Cervical Cancer Screening
- 1. Screening for Cervical Cancer Sarah McCormick MSIII Kansas City University of Medicine and Biosciences
- 2. Cervical Cancer Risk Factors HPV strains 16 and 18 Smoking Immuno-suppression Early age at first intercourse Multiple sex partner Obesity Multiple pregnancies Family history of cervical cancer
- 3. Screening Pap Smears Every woman who is sexually active or 21 yo Annual tests from ages 21 to 30 After age 30, pap tests may be given every 2 to 3 years, if the previous 3 tests have been negative, no history of CIN 2 or 3, and no increased risk (no DES exposure, not immuno-compromised) >30 HPV testing maybe offered as alternative to cytology, HPV + cytology every 3 years Samples the transition zone where the nonkeratinized stratified squamous epithelium (ectocervix) and simple columnar epithelium (endocervix) meet. 2 Types Papanicolaou Smear Liquid Preparations Thin Prep 1996 (liquid)- most sensitive, viewed twice once by image viewer, then by a lab professional, only test FDA approved for G,C and HPV reflex testing Sure Path 2000 Mono Prep 2006
- 4. Why Screen? Evidence of screening effectiveness only shown from observational studies >50% woman with cervical cancer have never had a pap, were screen only randomly, or did not have a pap in the last 5 years. Canadian study found inverse correlation between pap smears performed and a decrease in mortality rate from cervical and uterine cancer. Woman without a pap smear in the last 5 years had triple the risk of having invasive cervical cancer The IARC found a 90% reduction in cervical cancer incidence from screening adult females
- 5. What Happens at the Lab? Smears are fed into automated systems to be read Abnormal smears are manually read by a lab technician 10% negative smears are reread for quality assurance
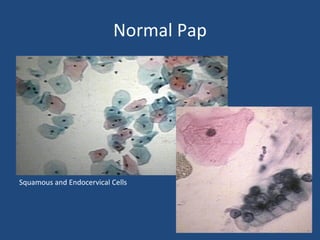
- 6. Normal Pap Squamous and Endocervical Cells
- 7. Abnormal Pap Chlamydia infected cells Koilocytes (HPV infected cells) dark wrinkled nuclei surrounded by clear halo Cells demonstrating dysplasia
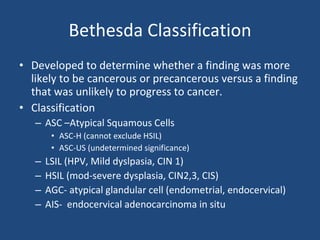
- 8. Bethesda Classification Developed to determine whether a finding was more likely to be cancerous or precancerous versus a finding that was unlikely to progress to cancer. Classification ASC –Atypical Squamous Cells ASC-H (cannot exclude HSIL) ASC-US (undetermined significance) LSIL (HPV, Mild dyslpasia, CIN 1) HSIL (mod-severe dysplasia, CIN2,3, CIS) AGC- atypical glandular cell (endometrial, endocervical) AIS- endocervical adenocarcinoma in situ
- 9. HPV Testing HPV is found in 70-80% cervical cancers, 82% adenocarcinomas, 70% squamous cell carcinomas of the female genital tract Persistent HPV infections cause premalignancies HPV testing with Pap is more sensitive than Pap alone. (94.6% vs 55.4%) Not used as screening test alone due to its poor specificity as compared to the Pap. (94.1% vs 96.8%) Better specificity in woman >30yrs old According to the Population Based Screening Study Amsterdam HPV + Pap screening led to earlier detection of lesions
