Proximal myopathy and causes
- 1. Proximal myopathy and causes AAM. Amjath Medicine 4th batch Fhcs-eusl
- 2. Myopathy • Any diseases of muscles. • Usually affect muscle without involving the nervous system or any disorders of neuro muscular junction. • Most common presentation is weakness. • When it is present in proximal muscles: it is called as proximal myopathy.
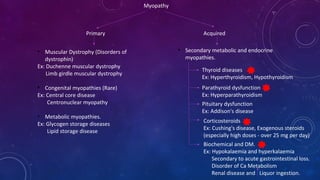
- 3. Myopathy Primary Acquired • Muscular Dystrophy (Disorders of dystrophin) Ex: Duchenne muscular dystrophy Limb girdle muscular dystrophy • Congenital myopathies (Rare) Ex: Central core disease Centronuclear myopathy • Metabolic myopathies. Ex: Glycogen storage diseases Lipid storage disease • Secondary metabolic and endocrine myopathies. Thyroid diseases Ex: Hyperthyroidism, Hypothyroidism Parathyroid dysfunction Ex: Hyperparathyroidism Pituitary dysfunction Ex: Addison's disease Corticosteroids Ex: Cushing's disease, Exogenous steroids (especially high doses - over 25 mg per day) Biochemical and DM. Ex: Hypokalaemia and hyperkalaemia Secondary to acute gastrointestinal loss. Disorder of Ca Metabolism Renal disease and Liquor ingestion.
- 4. Cont….. Acquired • Dermatomyositis and polymyositis : these are inflammatory myopathies with weakness, endomysial inflammation and elevated muscle enzymes. Ex: Primary polymyositis (idiopathic adult). Dermatomyositis (idiopathic adult). Polymyositis or dermatomyositis associated with neoplasia. • Drug-induced myopathy Ex: Statins (Atrovastatin, Simvastatin) Corticosteroids Cocaine • Infectious causes Ex: HIV Coxsackie viruses Influenza • Polymyalgia rheumatica: Proximal myopathy with associated muscle tenderness.
- 7. Clinical features • Weakness predominantly affecting proximal muscle groups (shoulder and limb girdles) is typical • Weakness manifests itself in different ways at different ages Ex: Motor delay in the toddler years. Reduced muscle strength and power in older children and adults. • Myalgia may occur in inflammatory myopathies. • Muscle-stretch reflexes are preserved. • Somatosensory reflexes are preserved. • Muscle tone normal or reduced.
- 8. history • Common symptoms a. Symmetrical proximal muscle weakness. b. Malaise. c. Fatigue. d. Absence of sensory symptoms (paraesthesia). e. Atrophy of muscles (and reduced reflexes) occurs late with myopathies (early with neuropathy).
- 9. • How acute are the symptoms? a. Weakness over hours suggests toxic cause or episodic paralysis. b. Weakness developing over days - consider dermatomyositis or rhabdomyolysis. c. Weakness over weeks suggests polymyositis, steroid myopathy, endocrine myopathy. •. Pain and tenderness without weakness - consider other causes. •. Which muscle groups are affected? a. Proximal muscle groups - difficulty rising from chair, climbing stairs, shaving, hair combing. b. Distal muscles - difficulty walking (flapping gait), grasping, handwriting. •. Metabolic myopathies present with: a. Difficulty with exercise. b. Cramps and myalgia with exercise (early with glycogen storage disorders and after prolonged exercise with lipid storage disorders). c. Myoglobinuria. d. Progressive muscle weakness in some metabolic myopathies.
- 10. • Past medical history: a. Autoimmune disease: Systemic lupus erythematosus, Rheumatoid arthritis, Polyarteritis nodosa. b. Endocrine disease c. Renal disease d. Alcoholism •. Family history: a. Muscular dystrophy. b. Other relevant conditions or myopathies. •. Medication: a. Steroids b. Lipid-lowering drugs c. Alcohol d. Colchicine e. Heroin
- 11. examination • Symmetrical proximal muscle weakness. • Muscle tenderness very rare with myopathy. • Fever with inflammatory causes. • There is usually no wasting but there may be hypertrophy of muscle (atrophy is a late sign). • Reflexes and sensation usually normal. • Hypotonia is common in some myopathies (for example, congenital myopathies). • There may be helpful additional signs such as the skin changes of dermatomyositis. • Urine should be examined - myoglobinuria in acute alcoholic myopathy can cause renal tubular necrosis.
- 12. Investigations • Blood and urine tests These, together with electrocardiogram (ECG) examination, are most useful in acute situations. a. Creatine kinase (with isoenzymes) - level may be 50-100 x normal reference range. b. Electrolytes including calcium and magnesium. c. Serum myoglobin. d. Urea and serum creatinine. e. Urinalysis and urine microscopy - myoglobinuria inferred by positive urinalysis with few red cells at microscopy. f. FBC. g. ESR. h. Antinuclear antibodies.
- 13. • ECG May show a. Changes of hypokalaemia - increased P-R interval, U waves, wide QRS and nonspecific ST-T changes. b. Sinus arrhythmias, deep Q waves and elevated R waves precordially.
- 14. • Muscle biopsy • Electromyography • Magnetic resonance imaging (MRI)