Splints
- 1. Orthopedic Injuries and Immobilization Stanford University Division of Emergency Medicine
- 2. History and Physical Exam ŌĆó Immediately upon presentation with a dislocation or fracture, the neurovascular and circulatory status must be checked. ŌĆó Attempt to ascertain the mechanism of injury. - may alert physician to other possibly associated injuries - as well as provide clues as to the type of injury involved ŌĆó Radiographs should be obtained if fracture OR DISLOCATION is suspected ŌĆó Radiographs should be obtained after reduction and IMMOBILIZATION of a fracture or dislocation.
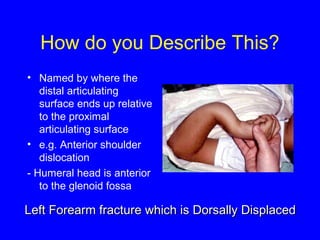
- 3. How do you Describe This? ŌĆó Named by where the distal articulating surface ends up relative to the proximal articulating surface ŌĆó e.g. Anterior shoulder dislocation - Humeral head is anterior to the glenoid fossa Left Forearm fracture wwhhiicchh iiss DDoorrssaallllyy DDiissppllaacceedd
- 4. REDUCING DISLOCATIONS and SUBLUXATIONS ŌĆó Three keys to success when attempting reduction a. knowledge of anatomy b. analgesia and sedation c. slow and gentle procedure ŌĆó Following reduction, the joint must be splinted and proper follow-up is mandatory ŌĆó After one or two unsuccessful attempts of reducing a dislocation (closed reduction), it is necessary to reduce under general anesthesia (closed) or during surgery (open reduction)
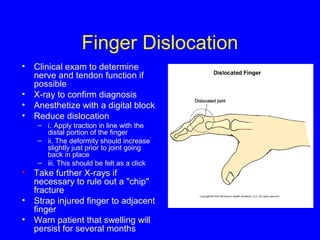
- 5. Finger Dislocation ŌĆó Clinical exam to determine nerve and tendon function if possible ŌĆó X-ray to confirm diagnosis ŌĆó Anesthetize with a digital block ŌĆó Reduce dislocation ŌĆō i. Apply traction in line with the distal portion of the finger ŌĆō ii. The deformity should increase slightly just prior to joint going back in place ŌĆō iii. This should be felt as a click ŌĆó Take further X-rays if necessary to rule out a "chip" fracture ŌĆó Strap injured finger to adjacent finger ŌĆó Warn patient that swelling will persist for several months
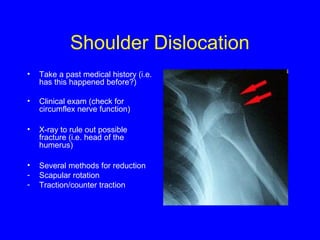
- 6. Shoulder Dislocation ŌĆó Take a past medical history (i.e. has this happened before?) ŌĆó Clinical exam (check for circumflex nerve function) ŌĆó X-ray to rule out possible fracture (i.e. head of the humerus) ŌĆó Several methods for reduction - Scapular rotation - Traction/counter traction
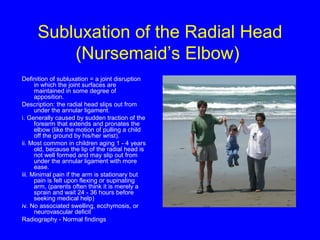
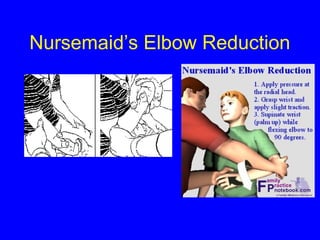
