тАПтАПRF - ┘Ж╪│ ╪о╪й.pptx
- 1. Acute Respiratory Failure Deanship of Graduate Studies & Scientific Research, 21 September University of Medical & Applied Sciences. Presented by: Mosa Alfageh BS, MsRC Student Supervised by: Prof: Ahmed Fad dahmesh BS, MsRC Student
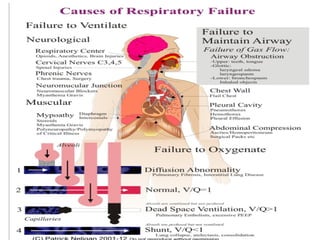
- 4. Introduction тАв The body depends on the coordinated functioning of the central nervous system, pulmonary system, heart, and vascular system to achieve effective respiration. Respiratory failure arises when one or more of these systems or organs fail to maintain optimal functioning. If respiratory failure occurs rapidly, such that compensatory mechanisms cannot accommodate, or if these compensatory mechanisms are overwhelmed, acute respiratory failure develops.
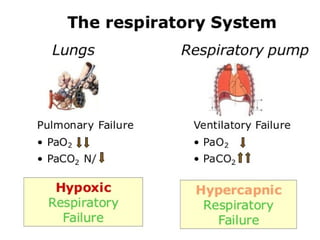
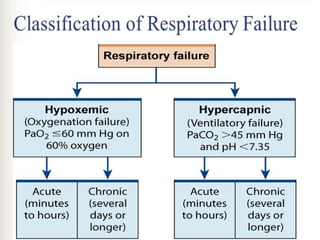
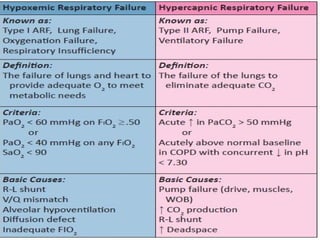
- 5. Definition 11/23/2024 MsRC 5 Failure in one or both gas exchange functions: oxygenation and carbon dioxide elimination In practice Pao2 <60mmhg or PaCO2>50mmhg Respiratory failure is a syndrome of inadequate gas exchange due to dysfunction of one or more essential components of the respiratory system
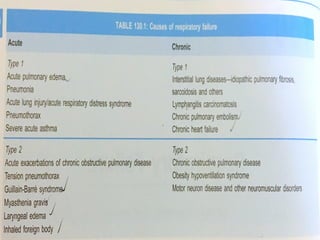
- 6. Types of respiratory failure 11/23/2024 MsRC 6 TYPE 1 (HYPOXEMIC ): PO2 < 60 mmHg on room air. TYPE 2 (HYPERCAPNIC / VENTILATORY): PCO2 > 50 mmHg TYPE 3 (PERI-OPERATIVE): This is generally a subset of type 1 failure but is sometimes considered separately because it is so common. TYPE 4 (SHOCK): secondary to cardiovascular instability.
- 7. TYPE 3 (PERI-OPERATIVE): 11/23/2024 MsRC 7 Residual anesthesia effects, post-operative pain, and abnormal abdominal mechanics contribute to decreasing FRC and progressive collapse of dependant lung units. Causes of post-operative atelectasis include; тАв Decreased FRC тАв Supine/ obese/ ascites тАв Anesthesia тАв Upper abdominal incision тАв Airway secretions
- 8. TYPE 4 (SHOCK): 11/23/2024 MsRC 8 Describes patients who are intubated and ventilated in the process of resuscitation for shock тАв cardiogenic тАв hypovolemic тАв septic
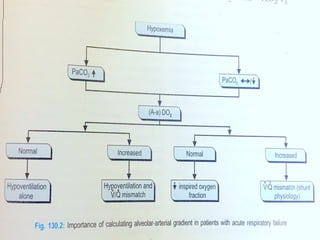
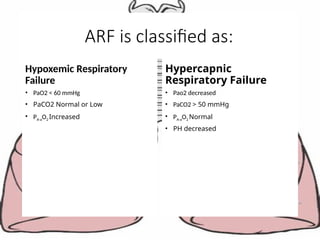
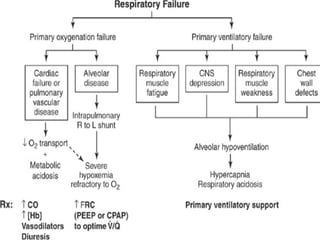
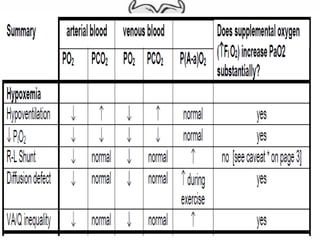
- 12. ARF is classified as: Hypoxemic Respiratory Failure тАв PaO2 < 60 mmHg тАв PaCO2 Normal or Low тАв PA-aO2 Increased Hypercapnic Respiratory Failure тАв Pao2 decreased тАв PaCO2 > 50 mmHg тАв PA-aO2 Normal тАв PH decreased
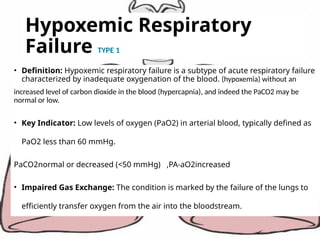
