Sjogrens's Syndrome
- 1. By Farshid Mokhberi Shahid Beheshti University Of Medical Sciences & Health services
- 2. Definition  Sjogren’s syndrome is a late onset chronic systemic autoimmune disease characterized by lymphocytic infiltration and destruction of the salivary and lacrimal glands resulting in dry mouth(xerostomia) and dryness and atrophy of conjunctiva and cornea (keratoconjunctivits sicca).  Swedish Ophthalmologist Henrik Sjogren who first described it (1933)
- 3. ETIOLOGY  Female : Male = 9 : 1  4/5/6th decade  Autoimmune ; HLA-B8 / DR3 ,although DR4 is more closely associated with syndrome occuring with raynaud’s phenomenon Pathogenesis of Sjogren’s syndrome is believed to be multifactorial. Known to be autoimmune, but studies suggest that the disease process has genetic, environmental(EBV/HCV) and hormonal(associated with high prevalence in women,esp estrogen) components
- 5.  Lymphocyte and plasma cell infiltration  Auto- antibody production (to ‘Ro’)  Connective tissue proliferation  Glandular cell apoptosis  atrophy of glandular structures in affected tissues (salivary glands, sebaceous glands, sweat glands)
- 6. Clinical Types ÔÇó PRIMARY : Alone ÔÇó SECONDARY : associated underlying connective tissue diseases (RA / SLE / Scleroderma ) ÔÇó SICCA SYNDROME : Xerophthalmia/ Xerostomia /Internal Organ / Bone Inv ÔÉò This disease is caused by an immune-mediated inflammation of salivary,lacrimal and sweat glands as Sicca Syndrome or with internal organ involvement.
- 7. Clinical Features ÔÇó Glandular manifestation ÔÇó Dry mouth (Xerostomia) due to decreased production of saliva by salivary glands Cracked, peeling and atrophic appearance of the lips. Dry and fissured tongue
- 8. Teeth : ÔÇó multilpe carries and early loss
- 9. ÔÇó Chronic oral candidiasis is frequent. ÔÇó Parotid Gland Enlargement
- 10.  Lacrimal Gland Involvement – Dryness of eyes causes keratoconjuctivitis sicca.  Burning itchy sensation in the eyes.
- 11. Skin manifestation  Xeroderma, pruritus and scaling  Annular erythema, Papular Erythema  Raynaud’s syndrome  Hyperglobulinemic Purpura  Vitiligo  Sweating abnormalities  Cutaneous Amyloidosis  Alopecia—diffuse and generalized
- 12. OTHER MANIFESTATIONS Joint symptoms: Arthralgia and arthritis Myalgia and myositis ENT : Sinusitis / Hearing Loss GI : GERD Respiratory: Interstitial pneumonitis, pulmonary fibrosis and pulmonary hypertension Nephrology : Interstitial nephritis, Renal Tubular Acidosis Neurology : migraine, neuropathies, cerebral vasculitis
- 14. Diagnosis ÔÇó hypergammaglobulinemia (IgG>IgA>IgM),ANA(>50%) elevated total protein and sedimentation rate. ÔÇó Anti-Ro and Anti-La Antibodies occur in approximately 60% of patients with Sjogren's syndrome ÔÇó Histolgy of skin shows an absence of sebaceous glands and decrease in the sweat glands.
- 15. Biopsy of labial salivary glands Ly lymphocytic and plasma cells infiltrate Two excretory ducts and 3 mucous salivary gland acini are seen
- 16. SCHIRMER’S TEST German Ophthalmologist Otto Schirmer  determines whether the eye produces enough tears to keep it moist  This test is used when a person experiences very dry eyes or excessive watering of the eyes
- 17. SCHIRMER’S TEST 1. Normal which is ≥15 mm wetting of the paper after 5 minutes 2. Mild which is 14-9 mm wetting of the paper after 5 minutes 3. Moderate which is 8-4 mm wetting of the paper after 5 minutes 4. Severe which is <4 mm wetting of the paper after 5 minutes.
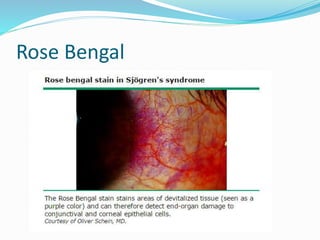
- 19. Rose Bengal
- 20. Revised classification criteria for Sjogren’s Syndrome 1-Ocular symptoms • Dry eyes for more than 3 months • Sensation of sand or gravel in the eyes • Need for tear substitutes more than 3 times a day 2-Oral Symptoms • Dry mouth for more than 3 months • Recurrently or Persistently swollen salivary glands • Need liquids to swallow dry food 3-Ocular Signs • Schirmer’s test • Rose bangal test 4-Salivary gland involvement 5- Autoantibodies Anti Ro and Anti La
- 21. Criteria For primary ÔÇó In patients without any potentially associated disease, primary SS may be defined as follows: ÔÇó a. The presence of any four of the six items is indicative of primary SS, as long as either item 4 (Histopathology) or 6 (Serology) is positive. ÔÇó b. The presence of any three of the four objective criteria items (that is, items 3, 4, 5) For secondary ÔÇó In patients with a potentially associated disease, the presence of item 1 or item 2 plus any two from among items 3, 4, and 5 may be considered as indicative of secondary
- 22. Treatment  Symptomatic treatment for dryness of eyes – by lubricating agents such as 0.5% methylcellulose eye drops for 4-5 times daily.  Cyclosporine ocular drops  Bromhexine 16 mg TDS has been found to increase the lacrimal secretion.  Artificial saliva and cyclosporin(2.5-5mg/kg), for xerostomia.  Routine dental care  Steam inhalation may help dryness of the respiratory tract.
- 23.  Candidiasis – topical nystatin 3times/day for a week  Systemic – ketoconazole 200-400mg/day or fluconazole 50-100 mg/day or itraconazole -100mg/day for 2 weeks  Systemic steroids are effective in reducing parotid swelling  hydroxychloroquine 200 mg daily is useful
- 24. Refrences ÔÇó WWW.UPTODATE.COM ÔÇó WWW.MEDSCAPE.COM ÔÇó WWW.EMEDICINE.COM ÔÇó WWW.PUBMED.COM ÔÇó WWW.WEBMD.COM ÔÇó WWW.MYOCLINIC.COM
- 25. Thanks For Your Attention