Rheumatic fever
- 2. Etiology âĒ Acute rheumatic fever is a systemic disease of childhood,often recurrent that follows group A beta hemolytic streptococcal infection âĒ It is a delayed non-suppurative sequelae to URTI with GABH streptococci. âĒ It is a diffuse inflammatory disease of connective tissue,primarily involving heart,blood vessels,joints, subcut.tissue and CNS 2
- 3. Epidemiology âĒ Ages 5-15 yrs are most susceptible âĒ Rare <3 yrs âĒ Girls>boys âĒ Common in 3rd world countries âĒ Environmental factors-- over crowding, poor sanitation, poverty, âĒ Incidence more during fall ,winter & early spring 3
- 4. Pathogenesis âĒ Delayed immune response to infection with group.A beta hemolytic streptococci. âĒ After a latent period of 1-3 weeks, antibody induced immunological damage occur to heart valves,joints, subcutaneous tissue & basal ganglia of brain 4
- 5. Group A Beta Hemolytic Streptococcus âĒ Strains that produces rheumatic fever - M types l, 3, 5, 6,18 & 24 âĒ Pharyngitis- produced by GABHS can lead to- acute rheumatic fever , rheumatic heart disease & post strept. Glomerulonepritis âĒ Skin infection- produced by GABHS leads to post streptococcal glomerulo nephritis only. It will not result in Rh.Fever or carditis 5
- 6. Clinical Features 1.Arthritis âĒ Migratory polyarthritis, involving major joints âĒ Commonly involved joints-knee,ankle,elbow & wrist âĒ Occur in 80%,involved joints are exquisitely tender âĒ In children below 5 yrs arthritis usually mild but carditis more prominent âĒ Arthritis do not progress to chronic disease 6
- 7. Clinical Features (Contd) 2.Carditis âĒ Manifest as pancarditis(endocarditis, myocarditis and pericarditis),occur in 40-50% of cases âĒ Carditis is the only manifestation of rheumatic fever that leaves a sequelae & permanent damage to the organ âĒ Valvulitis occur in acute phase âĒ Chronic phase- fibrosis,calcification & stenosis of heart valves. 7
- 8. Clinical Features (Contd) 3.Sydenham Chorea âĒ Occur in 5-10% of cases âĒ Mainly in girls of 1-15 yrs age âĒ May appear even 6 months after the attack of rheumatic fever âĒ Clinically manifest as-clumsiness, deterioration of handwriting,emotional lability or grimacing of face 8
- 9. Clinical Features (Contd) 4.Erythema Marginatum âĒ Occur in <5%. âĒ Unique, transient lesions of 1-2 inches in size âĒ Pale center with red irregular margin âĒ More on trunks & limbs & non-itchy âĒ Worsens with application of heat âĒ Often associated with chronic carditis 9
- 10. Clinical Features (Contd) 5.Subcutaneous nodules âĒ Occur in 10% âĒ Painless,pea-sized,palpable nodules âĒ Mainly over extensor surfaces of joints,spine,scapulae & scalp âĒ Associated with strong seropositivity âĒ Always associated with severe carditis 10
- 11. Clinical Features (Contd) Other features (Minor features) âĒ Fever â Low grade âĒ Arthralgia âĒ Pallor âĒ Anorexia âĒ Loss of weight 11
- 12. Laboratory Findings âĒ High ESR âĒ Anemia, leucocytosis âĒ Elevated C-reactive protien âĒ ASO titre >200. (Peak value attained at 3 weeks,then comes down to normal by 6 weeks) âĒ Anti-DNAse B test âĒ Throat culture-GABHstreptococci 12
- 13. Laboratory Findings (Contd) âĒ ECG- prolonged PR interval âĒ Echo - valve edema,mitral regurgitation, LA & LV dilatation,pericardial effusion,decreased contractility 13
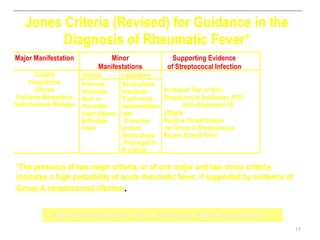