- 16. Hypoxemic Respiratory Failure TYPE 1 тАв Definition: Hypoxemic respiratory failure is a subtype of acute respiratory failure characterized by inadequate oxygenation of the blood. (hypoxemia) without an increased level of carbon dioxide in the blood (hypercapnia), and indeed the PaCO2 may be normal or low. тАв Key Indicator: Low levels of oxygen (PaO2) in arterial blood, typically defined as PaO2 less than 60 mmHg. PaCO2normal or decreased (<50 mmHg) ,PA-aO2increased тАв Impaired Gas Exchange: The condition is marked by the failure of the lungs to efficiently transfer oxygen from the air into the bloodstream.
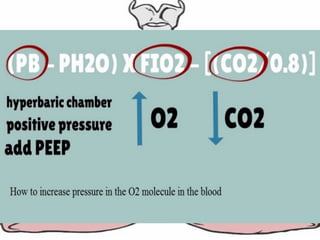
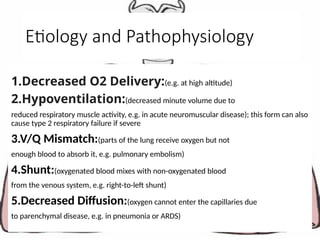
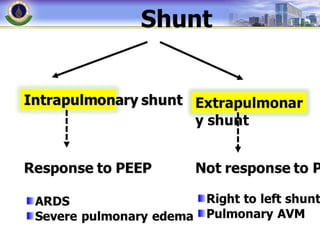
- 17. Etiology and Pathophysiology 1.Decreased O2 Delivery:(e.g. at high altitude) 2.Hypoventilation:(decreased minute volume due to reduced respiratory muscle activity, e.g. in acute neuromuscular disease); this form can also cause type 2 respiratory failure if severe 3.V/Q Mismatch:(parts of the lung receive oxygen but not enough blood to absorb it, e.g. pulmonary embolism) 4.Shunt:(oxygenated blood mixes with non-oxygenated blood from the venous system, e.g. right-to-left shunt) 5.Decreased Diffusion:(oxygen cannot enter the capillaries due to parenchymal disease, e.g. in pneumonia or ARDS)
- 18. 1.Decreased O2 Delivery: Examples- тАв A decrease in barometric pressure [e.g. breathing at high altitude]. тАв A decrease in FIO2 тАУ accidental [e.g. anesthetist does not supply enough oxygen or improper installation of oxygen supply lines or a leak in the breathing circuit]. тАв P(A-a)O2 normal тАв PaCO2 is decreased. This reduction in PaCO2 (hypocapnia) is due to hyperventilation in response to hypoxemia. тАв Peripheral chemoreceptors sense the low arterial PO2 and initiate an increase in ventilation through their input to the medullary respiratory centre 11/23/2024 MsRC 18 Etiology and Pathophysiology
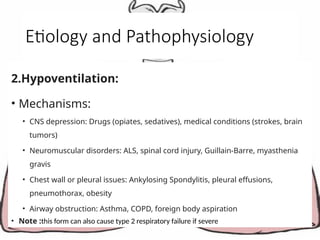
- 19. Etiology and Pathophysiology 2.Hypoventilation: тАв Mechanisms: тАв CNS depression: Drugs (opiates, sedatives), medical conditions (strokes, brain tumors) тАв Neuromuscular disorders: ALS, spinal cord injury, Guillain-Barre, myasthenia gravis тАв Chest wall or pleural issues: Ankylosing Spondylitis, pleural effusions, pneumothorax, obesity тАв Airway obstruction: Asthma, COPD, foreign body aspiration тАв Note :this form can also cause type 2 respiratory failure if severe
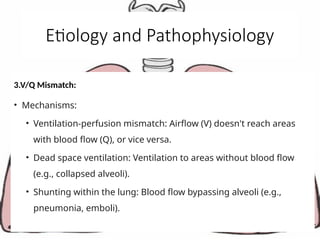
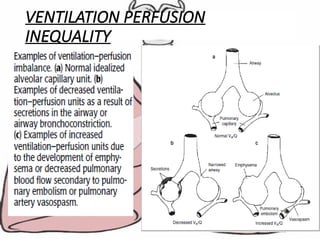
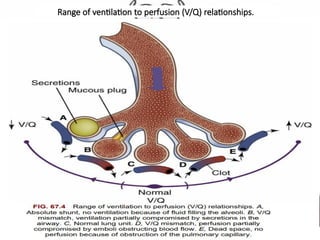
- 20. Etiology and Pathophysiology 3.V/Q Mismatch: тАв Mechanisms: тАв Ventilation-perfusion mismatch: Airflow (V) doesn't reach areas with blood flow (Q), or vice versa. тАв Dead space ventilation: Ventilation to areas without blood flow (e.g., collapsed alveoli). тАв Shunting within the lung: Blood flow bypassing alveoli (e.g., pneumonia, emboli).
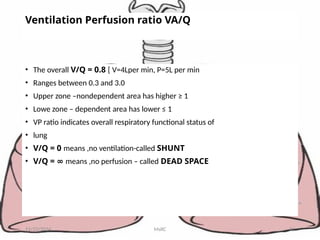
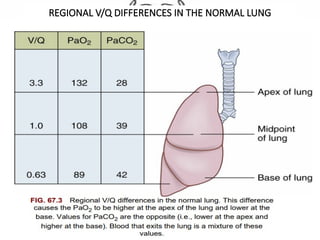
