SP Abortion.pptx++++++++++++++++++++77777
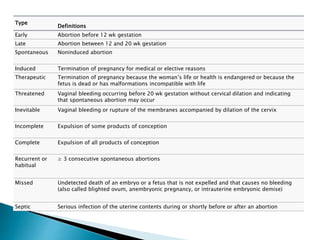
- 1. Type Definitions Early Abortion before 12 wk gestation Late Abortion between 12 and 20 wk gestation Spontaneous Noninduced abortion Induced Termination of pregnancy for medical or elective reasons Therapeutic Termination of pregnancy because the womanŌĆÖs life or health is endangered or because the fetus is dead or has malformations incompatible with life Threatened Vaginal bleeding occurring before 20 wk gestation without cervical dilation and indicating that spontaneous abortion may occur Inevitable Vaginal bleeding or rupture of the membranes accompanied by dilation of the cervix Incomplete Expulsion of some products of conception Complete Expulsion of all products of conception Recurrent or habitual Ōēź 3 consecutive spontaneous abortions Missed Undetected death of an embryo or a fetus that is not expelled and that causes no bleeding (also called blighted ovum, anembryonic pregnancy, or intrauterine embryonic demise) Septic Serious infection of the uterine contents during or shortly before or after an abortion
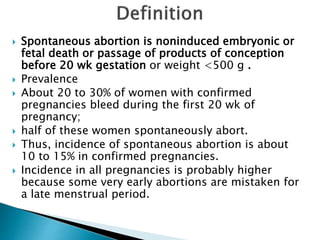
- 3. ’üĮ Spontaneous abortion is noninduced embryonic or fetal death or passage of products of conception before 20 wk gestation or weight <500 g . ’üĮ Prevalence ’üĮ About 20 to 30% of women with confirmed pregnancies bleed during the first 20 wk of pregnancy; ’üĮ half of these women spontaneously abort. ’üĮ Thus, incidence of spontaneous abortion is about 10 to 15% in confirmed pregnancies. ’üĮ Incidence in all pregnancies is probably higher because some very early abortions are mistaken for a late menstrual period.
- 4. ’üĮ Host factors ŌĆö Pregnancy loss may also be related to the host environment. As an example, congenital or acquired uterine abnormalities (eg, uterine septum, submucosal leiomyoma, intrauterine adhesions) can interfere with optimal implantation and growth. ’üĮ Acute maternal infection -eg, Listeria monocytogenes, Toxoplasma gondii, parvovirus B19, rubella, herpes simplex, cytomegalovirus, lymphocytic choriomeningitis virus can lead to abortion from fetal or placental infection. ’üĮ Chromosomal abnormalities, ’üĮ Maternal endocrinopathies (eg, thyroid dysfunction, Cushing's syndrome, polycystic ovary syndrome) can also contribute to a suboptimal host environment. Since corpus luteum progesterone production is an integral component of successful pregnancy, it is plausible that early pregnancy loss could be due to corpus luteum dysfunction; The effect of thyroid disease and thyroid peroxidase antibodies on abortion risk is also. ’üĮ A hypercoagulable state due to inherited or acquired thrombophilia and abnormalities of the immune system (eg, systemic lupus erythematosus, antiphospholipid syndrome) that lead to immunological rejection or placental damage are active areas of investigation. ’üĮ Other causes include immunologic abnormalities, major trauma-Invasive intrauterine procedures/trauma, such as chorionic villus sampling and amniocentesis, increase the risk of abortion, and uterine abnormalities (eg, fibroids, adhesions). ’üĮ Most often, the cause is unknown Unexplained 50%
- 5. ’üĮ Age > 35 ’üĮ History of spontaneous abortion ’üĮ Cigarette smoking ’üĮ Use of certain drugs (eg, cocaine, alcohol, high doses of caffeine) ’üĮ Fevers of 100┬░F (37.8┬░C) or more may increase the risk of miscarriage, but the only two large studies have been contradictory and inconclusive. ’üĮ Low-folate level ŌĆö were associated with an increased risk of SAb at 6 to 12 weeks of gestation, but only when the fetal karyotype was abnormal. ’üĮ A poorly controlled chronic disorder (eg, diabetes, hypertension, overt thyroid disorders) in the mother Subclinical thyroid disorders, a retroverted uterus, and minor trauma have not been shown to cause spontaneous abortions. Maternal weight ŌĆö Prepregnancy body mass index less than 18.5 or above 25 kg/m2 has been associated with an increased risk of infertility and SAB
- 6. ’üĮ Crampy pelvic pain, ’üĮ bleeding, and eventually expulsion of tissue. Late spontaneous abortion may begin with a gush of fluid when the membranes rupture. Hemorrhage is rarely massive. A dilated cervix indicates that abortion is inevitable. ’üĮ If products of conception remain in the uterus after spontaneous abortion, vaginal bleeding may occur, sometimes after a delay of hours to days. ’üĮ Infection may also develop, causing fever, pain, and sometimes sepsis.
