srp head and neck space infections UG.pptx
- 1. HEAD AND NECK SPACE INFECTIONS Dr. Shirish Patil Head neck & Skull base surgeon BIMS , Bgm
- 2. ŌĆó Spaces ŌĆó Risk factors ŌĆó Etiology ŌĆó Anatomy, clinical features & approach ŌĆó Investigations ŌĆó treatment
- 3. SPACES IN THE FACE MAXILLARY 1. Canine 2. Buccal Others 1. Parotid space ŌĆó MANDIBULAR Primary 1. Submental 2. Sub mandibular 3. Sub lingual Secondary/ Masticator 1. Pterygomandibular 2. Massetric 3. Temporal
- 4. Spaces of the neck ŌĆó Entire length of neck Deep neck spaces a. Retropharyngeal b. Danger c. Prevertebral d. Carotid ŌĆó Suprahyoid a. Submandibular b. Submental c. Sublingual d. Parapharyngeal e. Peritonsillar ŌĆó Infrahyoid Pretracheal space
- 5. RISK FACTORS ŌĆó Immunocompromised conditions ŌĆó Long term steroid intake ŌĆó Hepatitis ŌĆó Diabetes mellitus ŌĆó Malignancies ŌĆó Chemotherapy ŌĆó Collagen vascular diseases
- 6. ETIOLOGY OF DEEP NECK SPACE INFECTIONS ŌĆó Odontogenic ( MC ) ŌĆó Oropharngeal infections: tonsillits, pharyngitis Acute sinusitis in children ŌĆó Sialadenitis ŌĆō with or without obstruction ŌĆó Impacted upper aerodigestive tract FB ŌĆó Trauma ŌĆō iatrogenic / accidental ŌĆó Needle injection in IV drug users ( neck) ŌĆó Necrotic malignant LN ŌĆó Acute mastoiditis with Bezolds abscess ŌĆó Infected congenital lesions viz branchial clefts cysts, thyroglossal cysts The initiating site of infection is not known in 50% of DNSI ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”..Parischar . Deep neck abscesses: a retrospective review of 215 cases. Ann Oto Lary 110: 1025-1030, 1991
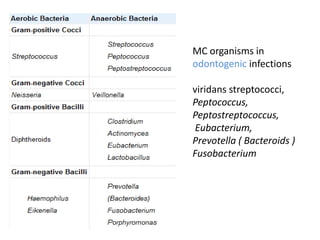
- 7. ORGANISMS IN DNSI ŌĆó Streptococcus viridans, ŌĆó Staphylococcus epidermidis, ŌĆó Staphylococcus aureus, ŌĆó group A beta-hemolytic Streptococcus (Streptococcus pyogenes), ŌĆó Bacteroides, ŌĆó Fusobacterium, and ŌĆó Peptostreptococcus species. NORMAL FLORA OF THE OROPHAARYNX
- 8. MC organisms in odontogenic infections viridans streptococci, Peptococcus, Peptostreptococcus, Eubacterium, Prevotella ( Bacteroids ) Fusobacterium
- 9. Microbiology ŌĆó The microbiology of deep neck space infections most often yields a mixture of aerobic and anaerobic organisms, usually representative of the oropharyngeal flora ŌĆó Methicillin-resistant Staphylococcus aureus (MRSA)-associated neck space infections is significantly increasing
- 10. Mech of anaerobic infection aerobic or facultative streptococci release exotoxins and lytic enzymes spreading cellulitis infection progresses, a mixed streptococcal/anaerobic infection hypoxic state increases, the predominance of anaerobic bacteria becomes evident
- 11. Routes of spread ŌĆó Lymphatic ŌĆó Arterial / venous ŌĆó Direct extensions
- 12. Example of venous spread Para nasal Sinus Facial planes Upper dentition Ophthalmic Vn Facial Vn Orbital cellulitis ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”..Cummings ORL & HNS