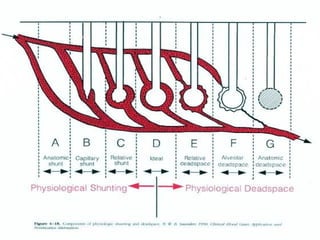
- 21. Ventilation Perfusion ratio VA/Q тАв The overall V/Q = 0.8 [ V=4Lper min, P=5L per min тАв Ranges between 0.3 and 3.0 тАв Upper zone тАУnondependent area has higher тЙе 1 тАв Lowe zone тАУ dependent area has lower тЙд 1 тАв VP ratio indicates overall respiratory functional status of тАв lung тАв V/Q = 0 means ,no ventilation-called SHUNT тАв V/Q = тИЮ means ,no perfusion тАУ called DEAD SPACE 11/23/2024 MsRC 21
- 22. SHUNTS have different effects on arterial PCO2 (PaCO2 ) than on arterial PO2 (PaO2 ). Blood passing through under ventilated alveoli tends to retain its CO2 and does not take up enough O2. тАв Blood traversing over ventilated alveoli gives off an excessive amount of CO2, but cannot take up increased amount of O2 because of the shape of the oxygen-hemoglobin (oxy-Hb) dissociation curve. тАв from the over ventilated alveoli to compensate for the under ventilated alveoli. Thus, with Shunt, PACO2 -to-PaCO2 gradients are small, and PAO2 -to-PaO2 gradients are usually large. 11/23/2024 MsRC 22
- 23. VENTILATION PERFUSION INEQUALITY тАв PaCO2 is normal тАв P(A-a)O2 is elevated тАв VA/Q inequality is the most common cause of hypoxemia in disease states 11/23/2024 MsRC 23
- 24. VENTILATION PERFUSION INEQUALITY тАв The distribution of ventilation varies with common events, such as changes in body posture, lung volumes, and age. тАв Increasing age produces a gradual increase in the degree of the VA/Q inequality. тАв VentilationтАУperfusion imbalance exists even in the normal lung, depending on the region, but remains fairly tightly regulated when assessing normal lung aggregate function 11/23/2024 MsRC 24
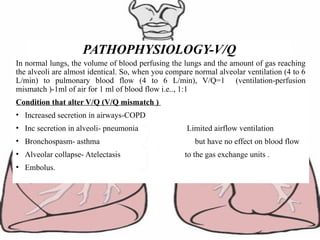
- 27. In normal lungs, the volume of blood perfusing the lungs and the amount of gas reaching the alveoli are almost identical. So, when you compare normal alveolar ventilation (4 to 6 L/min) to pulmonary blood flow (4 to 6 L/min), V/Q=1 (ventilation-perfusion mismatch )-1ml of air for 1 ml of blood flow i.e.., 1:1 Condition that alter V/Q (V/Q mismatch ) тАв Increased secretion in airways-COPD тАв Inc secretion in alveoli- pneumonia Limited airflow ventilation тАв Bronchospasm- asthma but have no effect on blood flow тАв Alveolar collapse- Atelectasis to the gas exchange units . тАв Embolus. PATHOPHYSIOLOGY-V/Q
- 28. REGIONAL V/Q DIFFERENCES IN THE NORMAL LUNG
- 29. Range of ventilation to perfusion (V/Q) relationships.
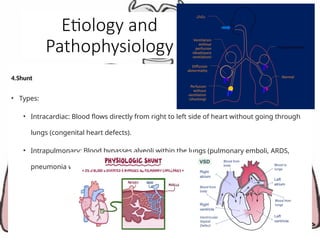
- 30. Etiology and Pathophysiology 4.Shunt тАв Types: тАв Intracardiac: Blood flows directly from right to left side of heart without going through lungs (congenital heart defects). тАв Intrapulmonary: Blood bypasses alveoli within the lungs (pulmonary emboli, ARDS, pneumonia with abscesses)
