remove C-collar ŌĆó Maximise 1st pass intubation success ŌĆó Control your environment ŌĆó 360 degree access ŌĆó Optimise position ŌĆó Use bougie for all cases ŌĆó Standardised equipment and techniques ŌĆó Formalised failed intubation and oxygenation drills
- 15. Who? ŌĆó Impending or actual failure of airway patency ŌĆó Failure of airway protection ŌĆó Oxygenation or ventilation failure ŌĆó Injured patients who are unmanageable or severely agitated after head injury ŌĆó Humanitarian indications ŌĆó Anticipated clinical course
- 17. So we think pre-hospital RSI has a place, but who should be doing it? Ōåō A TRAINED AND COMPETENT TEAM
- 18. Physician-paramedic team ŌĆó Good medical experience ŌĆó Anaesthetic experience ŌĆó Doctor ŌēĀ pre-hospital RSI competent! ŌĆó Additional pre-hospital training ŌĆó Cost ŌĆó Availability
- 19. Double Paramedic or paramedic/air crewman ŌĆó At home in the pre- hospital environment ŌĆó Experienced++ ŌĆó Infrastructure and governance needed ŌĆó Infrequent occurrence for those purely working out of hospital; skill maintenance issue
- 20. Do paramedics want to do it? ŌĆó 99 London HEMS paramedics were asked if they felt RSI should be part of experienced UK paramedicŌĆÖs practice (courtesy of Prof D Lockey) ŌĆó 65% said yes pre-term at London HEMS ŌĆó Only 32% said yes on completion of their term working for HEMS ŌĆó Isolated to London HEMS?
- 21. Success rates of pre-hospital RSI ŌĆó Physician/paramedic team ŌĆó 99.4% London HEMS (348/350) Mackay CA et al. Emerg Med J 2001 ŌĆó 98.8% London HEMS (397/402) Harris T et al. Resuscitation 2010 ŌĆó 99.5% GSA-HEMS (185/186) Bloomer R et al. Emerg Med J 2012 ŌĆó 99.1% SAMU France (685/691) Adnet F et al. Ann Emerg Med 1998 ŌĆó 100% Germany (342/342) Helm M et al. Br J Anaesth 2006 ŌĆó Paramedic ŌĆó 97% MICA Victoria (152/157) Bernard SA et al. Ann Surg 2010 ŌĆó 96% Auckland rescue helicopter (~280) Tony Smith ŌĆó 86.7% San Diego (281/209) Davis DP et al. J Trauma 2003
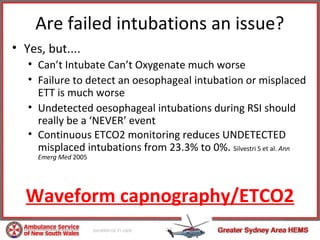
- 22. Are failed intubations an issue? ŌĆó Yes, but.... ŌĆó CanŌĆÖt Intubate CanŌĆÖt Oxygenate much worse ŌĆó Failure to detect an oesophageal intubation or misplaced ETT is much worse ŌĆó Undetected oesophageal intubations during RSI should really be a ŌĆśNEVERŌĆÖ event ŌĆó Continuous ETCO2 monitoring reduces UNDETECTED misplaced intubations from 23.3% to 0%. Silvestri S et al. Ann Emerg Med 2005 Waveform capnography/ETCO2
- 23. ŌĆó 209 RSI, 627 historical controls ŌĆó Mortality - RSI vs control, 33% vs 24% (p <0.05) ŌĆó Good outcome ŌĆō RSI vs control, 57% vs 45% (p <0.01) ŌĆó High rates of hypotension, hypoxaemia, hypercarbia ŌĆó Low intubation success ŌĆó Longer scene times ŌĆó Training issue? ŌĆó Use of ETCO2 not universal
- 24. ŌĆó312 pts RCT ŌĆóMICA paramedics with ETCO2 ŌĆóMidazolam/Sux ŌĆó97% success rate, 5 oesophageal intubations recognised ŌĆóFavourable outcome - 51% pre-hospital RSI compared 39% controls (p <0.05) ŌĆó13 lost to follow up, 1 more +ve outcome in control group would result in NS result
- 25. ŌĆó Prospective RCT by Careflight, awaiting publication ŌĆó Physician/paramedic vs standard care ŌĆó 338 recruited over 6yrs, needed 510 pts ŌĆó -ve primary outcome (GOSE 6 months) ŌĆó High cross over between groups ŌĆó When ASNSW physician/paramedic team added to careflight team data -> improved odds of survival at discharge (p-0.02)
- 26. Pre-hospital RSI is here to stay, so how do we make it safer?
- 28. PRE-HOSPITAL RSI Ōåō KEEP IT SIMPLE Ōåō STANDARDISE PRACTICE (equipment, techniques and drugs) Ōåō AVOID HUMAN ERROR Ōåō IMPROVE CRM
- 30. Standardised pre-hospital drugs ŌĆó Pre-drawn drugs ŌĆó Ketamine 200mg/20ml ŌĆó Suxamethonium 100mg/2ml (x2) ŌĆó Midazolam 10mg/10ml ŌĆó Morphine 10mg/10ml ŌĆó Spare Ampoules ŌĆó Rocuronium 50mg/5ml (x2) ŌĆó Fentanyl 500mcg/10ml (x2) ŌĆó Midazolam 15mg/3ml ŌĆó Ketamine 200mg/2ml (x5)
- 31. In hospital level of monitoring and Kit dump
- 33. Quality assurance and clinical governance
- 35. Summary ŌĆó Pre-hospital RSI is indicated in certain patients ŌĆó High risk intervention that needs to be delivered in a quality assured manner ŌĆó Pre-hospital RSI done badly is worse than standard management ŌĆó Some evidence for a morbidity and mortality benefit
- 36. Questions?