- 7. ’üĮ Clinical criteria-Women who are actively in the process of having a spontaneous abortion usually present with a history of amenorrhea, vaginal bleeding, and pelvic pain. ’üĮ Usually ultrasonography and quantitative ╬▓ subunit of human chorionic gonadotropin (╬▓-hCG) ’üĮ Diagnosis of threatened, inevitable, incomplete, or complete abortion is often possible based on clinical criteria (see Table: Characteristic Symptoms and Signs in Spontaneous Abortions) and a positive urine pregnancy test. However, ultrasonography and quantitative measurement of serum ╬▓-hCG are usually done to exclude ectopic pregnancy and to determine whether products of conception remain in the uterus (suggesting that abortion is incomplete rather than complete). However, results may be inconclusive, particularly during early pregnancy. ’üĮ
- 8. ’üĮ Definition. Uterine bleeding before 20 weeks with a closed cervical os and a confirmed viable intrauterine gestation. ’üĮ Vaginal spotting or heavier bleeding occurs in 20ŌĆō25% of pregnant women and may persist for days or weeks. However, some bleeding near the time of expected menses may be physiologic. ’üĮ Half of these pregnancies will eventually miscarry, but the risk is substantially lower if fetal cardiac activity is demonstrated. Fetuses that do not miscarry remain at increased risk for preterm delivery, low birthweight, and perinatal death. ’üĮ Treatment. There are no effective therapies and patients are monitored expectantly unless the pregnancy is undesired or non-viable. Bed rest is often recommended, but does not alter the course.
- 9. ’üĮ Definition. Imminent, partial, or complete expulsion of products of conception before 20 weeksŌĆÖ gestation through a dilated cervix. ’üĮ When the placenta, in whole or in part, detaches from the uterus, bleeding ensues. Typically bleeding is profuse and associated with uterine cramping. During incomplete miscarriage, the internal os remains open and allows passage of blood. Following complete detachment and expulsion of the gestational products, the internal cervical os closes. ’üĮ Incomplete miscarriages usually occur between 6 and 14 weeksŌĆÖ gestation; complete miscarriages are most common <6 or >14 weeks. ’üĮ Treatment. Suction curettage is typically required for inevitable or incomplete miscarriage; complete miscarriages may be managed expectantly without evacuation. ’üĮ
- 10. ’üĮ Definition. Any threatened, inevitable, or incomplete miscarriage associated with a fever before 20 weeksŌĆÖ gestation. ’üĮ Retained products of conception after spontaneous miscarriage, legal termination of pregnancy, or illegal termination of pregnancy acts as a nidus for the development of a local infection that is poten- tially fatal if generalized sepsis ensues. ’üĮ Patients usually present with fever, chills, leukocytosis, uterine ten- derness, and a foul-smelling cervicovaginal discharge. ’üĮ Treatment. Broad-spectrum intravenous antibiotics, prompt uterine evacuation, and supportive therapy in severe cases. However, a large, grossly infected uterus is at risk for perforation and may be allowed to evacuate with pitocin or prostaglandin stimulation.
- 11. ’üĮ Missed abortion is suspected if the uterus does not progressively enlarge or if quantitative ╬▓- hCG is low for gestational age or does not double within 48 to 72 h. Missed abortion is confirmed if ultrasonography shows any of the following: ’üĮ Disappearance of previously detected embryonic cardiac activity ’üĮ Absence of such activity when the fetal crown- rump length is > 5 mm (determined by transvaginal ultrasonography) ’üĮ Absence of a fetal pole (determined by transvaginal ultrasonography) when the mean sac diameter (average of diameters measured in 3 orthogonal planes) is > 18 mm
- 12. ’üĮ Definition. Fetal demise before 20 weeksŌĆÖ gestation without detach- ment of the placenta ŌĆō resulting in retention of products of conception for days or weeks behind a closed cervical os. ’üĮ Typically, after the demise there is an episode of bleeding that sub- sides and is followed by a continuous brown vaginal discharge. Many women have no other symptoms. Very rarely, prolonged retention of a dead fetus after midpregnancy can result in coagulopathy. ’üĮ Treatment. Management is individualized, depending on the cir- cumstances. Expectant management is often difficult for the patient to endure after being informed of the demise. Medical management is often the safest option.