- 31. RIGHT TO LEFT SHUNT тАв Shunt refers to the entry of blood into the systemic arterial system without going through ventilated areas of lung. тАв Shunt may be anatomical or physiological. тАв P(A-a)O2 is elevated. тАв PaCO2 is normal. 11/23/2024 MsRC 31
- 32. RIGHT TO LEFT SHUNT тАвAnatomic shunt: when a portion of blood bypasses the lungs through an anatomic channel. In healthy individuals i) A portion of the bronchial circulationтАЩs (blood supply to the conducting zone of the airways) venous blood drains into the pulmonary vein. ii) A portion of the coronary circulationтАЩs venous blood drains through the thebesian veins into the left ventricle. note: i & ii represent about 2% of the cardiac output and account for 1/3 of the normal P(A-a)O2 observed in health. 11/23/2024 MsRC 32
- 33. RIGHT TO LEFT SHUNT Congenital abnormalities i) intra-cardiac shunt [e.g. Tetralogy of Fallot: ventricular septal defect + pulmonary artery stenosis] ii) intra-pulmonary fistulas [direct communication between a branch of the pulmonary artery and a pulmonary vein]. 11/23/2024 MsRC 33
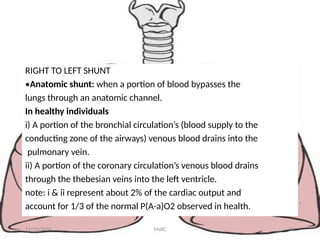
- 34. RIGHT TO LEFT SHUNT Physiologic shunt: In disease states, a portion of the cardiac output goes through the regular pulmonary vasculature but does not come into contact with alveolar air due to filling of the alveolar spaces with fluid [e.g. pneumonia, drowning, pulmonary edema] тАв An important diagnostic feature of a shunt is that the arterial Po2 does not rise to the normal level when the patient is given 100% oxygen to breathe. 11/23/2024 MsRC 34
- 35. RIGHT TO LEFT SHUNT Examples of intrapulmonary shunt. (a) Collapsed and fluid filled alveoli are examples of intrapulmonary shunt. (b) Anomalous blood return of mixed venous blood bypasses the alveolus and thereby contributes to the development of intrapulmonary shunt 11/23/2024 MsRC 35
- 36. Etiology and Pathophysiology тАв 5.Decreased Diffusion тАв Mechanism: тАв Oxygen can't easily cross from air sacs to the bloodstream due to: тАв Thickened alveolar walls (scarring, protein buildup) тАв Fluid in air sacs (edema, ARDS) тАв Less membrane surface area (emphysema, lung collapse) тАв Abnormal blood flow in capillaries (shunts, clots)
- 37. Clinical Manifestations тАв 1. Dyspnea (Shortness of Breath) тАв 2. Cyanosis тАв 3. Tachypnea тАв 4. Confusion or Altered Mental Status тАв 5. Fatigue тАв 6. Tachycardia 7. Use of Accessory Muscles
- 38. Diagnosis of Hypoxemic RF тАв 1.Hypoventilation: тАв Diagnosis: тАв History and physical examination: Look for signs of respiratory distress, decreased breath sounds. тАв Chest X-ray: May reveal abnormalities like pneumonia or pleural effusions. тАв ABG: Shows elevated CO2 levels and potentially low O2 levels. тАв Pulmonary function tests: Measure lung function and identify airway obstruction.
