Prep family lecture_shepherd
- 1. Shepherd Center Acquired Brain Injury Program
- 2. Introduction ’éŚ What is Neuropsychology? ’éŚ What happened to your loved one? ’éŚ Part 1: ’éŚ Basics of the Brain ’éŚ What happens with a brain injury ’éŚ Part 2: ’éŚ 2 Tracks at Shepherd: all patient-specific ’éŚ PREP (Pre-rehabilitation Education Program) ’éŚ Rehab Program ’éŚ Discharge- What happens when you leave here?
- 3. Brain Anatomy ’éŚ Brain is soft, and has consistency of a Jello mold ’éŚ Fits relatively snuggly in the skull ’éŚ Attached to skull by small veins and meninges ’éŚ Floats in cerebral spinal fluid ’éŚ Provides cushion, ŌĆ£shock absorberŌĆØ ’éŚ Enclosed environment ’éŚ Other than veins and arteries, there is only one exitŌĆöwhere brain stem exits the base of the skull to become the spinal cord ’éŚ This is why we have the pressure problem
- 4. Brain Anatomy ’éŚ Surface of the brain is wrinkled with deep folds ’éŚ Increase the surface area of the brain in a small space ’éŚ Compact, efficient ’éŚ Allows for more connections ’éŚ Cortical structures on surface ’éŚ Subcortical structures deeper in brain
- 5. Brain Anatomy ’éŚ Neo-cortex or Cortical Structures ’éŚ Each hemisphere divided into 4 lobes ’éŚ Frontal, temporal, occipital, parietal ’éŚ ŌĆ£ThinkingŌĆØ portion of the brain ’éŚ Subcortical Structures ’éŚ Life sustaining structures/functions ’éŚ White matter ŌĆō communication between different brain regions ’éŚ Brain stem controls heart rate, breathing, temperature, arousal/ wakefulness ’éŚ May be affected by focal damage or generalized mechanisms (swelling, compression, diffuse/shear injury, anoxia)
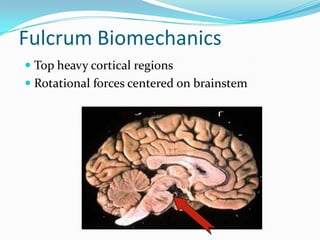
- 6. Anatomical Relationships ’éŚ Grey-white distinction ’éŚ Grey = cell body ’éŚ White = axons ’éŚ Axons carry information to/from outside world ’éŚ Converge in brainstem
- 7. Fulcrum Biomechanics ’éŚ Top heavy cortical regions ’éŚ Rotational forces centered on brainstem
- 8. Neuropathology of Brain Injury ’éŚ Acquired Brain Injury (ABI): ’éŚ Any injury that happens within the brain itself at the cellular level ’éŚ Traumatic Brain Injury (TBI) ’éŚ Non-Traumatic Brain Injury (TBI)
- 9. Neuropathology of Brain Injury Traumatic Brain Injury (TBI): ’éŚ Outside force impacts head hard enough to cause brain to move within the skull or the force directly hurts the brain ’éŚ Examples: motor vehicle collisions, falls, firearms, sports, physical violence, etc. ’éŚ Closed Head Injury vs. Open Head Injury
- 10. Neuropathology of Brain Injury Non-Traumatic Brain Injury (TBI): ’éŚ Does not involve external mechanical force ’éŚ Examples: stroke, aneurysm, insufficient oxygen (anoxia/hypoxia) or blood supply (ischemia), infectious disease, AVM, etc.