- 13. ’üĮ Ultrasonography is the most useful test in the diagnostic evaluation of women with suspected Sab. ’üĮ There is no role for monitoring hCG levels once the presence of an intrauterine pregnancy has been established sonographically. ’üĮ A definite diagnosis of nonviable intrauterine pregnancy (missed abortion) can be made based upon either of the following criteria: ’üĮ Absence of embryonic cardiac activity in an embryo with crown-rump length greater than 5 mm. ’üĮ Absence of a yolk sac when the mean sac diameter is 13 mm. ’üĮ Absence of an embryonic pole when the mean sac diameter (average of diameters measured in each of three orthogonal planes) is greater than 25 mm measured transabdominally or greater than 18 mm by the transvaginal technique. ’üĮ These measurements correspond to a gestational age of approximately 6 weeks. Serial examinations four to seven days apart are helpful to assess viability of the pregnancy when findings are equivocal or development appears to be lagging behind that expected by dating criteria. The normal sequential development during very early pregnancy, as noted sonographically, is shown in the table A gestational sac size of 2 to 3 mm may be visualized at four weeks and one to three days The yolk sac can be noted initially at the beginning of the fifth week of gestation An embryonic pole with cardiac activity can be first detected at 5.5 to 6 weeks
- 14. ’üĮ Abnormal yolk sac - An abnormal yolk sac may be large for gestational age, irregular, free floating in the gestational sac rather than at the periphery, or calcified. ’üĮ Slow fetal heart rate - Embryonic heart rate below 100 beats per minute (bpm) at 5 to 7 weeks of gestation is slow. If slow cardiac activity is observed, it is prudent to perform a follow-up sonogram (in five to seven days) to document loss of the cardiac activity before proceeding to dilatation and curettage. ’üĮ Small sac - Small mean sac size (MSS) is diagnosed when the difference between the MSS and crown-rump length (CRL) is less than 5 mm (MSS - CRL < 5). Poor pregnancy outcome - a sac with an irregular contour, mean sac diameter growth rate less than 1 mm/day, minimal decidual thickness/hypoechogenicity of the choriodecidual area/absent double decidual sac, and low sac position in the uterus. ’üĮ Subchorionic hematoma ŌĆō A subchorionic hematoma is a risk factor for SAb. A large subchorionic hematoma (ie, comprising at least 25 percent of the volume of the gestational sac) is concerning. There was also an increased risk of placental abruption and preterm premature rupture of membranes. Increased risks of preterm labor and stillbirth appeared to be dependent upon the presence of vaginal bleeding. ’üĮ Pregnancy outcome associated with subchorionic hematoma appears to depend upon location, with worse outcomes for retroplacental than marginal hematomas. Women with retroplacental hematomas are more likely to have an adverse outcome than those that are marginal (only the margin of the placenta is separated). Data are mixed regarding whether increasing size of the hematoma increases the risk of adverse outcomes.
- 15. Transabdominal sagittal sonogram of uterus reveals subchorionic hematoma (H) extending posteriorly around chorion (arrows) and lifting edge of anterior placenta (P). Appearance should not be confused with that of unfused amnion. Amnion is the thin membrane continuous along anterior placental edge, but limited by umbilical cord insertion; subchorionic bleeding leads to edge of placenta.
- 16. ’üĮ Termination of pregnancy
- 17. ’üĮ Definition. Elective or voluntary ŌĆ£abortionŌĆØ is the interruption of pregnancy before viability at the request of the woman. ’üĮ About 1.2 million terminations are performed annually in the USA. Half the women are younger than 25 years. About 88% are conducted up to 12 weeks, 10% from 13 weeks to 20 weeks, and 1ŌĆō2% beyond 20 weeks. ’üĮ Half the abortions worldwide are considered unsafe. Unsafe abor- tion accounts for an estimated 13% of all maternal deaths.