- 39. Diagnosis of Hypoxemic RF тАв 2.V/Q Mismatch тАв Diagnosis: тАв History and physical examination: Look for signs of respiratory distress and underlying lung conditions. тАв Chest X-ray and CT scan: May show abnormalities like pneumonia or emboli. тАв ABG: May show low O2 levels and potentially elevated CO2 levels. тАв V/Q scan: Helps identify areas of ventilation-perfusion mismatch.
- 40. Diagnosis of Hypoxemic RF тАв 3.Shunt тАв Diagnosis: тАв History and physical examination: Look for signs of right heart strain or pulmonary embolism. тАв Chest X-ray and CT scan: May show enlarged heart or evidence of lung abnormalities. тАв Echocardiogram: To assess heart structure and function. тАв V/Q scan: Helps identify areas of perfusion without ventilation (indicative of shunt).
- 41. Diagnosis of Hypoxemic RF тАв 4.Decreased Diffusion тАв History and physical exam: Look for signs of respiratory distress, abnormal breath sounds, and underlying lung conditions. тАв Chest X-ray and CT scan: May show evidence of lung disease, fluid accumulation, or structural abnormalities. тАв Arterial blood gas (ABG): Shows low oxygen levels (PaO2) and potentially normal or slightly elevated carbon dioxide levels (PaCO2). тАв Pulmonary function tests: Can assess gas exchange efficiency and identify ventilation-perfusion mismatch.
- 42. Treatment 1.Hypoventilation: тАв Address the underlying cause: Reverse drug effects, manage neurological disorders, treat chest wall or airway issues. тАв Non-invasive ventilation (BiPAP) or mechanical ventilation may be needed in severe cases. 2. V/Q Mismatch: тАв Address the underlying cause: Antibiotics for pneumonia, anticoagulation for emboli, ventilation support for ARDS, bronchodilators for COPD. тАв Oxygen therapy to improve oxygenation. тАв Mechanical ventilation may be needed in severe cases.
- 43. Treatment 3.Shunt тАв Depends on the type and cause of shunt. тАв Surgery for congenital heart defects. тАв Anticoagulation for pulmonary emboli. тАв Antibiotics for pneumonia with abscesses. тАв Mechanical ventilation for ARDS. тАв 4.Decreased Diffusion тАв Address the underlying cause: тАв Treat lung disease with medications or surgery тАв Manage fluid accumulation with diuretics or other therapies тАв Anticoagulation for pulmonary emboli тАв Oxygen therapy to improve oxygenation тАв Mechanical ventilation may be needed in severe cases
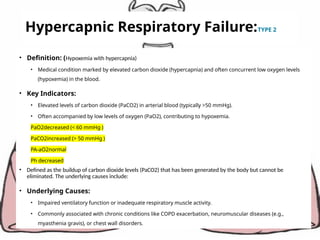
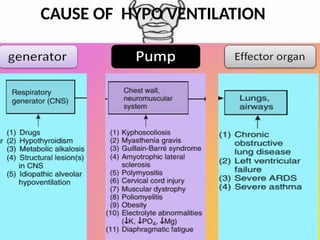
- 45. Hypercapnic Respiratory Failure:TYPE 2 тАв Definition: (Hypoxemia with hypercapnia) тАв Medical condition marked by elevated carbon dioxide (hypercapnia) and often concurrent low oxygen levels (hypoxemia) in the blood. тАв Key Indicators: тАв Elevated levels of carbon dioxide (PaCO2) in arterial blood (typically >50 mmHg). тАв Often accompanied by low levels of oxygen (PaO2), contributing to hypoxemia. PaO2decreased (< 60 mmHg ) PaCO2increased (> 50 mmHg ) PA-aO2normal Ph decreased тАв Defined as the buildup of carbon dioxide levels (PaCO2) that has been generated by the body but cannot be eliminated. The underlying causes include: тАв Underlying Causes: тАв Impaired ventilatory function or inadequate respiratory muscle activity. тАв Commonly associated with chronic conditions like COPD exacerbation, neuromuscular diseases (e.g., myasthenia gravis), or chest wall disorders.