- 13. Spread of odontogenic infections Vestibule Palate Maxillary sinus Buccal space Sublingual space Submandibular space
- 14. BUCCAL SPACE ŌĆó Between buccinator muscle & skin ŌĆó C/F Cheek swelling ŌĆó Drained ŌĆó intra orally- Inadequate ŌĆó Extra orally - scar
- 15. CANINE SPACE ŌĆó Between the anterior surface of maxilla and the levator labii superioris ŌĆó Swelling lateral to the nose ŌĆó Obliteration of nasolabial fold - HALLMARK ŌĆó Intra oral stab incision
- 16. DIVISION OF SUB MANDIBULAR SPACE Sub lingual ŌĆō 1st molar They communicate posteriorly Odontogenic cause is MC etiology Sub- mandibular- 2nd / 3rd molar
- 17. Swelling of the floor of mouth Dysphagia Elevated tongue Swelling over the submandibular region of the neck SUB LINGUAL SPACE SUB MANDIBULAR SPACE
- 19. SUBMANDIBULAR AND SUBLINGUAL SPACE ŌĆó Horizontal incision along the inferior border of mandible 0.5 to 5 cm long
- 20. SUBMENTAL SPACE Laterally : Anterior bellies of digastric Post : mylohyoid Ant : skin & superficial fascia
- 22. MASTICATOR SPACE/ SECONDARY MANDIBULAR SPACES Deep cervical fascia splits between the Zygomatic arch and the inferior border of mandible Contents: Mandible Muscles of mastication 3rd part of maxillary artery Trigeminal nerve Divisions: Massetric Pterygoid Temporal
- 23. MASTICATOR SPACE ŌĆó MC cause ŌĆō odontogenic ŌĆō 3rd molars from the sub mandibular ŌĆó Trismus is a hall mark of involvement of masticator space
- 24. ŌĆó Temporal ŌĆó Pterygoid & ŌĆó Massetric
- 25. PAROTID SPACE Deep cervical fascia splits between the Zygomatic arch and the inferior border of mandible Parotid gland Facial nerve Ext. carotid artery Post facial Vein
- 27. LUDWIGS ANGINA Wilhelm Fredrich von Ludwig first described it in 1836
- 28. PSEUDO LUDWIGS ŌĆó Suppurative lymphadenitis in scarlet fever, measles and diptheria.
- 29. severe trismus, drooling, inability to swallow, tachypnea, and dyspnea Edema in the floor of mouth Fluctuation is not appreciated Strangulation - ANGINA COD ŌĆō Airway compromise
- 30. INCISION AND DRAINAGE Horizontal incision 2 and ┬Į finger breadthŌĆÖs below the lower margin of mandible and can be extended further Mylohyoid is split Gross app : - ŌĆ£ salt pork ŌĆ£ appearance, woody induration, watery fluid and little bleeding
- 31. PARAPHARYNGEAL SPACE ŌĆō MedialŌĆötonsillar fossa, pterygomandibular ligament ŌĆō LateralŌĆömedial pterygoid, acsending ramus, ŌĆō Sup- skull base ŌĆō Inf- Hyoid ŌĆō Post- prevertebral fascia ŌĆó Poststyloid ŌĆō Carotid sheath- CA & IJV ŌĆō Cranial nerves IX, X, XI, XII ŌĆō Sympathetic chain
- 32. Parapharyngeal Space ŌĆó Communicates with several deep neck spaces. ŌĆō Parotid ŌĆō Masticator ŌĆō Peritonsillar ŌĆō Submandibular ŌĆō Retropharyngeal
- 33. PARAPHARYNGEAL SPACE ŌĆó Horizontal skin incision 2 1/2 finger breadth below the inferior margin of mandible, at the level of carotid bifurcation ŌĆó Dissect between the sub mandibular gland & SCM, medial to the mandible