- 10. HPV Testing Continued Positive HPV refers to the finding of HPV 16 and 18 Negative HPV results refer to the finding of no HPV, a finding of HPV strains not related to cancer, or no cells (bad sample) HPV testing with Pap approaches 100% sensitivity but 10% false positive rate Reflex HPV Test tests ASC-US for HPV from same sample as pap 80% of adolescents may test positive for HPV, so not as effective a test for adolescents
- 11. Follow up Adult Women ASC-US/H Reflex HPV ASC-US + HPV positive- colposcopy ASC-US with negative HPV- repeat Pap 12 mo (most likely inflammation or infection <2% premalignant) Repeat Pap is ASC-US- colpo ASC-H-colpo Adolescents ASC -ASC-US (no reflex test due to high positive rate!)- f/u 12 mo repeat pap If repeat is HSIL or greater-colpo If (ASC, LSIL) repeat pap in 12 mo Combined HPV DNA + Pap For women >30 yo only, no more than q3yrs HPV and cytology positive-colpo HPV positive, cytology negative- repeat 12 mo Persistently positive HPV-colpo
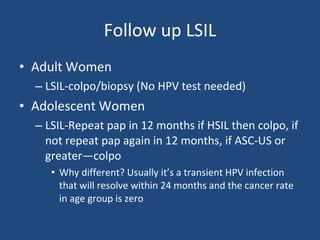
- 12. Follow up LSIL Adult Women LSIL-colpo/biopsy (No HPV test needed) Adolescent Women LSIL-Repeat pap in 12 months if HSIL then colpo, if not repeat pap again in 12 months, if ASC-US or greater—colpo Why different? Usually it’s a transient HPV infection that will resolve within 24 months and the cancer rate in age group is zero
- 13. Follow Up HSIL Adult and Adolescent Women At very high risk of malignancy (>50% have CIN 2 or more) Colpo with biopsy
- 14. Follow up AGS and AIS AGC (Atypical Glandular Cells) and AIS (Adenocarcinoma In Situ) Colpo + biopsy if >35 yo endometrial biopsy
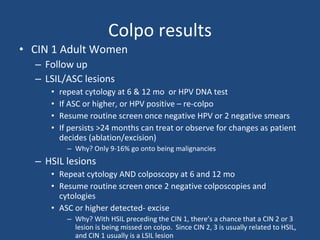
- 15. Colpo results CIN 1 Adult Women Follow up LSIL/ASC lesions repeat cytology at 6 & 12 mo or HPV DNA test If ASC or higher, or HPV positive – re-colpo Resume routine screen once negative HPV or 2 negative smears If persists >24 months can treat or observe for changes as patient decides (ablation/excision) Why? Only 9-16% go onto being malignancies HSIL lesions Repeat cytology AND colposcopy at 6 and 12 mo Resume routine screen once 2 negative colposcopies and cytologies ASC or higher detected- excise Why? With HSIL preceding the CIN 1, there’s a chance that a CIN 2 or 3 lesion is being missed on colpo. Since CIN 2, 3 is usually related to HSIL, and CIN 1 usually is a LSIL lesion
- 16. Colpo Results Continued CIN 1 Adolescent Women (<20 yo) Repeat cytology at 12 mo (then follow HSIL/LSIL procedure) Only 0.4% progress to CIN 3 CIN 2, 3 Adult Women Ablation or Excision Excise if: Suspected microinvasion, Unsatisfactory colposcopy)Lesion, extending into the endocervical canal,Endocervical curettage showing CIN or a glandular abnormality, Lack of correlation between the cytology and colposcopy/biopsies, Suspected adenocarcinoma in situ, Colposcopist unable to rule out invasive disease, Recurrence after an ablative or previous excisional procedure CIN 2, 3 Adolescent Women Repeat colpo and cytology q6months for 24 months 2 normal results-return to routine screening Persistant CIN2-observation Persistant CIN3-Ablation/excision
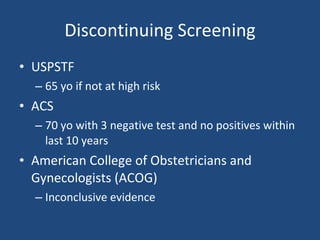
- 17. Discontinuing Screening USPSTF 65 yo if not at high risk ACS 70 yo with 3 negative test and no positives within last 10 years American College of Obstetricians and Gynecologists (ACOG) Inconclusive evidence
- 18. References www.thinprep.com http://www.pathguy.com/lectures/women.htm www.uptodate.com