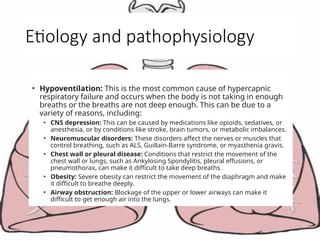
- 46. Etiology and pathophysiology тАв Hypoventilation: This is the most common cause of hypercapnic respiratory failure and occurs when the body is not taking in enough breaths or the breaths are not deep enough. This can be due to a variety of reasons, including: тАв CNS depression: This can be caused by medications like opioids, sedatives, or anesthesia, or by conditions like stroke, brain tumors, or metabolic imbalances. тАв Neuromuscular disorders: These disorders affect the nerves or muscles that control breathing, such as ALS, Guillain-Barre syndrome, or myasthenia gravis. тАв Chest wall or pleural disease: Conditions that restrict the movement of the chest wall or lungs, such as Ankylosing Spondylitis, pleural effusions, or pneumothorax, can make it difficult to take deep breaths. тАв Obesity: Severe obesity can restrict the movement of the diaphragm and make it difficult to breathe deeply. тАв Airway obstruction: Blockage of the upper or lower airways can make it difficult to get enough air into the lungs.
- 47. CAUSE OF HYPO VENTILATION
- 48. 11/23/2024 48
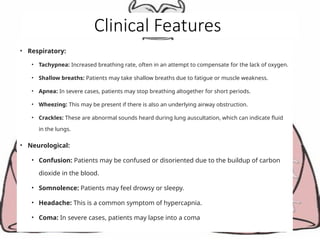
- 51. Clinical Features тАв Respiratory: тАв Tachypnea: Increased breathing rate, often in an attempt to compensate for the lack of oxygen. тАв Shallow breaths: Patients may take shallow breaths due to fatigue or muscle weakness. тАв Apnea: In severe cases, patients may stop breathing altogether for short periods. тАв Wheezing: This may be present if there is also an underlying airway obstruction. тАв Crackles: These are abnormal sounds heard during lung auscultation, which can indicate fluid in the lungs. тАв Neurological: тАв Confusion: Patients may be confused or disoriented due to the buildup of carbon dioxide in the blood. тАв Somnolence: Patients may feel drowsy or sleepy. тАв Headache: This is a common symptom of hypercapnia. тАв Coma: In severe cases, patients may lapse into a coma
- 52. Diagnosis 1. ABG 2.Chest X-ray 3.Pulmonary Function Tests (PFTs) 4.Neuromuscular Studies 5.Capnography 6.Continuous Oxygen Saturation Monitoring
- 53. Treatments тАв Bronchodilators тАв Oxygen Therapy тАв Non-Invasive Ventilation (NIV): BiPAP and CPAP тАв Corticosteroids тАв Mechanical Ventilation
- 54. тАв Shunt versus Dead space тАв тАв Anatomic shunt cause deoxygenated blood to тАв transfer into the systemic circulation without passing тАв through the pulmonary circulation: тАв тАв Bronchial and Thebesian Veins тАв тАв Accounts for 75% of the difference between alveolar тАв O2 and arterial O2. 11/23/2024 MsRC 56