- 11. Neuropathology of TBI ’éŚ Contusions: Bruising ’éŚ blood vessels in or around brain are damaged or broken ’éŚ Hemorrhage ’éŚ bleeding from blood vessel leakage rupture ’éŚ Hematoma ’éŚ Localized pooling of blood that occurs from hemorrhaging. ’éŚ Can be large or small
- 12. Neuropathology in TBI ’éŚ Edema ’éŚ Swelling in brain tissue ’éŚ Or influx of fluid ’éŚ Causes increased intracranial pressure (ICP) ’éŚ Enclosed space: Increased pressure on all brain tissue, can put pressure on stem ’éŚ Treatments: ’éŚ Medically induced coma ’éŚ Brain diuretic (reduce fluid/water) ’éŚ Placement of shunt (drain) ’éŚ Craniectomy (remove portion of skull bone to allow extra space for swelling)
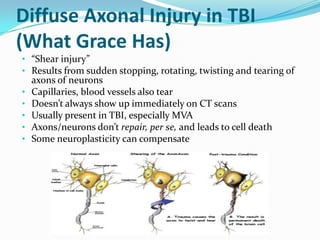
- 13. Diffuse Axonal Injury in TBI (What Grace Has) ŌĆó ŌĆ£Shear injuryŌĆØ ŌĆó Results from sudden stopping, rotating, twisting and tearing of axons of neurons ŌĆó Capillaries, blood vessels also tear ŌĆó DoesnŌĆÖt always show up immediately on CT scans ŌĆó Usually present in TBI, especially MVA ŌĆó Axons/neurons donŌĆÖt repair, per se, and leads to cell death ŌĆó Some neuroplasticity can compensate
- 14. Anoxia/Hypoxia ’éŚ Anoxic Brain Injury ’éŚ Brain does not receive any oxygen. Cells in the brain need oxygen to survive ’éŚ Anoxic Anoxia: no oxygen supplied to the brain ’éŚ Anemic Anoxia: blood that does not carry enough oxygen ’éŚ Toxic Anoxia: toxins that block oxygen in the blood ’éŚ Hypoxic Brain Injury ’éŚ Brain receives some, but not enough oxygen ’éŚ Common causes: ’éŚ Cardiovascular disease or trauma, asphyxia (e.g., drowning), chest trauma, electrocution, severe asthma attack, poisoning, substance overdose
- 15. Chemical Changes ’éŚ Brain is very efficientŌĆöproduces at the cellular level only what it needs and needs everything it produces ’éŚ Brain injury may cause neurochemical imbalance ’éŚ Neurotransmitters: ’éŚ E.g., Serotonin ’āĀ mood ’éŚ Medications may be given: ’éŚ Parlodel for arousal ’éŚ Ritalin for focused attention & arousal ’éŚ Mood stabilizers, antidepressants may be beneficial ’éŚ Damage to pituitary gland can effect hormone disruptions, sleep/wake cycles can be affected
- 16. STORMING ’éŚ Hypothalamic Instability ’éŚ ANS poorly regulated by central brain mechanisms ’éŚ Elevated blood pressure ’éŚ Fever ’éŚ Tachycardia ’éŚ Rapid respirations ’éŚ Sweating ’éŚ May or may not be stimulated ’éŚ Not a sign of improvement ’éŚ Can be very difficult to watch
- 18. Two Tracks at Shepherd Center ’éŚ PREP Program (Pre-Rehabilitation Education Program) ’éŚ Rancho Levels 1-3, passive therapies to keep body conditioned, and ready for progression to full rehab ’éŚ Stimulation for coma emergence ’éŚ Rehabilitation Program ’éŚ Full Rehabilitation Program ’éŚ Dual diagnosis SCI patients ’éŚ Patient has both a spinal cord injury and brain injury ’éŚ They frequently co-occur (e.g., car accidents, falls, etc)
- 19. Overview: Pre-Rehabilitation Education Program ’éŚ Reflexive & generalized responses without purposeful or goal-directed behaviors ’éŚ Goal: Provide best possible environment for emergence ’éŚ 1.5 hours daily of passive therapies ’éŚ Minimize complications of immobility ’éŚ Increase quality and quantity of responses to stimuli ’éŚ Recovery is not dependent on amount of stimulationŌĆö more is not necessarily better ’éŚ Neurostimulants - medications to promote arousal ’éŚ Establish and maintain medical stability ’éŚ Family training, home modifications, preparation for discharge
- 20. Levels of Arousal ’éŚ Severity of Initial Injury ’éŚ Glasgow Coma Scale (GCS 3-15) ’éŚ Length of reduced arousal ’éŚ Rancho Scale Levels ’éŚ Only for TBI ’éŚ Range from 1-10 ’éŚ Levels 1-3 are low-level consciousness (Prep Program) ’éŚ Level 4-10 full Rehab program ’éŚ Traditional arousal terminology ’éŚ Assessing functional abilities