- 14. Diagnosis âĒ Rheumatic fever is mainly a clinical diagnosis âĒ No single diagnostic sign or specific laboratory test available for diagnosis âĒ Diagnosis based on MODIFIED JONES CRITERIA 14
- 15. Jones Criteria (Revised) for Guidance in the Diagnosis of Rheumatic Fever* Major Manifestation Minor Supporting Evidence Manifestations of Streptococal Infection Carditis Clinical Laboratory Polyarthritis Previous Acute phase Chorea rheumatic reactants: Increased Titer of Anti- Erythema Marginatum fever or Erythrocyte Streptococcal Antibodies ASO Subcutaneous Nodules rheumatic sedimentation (anti-streptolysin O), heart disease rate, others Arthralgia C-reactive Positive Throat Culture Fever protein, for Group A Streptococcus leukocytosis Recent Scarlet Fever Prolonged P- R interval *The presence of two major criteria, or of one major and two minor criteria, indicates a high probability of acute rheumatic fever, if supported by evidence of Group A streptococcal nfection. Recommendations of the American Heart Association 15
- 16. Treatment âĒ Step I - primary prevention (eradication of streptococci) âĒ Step II - anti inflammatory treatment (aspirin,steroids) âĒ Step III- supportive management & management of complications âĒ Step IV- secondary prevention (prevention of recurrent attacks) 16
- 17. STEP I: Primary Prevention of Rheumatic Fever (Treatment of Streptococcal Tonsillopharyngitis) Agent Dose Mode Duration Benzathine penicillin G 600 000 U for patients Intramuscular Once 27 kg (60 lb) 1 200 000 U for patients >27 kg or Penicillin V Children: 250 mg 2-3 times daily Oral 10 d (phenoxymethyl penicillin) Adolescents and adults: 500 mg 2-3 times daily For individuals allergic to penicillin Erythromycin: 20-40 mg/kg/d 2-4 times daily Oral 10 d Estolate (maximum 1 g/d) or Ethylsuccinate 40 mg/kg/d 2-4 times daily Oral 10 d (maximum 1 g/d) Recommendations of American Heart Association 17
- 18. Step II: Anti inflammatory treatment Clinical condition Drugs Arthritis only Aspirin 75-100 mg/kg/day,give as 4 divided doses for 6 weeks (Attain a blood level 20- 30 mg/dl) Carditis Prednisolone 2-2.5 mg/kg/day, give as two divided doses for 2 weeks Taper over 2 weeks & while tapering add Aspirin 75 mg/kg/day for 2 weeks. Continue aspirin alone 100 mg/kg/day for another 4 weeks 18
- 19. 3.Step III: Supportive management & management of complications âĒ Bed rest âĒ Treatment of congestive cardiac failure: -digitalis,diuretics âĒ Treatment of chorea: -diazepam or haloperidol âĒ Rest to joints & supportive splinting 19
- 20. STEP IV : Secondary Prevention of Rheumatic Fever (Prevention of Recurrent Attacks) Agent Dose Mode Benzathine penicillin G 1 200 000 U every 4 weeks* Intramuscular or Penicillin V 250 mg twice daily Oral or Sulfadiazine 0.5 g once daily for patients 27 kg (60 lb Oral 1.0 g once daily for patients >27 kg (60 lb) For individuals allergic to penicillin and sulfadiazine Erythromycin 250 mg twice daily Oral *In high-risk situations, administration every 3 weeks is justified and recommended Recommendations of American Heart Association 20
- 21. Prognosis âĒ Rheumatic fever can recur whenever the individual experience new GABH streptococcal infection,if not on prophylactic medicines âĒ Good prognosis for older age group & if no carditis during the initial attack âĒ Bad prognosis for younger children & those with carditis with valvar lesions 21