Shock Presentation Definition, etiology, types and management
- 1. SHOCK MANAGEMENT PRESENTATION BY DR AMINU BELLO DIRECTOR SCHOOL OF NURSING KATSINA
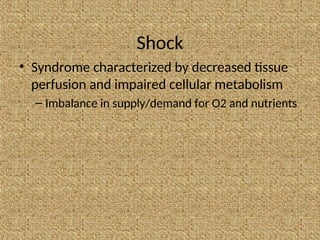
- 2. Shock • Syndrome characterized by decreased tissue perfusion and impaired cellular metabolism – Imbalance in supply/demand for O2 and nutrients
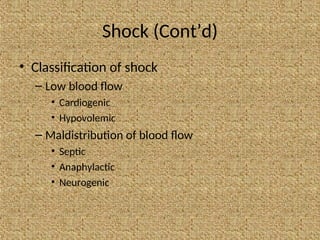
- 3. Shock (Cont’d) • Classification of shock – Low blood flow • Cardiogenic • Hypovolemic – Maldistribution of blood flow • Septic • Anaphylactic • Neurogenic
- 4. Low Blood Flow Carcinogenic Shock • Definition – Systolic or diastolic dysfunction – Compromised cardiac output (CO)
- 5. Low Blood Flow Cardiogenic Shock (Cont’d) • Precipitating causes – Myocardial infarction – Cardiomyopathy – Blunt cardiac injury – Severe systemic or pulmonary hypertension – Cardiac tamponade (Obstructive) – Myocardial depression from metabolic problems
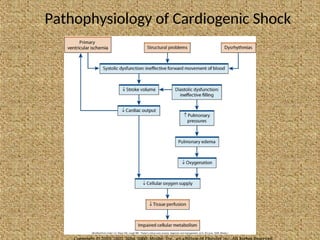
- 6. Pathophysiology of Cardiogenic Shock
- 7. Low Blood Flow Cardiogenic Shock • Early manifestations – Tachycardia – Hypotension – Narrowed pulse pressure – ↑ Myocardial O2 consumption
- 8. Low Blood Flow Cardiogenic Shock (Cont’d) • Physical examination – Tachypnea, pulmonary congestion – Pallor; cool, clammy skin – Decreased capillary refill time – Anxiety, confusion, agitation • ↑ in pulmonary artery wedge pressure • Decreased renal perfusion and UO
- 9. Low Blood Flow Hypovolemic Shock • Absolute hypovolemia: Loss of intravascular fluid volume – Hemorrhage – GI loss (e.g., vomiting, diarrhea) – Fistula drainage – Diabetes insipidus – Hyperglycemia – Diuresis
- 10. Low Blood Flow Hypovolemic Shock (Cont’d) • Relative hypovolemia – Results when fluid volume moves out of the vascular space into extravascular space (e.g., interstitial or intracavitary space) – Termed third spacing
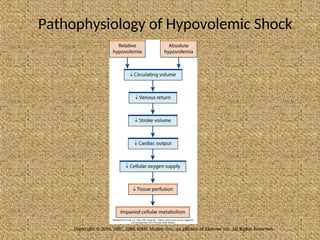
- 11. Pathophysiology of Hypovolemic Shock Copyright © 2010, 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
- 12. Low Blood Flow Hypovolemic Shock • Response to acute volume loss depends on – Extent of injury or insult – Age – General state of health
- 13. Low Blood Flow Hypovolemic Shock (Cont’d) • Clinical manifestations – Anxiety – Tachypnea – Increase in CO, heart rate – Decrease in stroke volume, PAWP, UO • If loss is >30%, blood volume is replaced
- 14. Maldistribution of Blood Flow Neurogenic Shock • Hemodynamic phenomenon that can occur within 30 minutes of a spinal cord injury at the fifth thoracic (T5) vertebra or above and can last up to 6 weeks • Results in massive vasodilation leading to pooling of blood in vessels
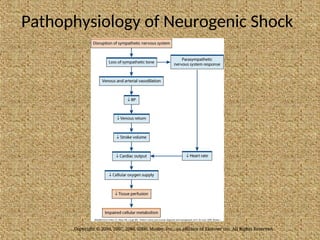
- 15. Pathophysiology of Neurogenic Shock Copyright © 2010, 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
- 16. Maldistribution of Blood Flow Neurogenic Shock (Cont’d) • Clinical manifestations – Hypotension – Bradycardia – Temperature dysregulation (resulting in heat loss) – Dry skin – Poikilothermia (taking on the temperature of the environment)
- 17. Maldistribution of Blood Flow Anaphylactic Shock • Acute, life-threatening hypersensitivity reaction – Massive vasodilation – Release of mediators – ↑ Capillary permeability