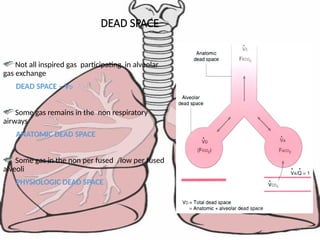
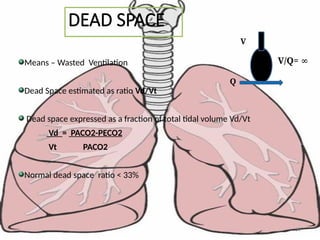
- 57. 59 DEAD SPACE Not all inspired gas participating in alveolar gas exchange DEAD SPACE тАУ VD Some gas remains in the non respiratory airways ANATOMIC DEAD SPACE Some gas in the non per fused /low per fused alveoli PHYSIOLOGIC DEAD SPACE
- 58. 60 DEAD SPACE Means тАУ Wasted Ventilation Dead Space estimated as ratio Vd/Vt Dead space expressed as a fraction of total tidal volume Vd/Vt Vd = PACO2-PECO2 Vt PACO2 Normal dead space ratio < 33% Q V V/Q= тИЮ
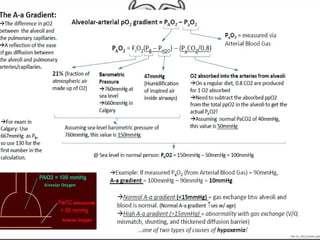
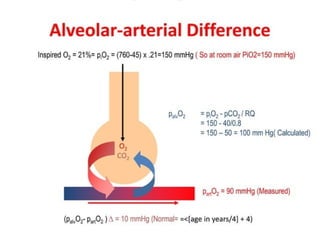
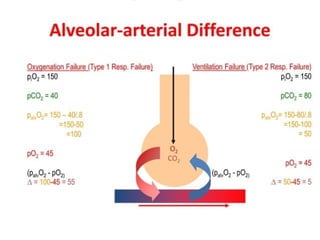
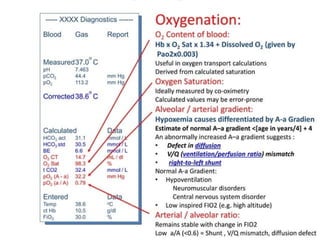
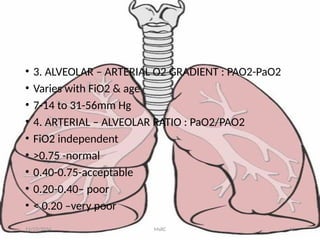
- 59. тАв 3. ALVEOLAR тАУ ARTERIAL O2 GRADIENT : PAO2-PaO2 тАв Varies with FiO2 & age тАв 7-14 to 31-56mm Hg тАв 4. ARTERIAL тАУ ALVEOLAR RATIO : PaO2/PAO2 тАв FiO2 independent тАв >0.75 -normal тАв 0.40-0.75-acceptable тАв 0.20-0.40тАУ poor тАв < 0.20 тАУvery poor 11/23/2024 MsRC 61
- 60. тАв The AlveolarтАУarterial gradient ( AтАУa gradient тАв is a measure of the difference between тАв the alveolar concentration (A) of oxygen and тАв the arterial (a) concentration of oxygen. тАв It is used in diagnosing the source of hypoxemia. тАв It helps to assess the integrity of alveolar capillary unit. тАв For example, in high altitude, the arterial oxygen [[PaO2]] тАв is low but only because the alveolar oxygen (PAO2) is also тАв low. However, in states of ventilation perfusion тАв mismatch, such as pulmonary embolism or right-to-left тАв shunt, oxygen is not effectively transferred from тАв the alveoli to the blood which results in elevated A-a тАв gradient 11/23/2024 MsRC 62
Editor's Notes
- #2: ABCDEF bundle Element A (Assess, Prevent, and Manage Pain) Element B (Both SATs and SBTs) Element C (Choice of Analgesia and Sedation) Element D (Delirium Assess and Manage) Element E (Early Mobility and Exercise) Element F (Family Engagement/Empowerment)
- #4: Ventilation Perfusion Diffusion
- #30: SHUNTS have different effects on arterial PCO2 (PaCO2 ) than on arterial PO2 (PaO2 ). Blood passing through under ventilated alveoli tends to retain its CO2 and does not take up enough O2. яГШBlood traversing over ventilated alveoli gives off an excessive amount of CO2, but cannot take up increased amount of O2 because of the shape of the oxygen-hemoglobin (oxy-Hb) dissociation curve. яГШ 2 from the over ventilated alveoli to compensate for the under ventilated alveoli. яГШThus, with Shunt, PACO2 -to-PaCO2 gradients are small, and PAO2 -to-PaO2 gradients are usually large.