- 7. Subluxation of the Radial Head (NursemaidŌĆÖs Elbow) Definition of subluxation = a joint disruption in which the joint surfaces are maintained in some degree of apposition. Description: the radial head slips out from under the annular ligament. i. Generally caused by sudden traction of the forearm that extends and pronates the elbow (like the motion of pulling a child off the ground by his/her wrist). ii. Most common in children aging 1 - 4 years old, because the lip of the radial head is not well formed and may slip out from under the annular ligament with more ease. iii. Minimal pain if the arm is stationary but pain is felt upon flexing or supinating arm, (parents often think it is merely a sprain and wait 24 - 36 hours before seeking medical help) iv. No associated swelling, ecchymosis, or neurovascular deficit Radiography - Normal findings
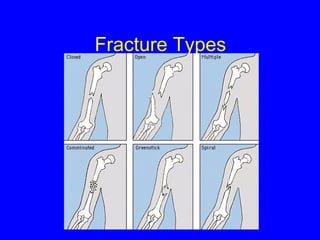
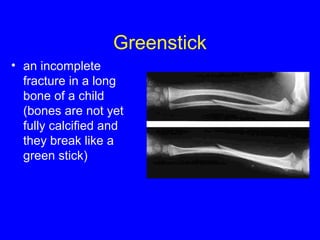
- 10. Greenstick ŌĆó an incomplete fracture in a long bone of a child (bones are not yet fully calcified and they break like a green stick)
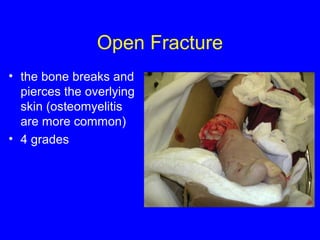
- 11. Open Fracture ŌĆó the bone breaks and pierces the overlying skin (osteomyelitis are more common) ŌĆó 4 grades
- 12. Spiral Fracture ŌĆó a fracture that spirals part of the length of a long bone
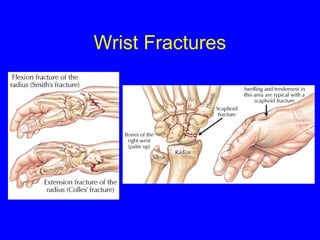
- 13. Wrist Fractures
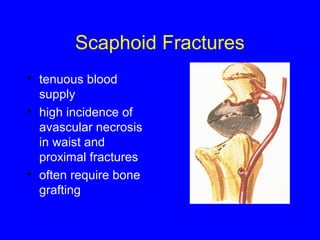
- 14. Scaphoid Fractures ŌĆó tenuous blood supply ŌĆó high incidence of avascular necrosis in waist and proximal fractures ŌĆó often require bone grafting
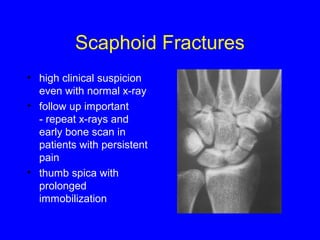
- 15. Scaphoid Fractures ŌĆó high clinical suspicion even with normal x-ray ŌĆó follow up important - repeat x-rays and early bone scan in patients with persistent pain ŌĆó thumb spica with prolonged immobilization
- 16. Hey Kids, As Seen On TV!! Learn How to Splint in 10 Easy Lessons!!!! Amaze Your Friends !!! WOW !!! Be the First on your Block !!!
- 17. Introduction ŌĆó Evidence of rudimentary splints found as early as 500 BC. ŌĆó Used to temporarily immobilize fractures, dislocations, and soft tissue injuries. ŌĆó Circumferential casts abandoned in the ED - increased compartment syndrome and other complications - ideal for the ED ŌĆō allow swelling - splints easier to apply
- 18. Indications for Splinting ŌĆó Fractures ŌĆó Sprains ŌĆó Joint infections ŌĆó Tenosynovitis ŌĆó Acute arthritis / gout ŌĆó Lacerations over joints ŌĆó Puncture wounds and animal bites of the hands or feet
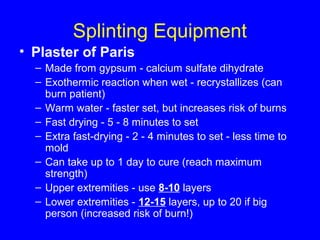
- 19. Splinting Equipment ŌĆó Plaster of Paris ŌĆō Made from gypsum - calcium sulfate dihydrate ŌĆō Exothermic reaction when wet - recrystallizes (can burn patient) ŌĆō Warm water - faster set, but increases risk of burns ŌĆō Fast drying - 5 - 8 minutes to set ŌĆō Extra fast-drying - 2 - 4 minutes to set - less time to mold ŌĆō Can take up to 1 day to cure (reach maximum strength) ŌĆō Upper extremities - use 8-10 layers ŌĆō Lower extremities - 12-15 layers, up to 20 if big person (increased risk of burn!)