- 18. Maldistribution of Blood Flow Anaphylactic Shock (Cont’d) • Clinical manifestations – Anxiety, confusion, dizziness – Tachycardia, tachypnea, hypotension – Wheezing, stridor – Sense of impending doom – Chest pain
- 19. Maldistribution of Blood Flow Anaphylactic Shock (Cont’d) • Clinical manifestations – Swelling of the lips and tongue, angioedema – Wheezing, stridor – Flushing, pruritus, urticaria – Respiratory distress and circulatory failure
- 20. Maldistribution of Blood Flow Septic Shock • Sepsis: Systemic inflammatory response to documented or suspected infection • Severe sepsis = Sepsis + Organ dysfunction
- 21. Maldistribution of Blood Flow Septic Shock (Cont’d) • Septic shock = Presence of sepsis with hypotension despite fluid resuscitation + Presence of tissue perfusion abnormalities
- 22. Maldistribution of Blood Flow Septic Shock (Cont’d) • Mortality rates as high as 50% • Primary causative organisms – Gram-negative and gram-positive bacteria – Endotoxin stimulates inflammatory response
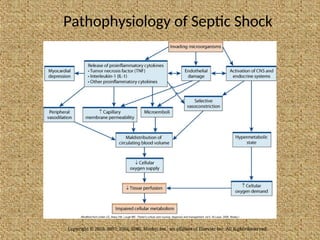
- 23. Pathophysiology of Septic Shock Copyright © 2010, 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
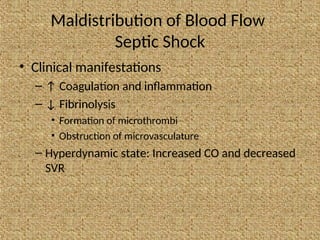
- 24. Maldistribution of Blood Flow Septic Shock • Clinical manifestations – ↑ Coagulation and inflammation – ↓ Fibrinolysis • Formation of microthrombi • Obstruction of microvasculature – Hyperdynamic state: Increased CO and decreased SVR
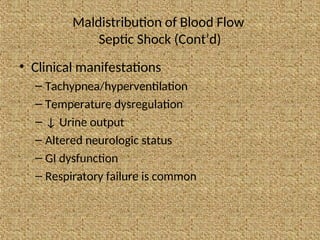
- 25. Maldistribution of Blood Flow Septic Shock (Cont’d) • Clinical manifestations – Tachypnea/hyperventilation – Temperature dysregulation – ↓ Urine output – Altered neurologic status – GI dysfunction – Respiratory failure is common
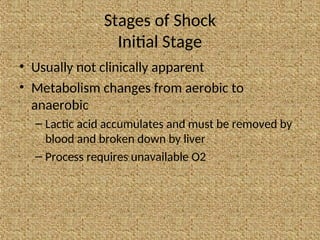
- 26. Stages of Shock Initial Stage • Usually not clinically apparent • Metabolism changes from aerobic to anaerobic – Lactic acid accumulates and must be removed by blood and broken down by liver – Process requires unavailable O2
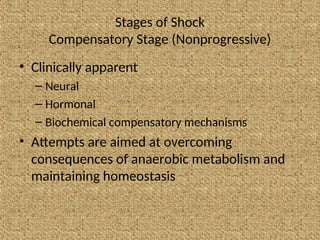
- 27. Stages of Shock Compensatory Stage (Nonprogressive) • Clinically apparent – Neural – Hormonal – Biochemical compensatory mechanisms • Attempts are aimed at overcoming consequences of anaerobic metabolism and maintaining homeostasis
- 28. Stages of Shock Compensatory Stage (Nonprogressive) • Baroreceptors in carotid and aortic bodies activate SNS in response to ↓ BP – Vasoconstriction while blood to vital organs maintained • ↓ Blood to kidneys activates renin– angiotensin system – ↑ Venous return to heart, CO, BP
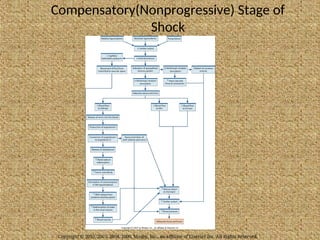
- 29. Compensatory(Nonprogressive) Stage of Shock Copyright © 2010, 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
- 30. Stages of Shock Compensatory Stage (Nonprogressive Cont’d) • If perfusion deficit corrected, patient recovers with no residual sequelae • If deficit not corrected, patient enters progressive stage
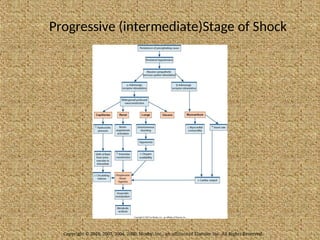
- 31. Stages of Shock Progressive Stage (intermediate) • Begins when compensatory mechanisms fail • Aggressive interventions to prevent multiple organ dysfunction syndrome
- 32. Progressive (intermediate)Stage of Shock Copyright © 2010, 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
- 33. Stages of Shock Progressive Stage (intermediate Cont’d) • Hallmarks of ↓ cellular perfusion and altered capillary permeability: • Leakage of protein into interstitial space • ↑ Systemic interstitial edema