- 18. ’üĮ The Abortion Pill: Medical Abortion with Mifepristone and Misoprostol
- 19. ’üĮ Medical Abortion is a form of early abortion caused by the combination of two medications, mifepristone and misoprostol that is an option for women who are 8-9 weeks pregnant or less. Also known as RU486 or medication abortion. ’üĮ During the first appointment at the clinic patient receive the mifepristone pill - RU486 orally. A progesterone receptor antagonist that blocks the hormone needed to maintain the pregnancy. ’üĮ Then 24 to 72 hours later patient at home takes the second medication, ’üĮ Misoprostol (Cytotec, USA) IS prostaglandin E1 analogs. Misoprostol causes contractions resulting in a miscarriage. ’üĮ Mifepristone and misoprostol are FDA approved.
- 20. ’üĮ Mifepristone blocks the hormone progesterone needed to maintain the pregnancy. Because this hormone is blocked, the uterine lining begins to shed, the cervix begins to soften and bleeding may occur. With the later addition of the misoprostol, the uterus contracts and the pregnancy is usually expelled within 6 to 8 hours. ’üĮ Because the woman chooses when she takes the second medication within the time frame of 24 to 72 hours after the first medication, she has some control over the timing of when she expels the pregnancy and experiences the side effects of bleeding and cramping.
- 21. ’üĮ A follow-up exam is scheduled for two weeks later to make sure the process is complete. ’üĮ If women have not yet miscarried, doctor perform a aspiration abortion. ’üĮ A very small percentage (5%) of women do not pass the pregnancy tissue and need a suction procedure to complete the process.
- 22. Side Effects Most of the side effects when using this early abortion option are caused by the second medication, misoprostol. Side-effects may include: heavy bleeding, headache, nausea, vomiting, diarrhea, and heavy cramping. Risks Vaginal bleeding with medical abortion could be extremely heavy. In rare situations it could require a aspiration abortion and very rarely, a blood transfusion. If pregnancy is continued after taking these medications, there is a high risk of fetal deformities.
- 23. ’üĮ These are 99% effective. ’üĮ About 90% of all terminations in the USA and the UK. ’üĮ The cervix is first dilated, then the uterine cavity is mechanically evacuated. ’üĮ Surgical termination is a simple procedure and is safer than childbirth when performed before week 16. ’üĮ Manual vacuum aspiration (MVA) can be performed up to 6ŌĆō7 weeksŌĆÖ gestation without regional anesthesia. A soft, flexible, plastic cannula is attached to a handheld self- locking syringe. Evacuation is accomplished by repetitive in-and-out, rotating movements. ’üĮ Electric vacuum aspiration (EVA) uses an electric pump, requires a paracervical block and cervical dilation, and is used for terminations between 6 and 15 weeksŌĆÖ gestation.
- 24. ’üĮ The frequency of complications depends on operator experience and gestational age (increased if <6 weeks or >16 weeks). ’üĮ Immediate complications. Hemorrhage, cervical injury, anesthesia complications. The use of osmotic dilators (laminaria) significantly reduces the risk of uterine perforation. ’üĮ Late complications. Retained products of conception, infection (endometritis), and Rh sensitization. ’üĮ Mortality rate. Fewer than 1/100,000 surgical procedures when a patient is under the care of an experienced clinician. ’üĮ
- 25. ’üĮ Dilation and evacuation (D&E) is performed between 15 and 20 weeksŌĆÖ gestation. ’üĮ Due to the larger fetal size, the procedure is often done in the operating room under general anesthesia. ’üĮ Cervical preparation and dilation precedes mechanical destruction and evacuation of fetal parts using specialized (Sopher) forceps. The placenta and remaining tissue are then removed by suction curettage. ’üĮ Regardless of technique, identification of products of conception is mandatory before the procedure is considered complete.































![maternal guide presentation [Autosaved].pptx](https://cdn.slidesharecdn.com/ss_thumbnails/maternalpresentationautosaved-250208125838-a01bbc1b-thumbnail.jpg?width=560&fit=bounds)






