- 20. Splinting Equipment ŌĆó Ready Made Splinting Material ŌĆō Plaster (OCL) ŌĆó 10 -20 sheets of plaster with padding and cloth cover ŌĆō Fiberglass (Orthoglass) ŌĆó Cure rapidly (20 minutes) ŌĆó Less messy ŌĆó Stronger, lighter, wicks moisture better ŌĆó Less moldable
- 21. Splinting Equipment ŌĆó Stockinette ŌĆó protects skin, looks nifty (often not necessary) ŌĆó cut longer than splint ŌĆó 2,3,4,8,10,12-in. widths ŌĆó Padding - Webril ŌĆó 2-3 layers, more if anticipate lots of swelling ŌĆó Extra over elbows, heels ŌĆó Be generous over bony prominences ŌĆó Always pad between digits when splinting hands/feet or when buddy taping ŌĆó Avoid wrinkles ŌĆó Do not tighten - ischemia! ŌĆó Avoid circumfrential use ŌĆó Ace wraps
- 22. Specific Splints and Orthoses Upper Extremity ŌĆó Elbow/Forearm ŌĆō Long Arm Posterior ŌĆō Double Sugar - Tong ŌĆó Forearm/Wrist ŌĆō Volar Forearm / Cockup ŌĆō Sugar - Tong ŌĆó Hand/Fingers ŌĆō Ulnar Gutter ŌĆō Radial Gutter ŌĆō Thumb Spica ŌĆō Finger Splints Lower Extremity ŌĆó Knee ŌĆō Knee Immobilizer / Bledsoe ŌĆō Bulky Jones ŌĆō Posterior Knee Splint ŌĆó Ankle ŌĆō Posterior Ankle ŌĆō Stirrup ŌĆó Foot ŌĆō Hard Shoe
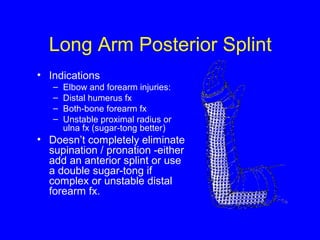
- 23. Long Arm Posterior Splint ŌĆó Indications ŌĆō Elbow and forearm injuries: ŌĆō Distal humerus fx ŌĆō Both-bone forearm fx ŌĆō Unstable proximal radius or ulna fx (sugar-tong better) ŌĆó DoesnŌĆÖt completely eliminate supination / pronation -either add an anterior splint or use a double sugar-tong if complex or unstable distal forearm fx.
- 24. Double Sugar Tong ŌĆó Indications ŌĆō Elbow and forearm fx - prox/mid/distal radius and ulnar fx. ŌĆō Better for most distal forearm and elbow fx because limits flex/extension and pronation / supination. 10 90
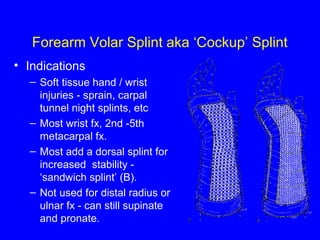
- 25. Forearm Volar Splint aka ŌĆśCockupŌĆÖ Splint ŌĆó Indications ŌĆō Soft tissue hand / wrist injuries - sprain, carpal tunnel night splints, etc ŌĆō Most wrist fx, 2nd -5th metacarpal fx. ŌĆō Most add a dorsal splint for increased stability - ŌĆśsandwich splintŌĆÖ (B). ŌĆō Not used for distal radius or ulnar fx - can still supinate and pronate.
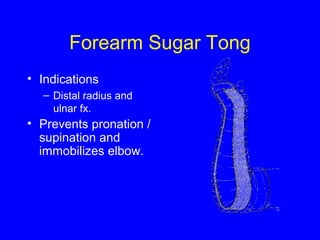
- 26. Forearm Sugar Tong ŌĆó Indications ŌĆō Distal radius and ulnar fx. ŌĆó Prevents pronation / supination and immobilizes elbow.
- 27. Hand Splinting ŌĆó The correct position for most hand splints is the position of function, a.k.a. the neutral position. ŌĆó This is with the the hand in the ŌĆ£beer canŌĆØ position (which may have contributed to the injury in the first place) : wrist slightly extended (10-25┬░) with fingers flexed as shown. ŌĆó When immobilizing metacarpal neck fractures, the MCP joint should be flexed to 90┬░. ŌĆó Have the patient hold an ace wrap (or a beer can if available) until the splint hardens. ŌĆó For thumb fx, immobilize the thumb as if holding a wine glass.
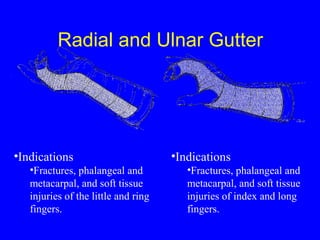
- 28. Radial and Ulnar Gutter ŌĆóIndications ŌĆóFractures, phalangeal and metacarpal, and soft tissue injuries of the little and ring fingers. ŌĆóIndications ŌĆóFractures, phalangeal and metacarpal, and soft tissue injuries of index and long fingers.