- 34. Stages of Shock Progressive Stage (intermediate Cont’d) • Anasarca (severe generalized edema) • Fluid leakage affects solid organs and peripheral tissues • ↓ Blood flow to pulmonary capillaries
- 35. Stages of Shock Progressive Stage (intermediate Cont’d) • Movement of fluid from pulmonary vasculature to interstitium • Pulmonary edema • Bronchoconstriction • ↓ Residual capacity
- 36. Stages of Shock Progressive Stage (intermediate Cont’d) • Fluid moves into alveoli • Edema • Decreased surfactant • Worsening V/Q mismatch • Tachypnea • Crackles • Increased work of breathing
- 37. Stages of Shock Progressive Stage (intermediate Cont’d) • CO begins to fall • Decreased peripheral perfusion • Hypotension • Weak peripheral pulses • Ischemia of distal extremities
- 38. Stages of Shock Progressive Stage (intermediate Cont’d) • Myocardial dysfunction results in • Dysrhythmias • Ischemia • Myocardial infarction • End result: Complete deterioration of cardiovascular system
- 39. Stages of Shock Progressive Stage (intermediate Cont’d) • Mucosal barrier of GI system becomes ischemic • Ulcers • Bleeding • Risk of translocation of bacteria • Decreased ability to absorb nutrients
- 40. Stages of Shock Progressive Stage (intermediate Cont’d) • Liver fails to metabolize drugs and wastes • Jaundice • Elevated enzymes • Loss of immune function • Risk for DIC and significant bleeding
- 41. Stages of Shock Progressive Stage (intermediate Cont’d) • Acute tubular necrosis/acute renal failure
- 42. Stages of Shock Refractory Stage (Irreversible) • Exacerbation of anaerobic metabolism • Accumulation of lactic acid • ↑ Capillary permeability
- 43. Stages of Shock Refractory Stage • Profound hypotension and hypoxemia • Tachycardia worsens • Decreased coronary blood flow • Cerebral ischemia
- 44. Stages of Shock Refractory Stage (Cont’d) • Failure of one organ system affects others • Recovery unlikely
- 45. Diagnostic Studies • Through history and physical examination • No single study to determine shock – Blood studies • Elevation of lactate • Base deficit – 12-lead ECG – Chest x-ray – Hemodynamic monitoring
- 46. Collaborative Care • Successful management includes – Identification of patients at risk for shock – Integration of the patient’s history, physical examination, and clinical findings to establish a diagnosis
- 47. Collaborative Care (Cont’d) • Successful management includes – Interventions to control or eliminate the cause of the decreased perfusion – Protection of target and distal organs from dysfunction – Provision of multisystem supportive care
- 48. Collaborative Care (Cont’d) • General management strategies – Ensure patent airway – Maximize oxygen delivery
- 49. Collaborative Care (Cont’d) • Cornerstone of therapy for septic, hypovolemic, and anaphylactic shock = volume expansion – Isotonic crystalloids (e.g., normal saline) for initial resuscitation of shock
- 50. Collaborative Care (Cont’d) • Volume expansion – If the patient does not respond to 2 to 3 L of crystalloids, blood administration and central venous monitoring may be instituted • Complications of fluid resuscitation – Hypothermia – Coagulopathy
- 51. Collaborative Care (Cont’d) • Primary goal of drug therapy = correction of decreased tissue perfusion – Vasopressor drugs (e.g., epinephrine) • Achieve/maintain MAP >60 to 65 mm Hg • Reserved for patients unresponsive to other therapies