- 21. PREP Program (cont.) ’éŚ JFK Coma Recovery Scale (Speech Therapy) ’éŚ Useful in documenting even slight improvements ’éŚ Visual: Startle, localization, pursuit, tracking, object recognition ’éŚ Auditory: Startle, localization, consistency ’éŚ Oromotor: Oral movement, vocalization, verbalization, ’éŚ Communication: Accuracy, consistency ’éŚ Arousal ’éŚ Neurobehavioral Examination (Neuropsychology) ’éŚ Family Education and feedback
- 22. LEVEL 1 ’éŚ Rancho 1: No Responses : Total Assistance ’éŚ Arousal Level: Coma ’éŚ Functional Abilities ’éŚ Eyes closed ’éŚ No response to any stimuli
- 23. LEVEL 2 ’éŚ Rancho 2: Generalized Responses ’éŚ Arousal Level: Vegetative State ’éŚ Functional Abilities ’éŚ Eyes open ’éŚ Generalized responses ’éŚ Reflexive behaviors (grasping) ’éŚ Non-purposeful movements ’éŚ Fragments of coordinated movement ’éŚ Vocalization but not verbalization
- 24. LEVEL 3 (GraceŌĆÖs Current Level) ’éŚ Rancho 3: Localized Responses ’éŚ Arousal Level: Minimally Conscious ’éŚ Functional Abilities ’éŚ Localized responses ’éŚ Intelligible verbalization ’éŚ Purposeful behavior ’éŚ Responses still inconsistent
- 25. PREP Program (cont.) ’éŚ Emergence criteria ’éŚ Interactive communication to simple, concrete questions or requests ’éŚ Following commands ’éŚ Yes/no responses ’éŚ Allow time ’éŚ OR functional use of 2 objects ’éŚ Reliable: With all staff, not reflexive ’éŚ Consistent: 85% of the time ’éŚ Motor and language impairments can interfere
- 26. Neural Recovery ’éŚ Everyone is DIFFERENT ’éŚ Time & Biology ’éŚ Types of recovery ’éŚ Recovery from secondary effects ’éŚ Cortical reorganization ’éŚ Nearby cells may take on additional work ’éŚ Limitations ’éŚ We do not make new brain cells ’éŚ Limited capacity for reorganization
- 27. PREP Program (cont.) ’éŚ Speak in a comforting, positive, and familiar way. Be mindful of delayed response time. ’éŚ We cannot be sure how much cognitive processing is occurring. ’éŚ When visitors are present, focus on the patient. ’éŚ Limit the number of visitors. Keep visits short ŌĆō rest is essential ’éŚ Provide the patient with pictures, music, and personal items that are comforting and familiar. ’éŚ There are opportunities to assist with patient care as directed by nurses.
- 28. PREP - Going HomeŌĆ” ’éŚ Each patientŌĆÖs recovery rate is unique ’éŚ Recovery continues after discharge ’éŚ For some patients, familiar environment can be stimulation for emergence ’éŚ We want you to feel competent to go home ’éŚ Family Training Day ’éŚ Marcus Bridge Program, telehealth ’éŚ Continued support ’éŚ Return for rehabilitation if appropriate
- 29. Factors That Can Affect Recovery ’éŚ Age ’éŚ Prior brain injury ’éŚ Previous health status ’éŚ Length of PTA ’éŚ Time since injury ’éŚ How much tissue was damaged ’éŚ Focal injuries are more resistant to recovery ’éŚ Language, executive functions, ataxia are more resistant ’éŚ Substance abuse, smoking tobacco ’éŚ Adaptive functioning before injury ’éŚ Family involvement ’éŚ More therapy hours are not related to amount of recovery
- 30. Family ’éŚ You know your loved one better than we do ’éŚ Your knowledge about their emotional and physical needs is valuable to us and to their recovery ’éŚ Your participation and involvement is helpful ’éŚ Feelings of loss, sadness, anger, guilt, and frustration are common and normal ’éŚ You do not have to go through this alone- help is available
- 31. Stages of Family Adjustment 1. DENIAL 1. TRUST ’éŚ Just listen ’éŚ Encourage hope ’éŚ Self-care advice ’éŚ One foot in front of other 2. BEWILDERMENT 2. OBJECTIVITY 3. DESPAIR 3. LONG-TERM PLAN 4. INSIGHT 4. IN DEPTH FEEDBACK 5. MOURNING 5. PERMISSION 6. ACCEPTANCE 6. RESOURCES
- 32. Self Care is Essential ’éŚ You have to be healthy in order to be able to take care of someone else ’éŚ Break the stress response cycle ’éŚ Rest, eat well, get some exercise ’éŚ Practice whatever gives you strength, peace, hope ’éŚ Manage your physical & emotional energy ’éŚ Asking for help is a valuable skill, not a weakness ’éŚ Find people who will help you and then let them ’éŚ Share your feelings with trusted others ’éŚ This is your chance for a break before your loved one is discharged