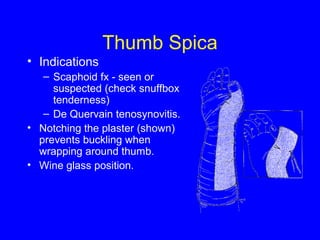
- 29. Thumb Spica ŌĆó Indications ŌĆō Scaphoid fx - seen or suspected (check snuffbox tenderness) ŌĆō De Quervain tenosynovitis. ŌĆó Notching the plaster (shown) prevents buckling when wrapping around thumb. ŌĆó Wine glass position.
- 30. Finger Splints ŌĆó Sprains - dynamic splinting (buddy taping). ŌĆó Dorsal/Volar finger splints - phalangeal fx, though gutter splints probably better for proximal fxs.
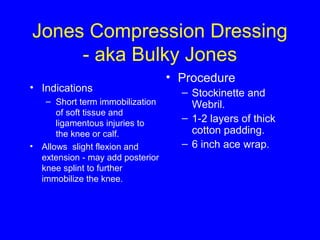
- 31. Jones Compression Dressing - aka Bulky Jones ŌĆó Indications ŌĆō Short term immobilization of soft tissue and ligamentous injuries to the knee or calf. ŌĆó Allows slight flexion and extension - may add posterior knee splint to further immobilize the knee. ŌĆó Procedure ŌĆō Stockinette and Webril. ŌĆō 1-2 layers of thick cotton padding. ŌĆō 6 inch ace wrap.
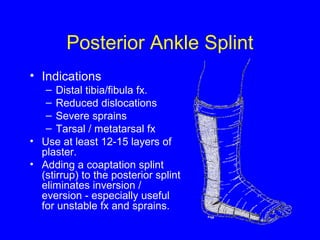
- 32. Posterior Ankle Splint ŌĆó Indications ŌĆō Distal tibia/fibula fx. ŌĆō Reduced dislocations ŌĆō Severe sprains ŌĆō Tarsal / metatarsal fx ŌĆó Use at least 12-15 layers of plaster. ŌĆó Adding a coaptation splint (stirrup) to the posterior splint eliminates inversion / eversion - especially useful for unstable fx and sprains.
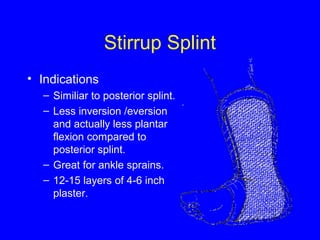
- 33. Stirrup Splint ŌĆó Indications ŌĆō Similiar to posterior splint. ŌĆō Less inversion /eversion and actually less plantar flexion compared to posterior splint. ŌĆō Great for ankle sprains. ŌĆō 12-15 layers of 4-6 inch plaster.
- 34. Other Orthoses ŌĆó Knee Immobilizer ŌĆō Semirigid brace, many models ŌĆō Fastens with Velcro ŌĆō Worn over clothing ŌĆó Bledsoe Brace ŌĆō Articulated knee brace ŌĆō Amount of allowed flexion and extension can be adjusted ŌĆō Used for ligamentous knee injuries and post-op ŌĆó AirCast/ Airsplint ŌĆō Resembles a stirrup splint with air bladders ŌĆō Worn inside shoe ŌĆó Hard Shoe ŌĆō Used for foot fractures or soft tissue injuries
- 35. Complications ŌĆó Burns ŌĆō Thermal injury as plaster dries ŌĆō Hot water, Increased number of layers, extra fast-drying, poor padding - all increase risk ŌĆō If significant pain - remove splint to cool ŌĆó Ischemia ŌĆō Reduced risk compared to casting but still a possibility ŌĆō Do not apply Webril and ace wraps tightly ŌĆō Instruct to ice and elevate extremity ŌĆō Close follow up if high risk for swelling, ischemia. ŌĆō When in doubt, cut it off and look ŌĆō Remember - pulses lost late. ŌĆó Pressure sores ŌĆō Smooth Webril and plaster well ŌĆó Infection ŌĆō Clean, debride and dress all wounds before splint application ŌĆō Recheck if significant wound or increasing pain Any complaints of worsening pain - Take the splint off and look!
- 36. Questions?