- 52. Collaborative Care (Cont’d) • Primary goal of drug therapy = correction of decreased tissue perfusion – Vasodilator therapy (e.g., nitroglycerin [cardiogenic shock], nitroprusside [noncardiogenic shock]) • Achieve/maintain MAP >60 to 65 mm Hg
- 53. Collaborative Care (Cont’d) • Nutrition is vital to decreasing morbidity from shock – Initiate enteral nutrition within the first 24 hours
- 54. Collaborative Care (Cont’d) • Nutrition is vital to decreasing morbidity from shock – Initiate parenteral nutrition if enteral feedings contraindicated or fail to meet at least 80% of the caloric requirements – Monitor protein, nitrogen balance, BUN, glucose, electrolytes
- 55. Collaborative Care Cardiogenic Shock • Restore blood flow to the myocardium by restoring the balance between O2 supply and demand • Thrombolytic therapy • Angioplasty with stenting • Emergency revascularization • Valve replacement
- 56. Collaborative Care Cardiogenic Shock (Cont’d) • Hemodynamic monitoring • Drug therapy (e.g., diuretics to reduce preload) • Circulatory assist devices (e.g., intra-aortic balloon pump, ventricular assist device)
- 57. Collaborative Care Hypovolemic Shock • Management focuses on stopping the loss of fluid and restoring the circulating volume • Fluid replacement is calculated using a 3:1 rule (3 ml of isotonic crystalloid for every 1 ml of estimated blood loss)
- 58. Collaborative Care Septic Shock • Fluid replacement (e.g., 6 to 10 L of isotonic crystalloids and 2 to 4 L of colloids) to restore perfusion • Hemodynamic monitoring • Vasopressor drug therapy; vasopressin for patients refractory to vasopressor therapy
- 59. Collaborative Care Septic Shock (Cont’d) • Intravenous corticosteroids for patients who require vasopressor therapy, despite fluid resuscitation, to maintain adequate BP
- 60. Collaborative Care Septic Shock (Cont’d) • Antibiotics after obtaining cultures (e.g., blood, wound exudate, urine, stool, sputum) • Drotrecogin alfa (Xigris) – Major side effect: Bleeding
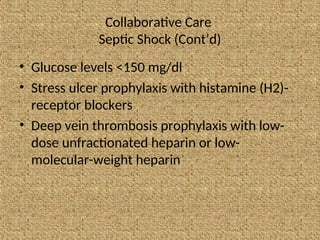
- 61. Collaborative Care Septic Shock (Cont’d) • Glucose levels <150 mg/dl • Stress ulcer prophylaxis with histamine (H2)- receptor blockers • Deep vein thrombosis prophylaxis with low- dose unfractionated heparin or low- molecular-weight heparin
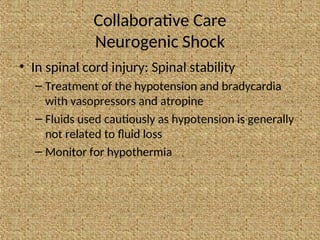
- 62. Collaborative Care Neurogenic Shock • In spinal cord injury: Spinal stability – Treatment of the hypotension and bradycardia with vasopressors and atropine – Fluids used cautiously as hypotension is generally not related to fluid loss – Monitor for hypothermia
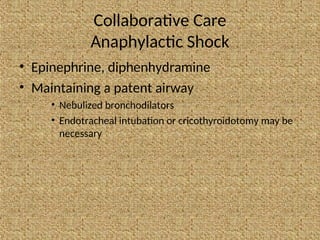
- 63. Collaborative Care Anaphylactic Shock • Epinephrine, diphenhydramine • Maintaining a patent airway • Nebulized bronchodilators • Endotracheal intubation or cricothyroidotomy may be necessary
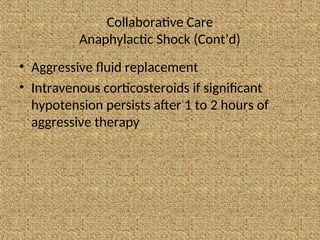
- 64. Collaborative Care Anaphylactic Shock (Cont’d) • Aggressive fluid replacement • Intravenous corticosteroids if significant hypotension persists after 1 to 2 hours of aggressive therapy
- 65. Nursing Assessment (Cont’d) • ABCs: Airway, breathing, and circulation • Focused assessment of tissue perfusion – Vital signs – Peripheral pulses – Level of consciousness – Capillary refill – Skin (e.g., temperature, color, moisture) – Urine output