- #45: HYPOVENTILATION тАв Hypoventilation is used here to refer to conditions in which alveolar ventilation is abnormally low in relation to oxygen uptake or carbon dioxide output. тАв Alveolar ventilation is the volume of fresh inspired gas going to the alveoli (i.e. NonтАУdead space ventilation). тАв Hypoventilation occurs when the alveolar ventilation is reduced and the alveolar Po2 therefore settles out at a lower level than normal. For the same reason, the alveolar Pco2, and therefore arterial Pco2, are also raised
- #46: Increased airways resistance (chronic obstructive pulmonary disease, asthma, suffocation) тАв Reduced breathing effort (drug effects, brain stem lesion, extreme obesity) тАв A decrease in the area of the lung available for gas exchange (such as in chronic bronchitis) тАв Neuromuscular problems (Guillain-Barr├й syndrome,motor neuron disease) тАв Deformed (kyphoscoliosis), rigid (ankylosing spondylitis), or flail chest.
- #47: HYPOVENTILATION тАв P(A-a)O2 is normal. тАв PaCO2 is elevated (hypercapnia) тАв Increasing the fraction of inspired oxygen (FIO2) can alleviate the hypoxemia and the hypercapnia can be corrected by mechanically ventilating the patient to eliminate CO2.

![1.Decreased O2 Delivery:
Examples-
тАв A decrease in barometric pressure [e.g. breathing at high
altitude].
тАв A decrease in FIO2 тАУ accidental [e.g. anesthetist does not
supply enough oxygen or improper installation of oxygen
supply lines or a leak in the breathing circuit].
тАв P(A-a)O2 normal
тАв PaCO2 is decreased. This reduction in PaCO2 (hypocapnia) is
due to hyperventilation in response to hypoxemia.
тАв Peripheral chemoreceptors sense the low arterial PO2 and
initiate an increase in ventilation through their input to the
medullary respiratory centre
11/23/2024 MsRC 18
Etiology and Pathophysiology](https://image.slidesharecdn.com/rf-241123193130-002849ac/85/RF-pptx-18-320.jpg)
![RIGHT TO LEFT SHUNT
Congenital abnormalities
i) intra-cardiac shunt [e.g. Tetralogy of Fallot:
ventricular
septal defect + pulmonary artery stenosis]
ii) intra-pulmonary fistulas [direct communication
between a branch of the pulmonary artery and a
pulmonary vein].
11/23/2024 MsRC 33](https://image.slidesharecdn.com/rf-241123193130-002849ac/85/RF-pptx-33-320.jpg)
![RIGHT TO LEFT SHUNT
Physiologic shunt: In disease states, a portion of the
cardiac output goes through the regular pulmonary vasculature
but
does not come into contact with alveolar air due to filling of
the alveolar spaces with fluid [e.g. pneumonia, drowning,
pulmonary edema]
тАв An important diagnostic feature of a shunt
is that the arterial Po2 does not rise to the
normal level when the patient is given 100%
oxygen to breathe.
11/23/2024 MsRC 34](https://image.slidesharecdn.com/rf-241123193130-002849ac/85/RF-pptx-34-320.jpg)
![тАв The AlveolarтАУarterial gradient ( AтАУa gradient
тАв is a measure of the difference between
тАв the alveolar concentration (A) of oxygen and
тАв the arterial (a) concentration of oxygen.
тАв It is used in diagnosing the source of hypoxemia.
тАв It helps to assess the integrity of alveolar capillary unit.
тАв For example, in high altitude, the arterial oxygen [[PaO2]]
тАв is low but only because the alveolar oxygen (PAO2) is also
тАв low. However, in states of ventilation perfusion
тАв mismatch, such as pulmonary embolism or right-to-left
тАв shunt, oxygen is not effectively transferred from
тАв the alveoli to the blood which results in elevated A-a
тАв gradient
11/23/2024 MsRC 62](https://image.slidesharecdn.com/rf-241123193130-002849ac/85/RF-pptx-60-320.jpg)