- 66. Nursing Assessment (Cont’d) • Brief history – Events leading to shock – Onset and duration of symptoms • Details of care received before hospitalization • Allergies • Vaccinations
- 67. Nursing Diagnoses • Ineffective tissue perfusion: Renal, cerebral, cardiopulmonary, gastrointestinal, hepatic, and peripheral • Fear • Potential complication: Organ ischemia/dysfunction
- 68. Planning • Goals for patient – Assurance of adequate tissue perfusion – Restoration of normal or baseline BP – Return/recovery of organ function – Avoidance of complications from prolonged states of hypoperfusion
- 69. Nursing Implementation • Health Promotion – Identify patients at risk (e.g., elderly patients, those with debilitating illnesses or who are immunocompromised, surgical or accidental trauma patients)
- 70. Nursing Implementation (Cont’d) • Health Promotion – Planning to prevent shock (e.g., monitoring fluid balance to prevent hypovolemic shock, maintenance of handwashing to prevent spread of infection)
- 71. Nursing Implementation (Cont’d) • Acute Interventions – Monitor the patient’s ongoing physical and emotional status to detect subtle changes in the patient’s condition – Plan and implement nursing interventions and therapy
- 72. Nursing Implementation (Cont’d) • Acute Interventions – Evaluate the patient’s response to therapy – Provide emotional support to the patient and family – Collaborate with other members of the health team when warranted
- 73. Nursing Implementation (Cont’d) • Neurologic status: Orientation and level of consciousness • Cardiac status – Continuous ECG – VS, capillary refill – Hemodynamic parameters: central venous pressure, PA pressures, CO, PAWP – Heart sounds: Murmurs, S3, S4
- 74. Nursing Implementation (Cont’d) • Respiratory status – Respiratory rate and rhythm – Breath sounds – Continuous pulse oximetry – Arterial blood gases – Most patients will be intubated and mechanically ventilated
- 75. Nursing Implementation (Cont’d) • Urine output • Tympanic or pulmonary arterial temperature • Skin: Temperature, pallor, flushing, cyanosis, diaphoresis, piloerection • Bowel sounds
- 76. Nursing Implementation (Cont’d) • Nasogastric drainage/stools for occult blood • I&O, fluid and electrolyte balance • Oral care/hygiene based on O2 requirements • Passive/active range of motion
- 77. Nursing Implementation (Cont’d) • Assess level of anxiety and fear – Medication PRN – Talk to patient – Visit from clergy – Family involvement – Comfort measures – Privacy – Call light within reach
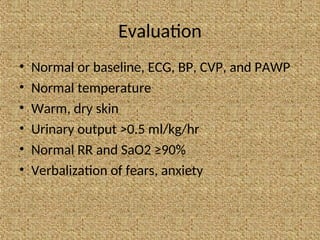
- 78. Evaluation • Normal or baseline, ECG, BP, CVP, and PAWP • Normal temperature • Warm, dry skin • Urinary output >0.5 ml/kg/hr • Normal RR and SaO2 ≥90% • Verbalization of fears, anxiety
- 79. THANK YOU VERY MUCH FOR YOUR ATTENTION.

![Collaborative Care (Cont’d)
• Primary goal of drug therapy = correction of
decreased tissue perfusion
– Vasodilator therapy (e.g., nitroglycerin
[cardiogenic shock], nitroprusside [noncardiogenic
shock])
• Achieve/maintain MAP >60 to 65 mm Hg](https://image.slidesharecdn.com/shockpresentation-240806062754-b5ed903a/85/Shock-Presentation-Definition-etiology-types-and-management-52-320.jpg)