- 34. RETROPHARYNGEAL SPACE ŌĆó Boundaries: ŌĆō Upper: skull base ŌĆō Lower: mediastinum at the tracheal bifurcation ŌĆō Anterior: buccopharynge al fascia, lining of the posterior pharynx and esophagus ŌĆō Posterior: alar fascia
- 36. ŌĆó Content: lymph node of Rouvier ŌĆó Routes of entry: 1. direct spread from the parapharyngeal space, 2. 2. lymphatic spread from the paranasal sinuses nasopharyngeal region ’āĀ suppuration of Lymph nodes 3. From prevertebral space
- 37. ADULTS CHIDREN < 5 years Onset Chronic Acute Etiology PottŌĆÖs spine Suppuration of LN of Rouvier URTI ACUTE SINUSITIS C/F Dysphagia Meningismus- de to irritation of paraspinal muscles
- 38. X ray STN Lateral C2 - > 7mm / > 1/3 the width of body of C2 C6 Children ( <15 yrs) > 14 mm Adults > 22mm
- 40. RETROPHARYNGEAL SPACE ŌĆó Small : intra oral drainage : Trendelenburg position ŌĆó Large: Transcutaneous : Vertical skin incision along anterior border of SCM : retract great vessels & SCM posteriorly
- 41. DANGER SPACE ŌĆó Potential Space, dangerous for rapid inferior spread of infection to the posterior mediastinum through its loose areolar tissue ŌĆó Boundaries ŌĆō Superior: skull base ŌĆō Inferior: diaphragm ŌĆō Anterior: alar fascia, retropharyngeal space ŌĆō Posterior: prevertebral fascia ŌĆō Lateral: transverse processes of vertebrae ŌĆó Contains: sympathetic trunk ŌĆó Routes of entry: retropharyngeal, parapharyngeal, or prevertebral spaces
- 43. DANGER SPACE
- 44. PREVERTEBRAL SPACE ŌĆó Potential space ŌĆó Boundaries ŌĆō Superior: clivus of the skull base ŌĆō Inferior: coccyx ŌĆō Anterior: prevertebral fascia ŌĆō Posterior: vertebral bodies ŌĆō Lateral: transverse processes ŌĆó Contains: paraspinous, prevertebral, and scalene muscles, vertebral artery and vein, brachial plexus, and phrenic nerve ŌĆó Routes of entry: infection of the vertebral bodies and penetrating injuries
- 46. PERI TONSILLAR SPACE ŌĆó MedialŌĆöcapsule of palatine tonsil ŌĆó LateralŌĆösuperior pharyngeal constrictor ŌĆó AntŌĆöanterior tonsil pillar ŌĆó PostŌĆöposterior tonsil pillar
- 47. ŌĆó C/f ŌĆō trismus, dysphagia, Hot potato Voice, Otalgia, deviated uvula ŌĆó George Washington died of Quinsy
- 48. CAROTID SPACE ŌĆó Formed by all three layers of deep fascia ŌĆó Anatomically separate from all layers. ŌĆó Contains carotid artery, internal jugular vein, and vagus nerve ŌĆó ŌĆ£LincolnŌĆÖs HighwayŌĆØ ŌĆó Travels through para pharyngeal space ŌĆó Extends from skull base to thorax.
- 49. Anterior Visceral Space ŌĆó Infrahyoid ŌĆó Pretracheal space ŌĆó Enclosed by visceral division of middle layer of deep fascia ŌĆó Contains thyroid ŌĆó Surrounds trachea ŌĆó Superior border - thyroid cartilage ŌĆó Inferior border - anterior superior mediastinum down to the arch of the aorta. ŌĆó Posterior border ŌĆō anterior wall of esophagus ŌĆó Communicates laterally with the retropharyngeal space below the thyroid gland.
- 50. ŌĆó Iatrogenic perforation ( UGI ) ŌĆó FB ŌĆó Trauma ŌĆó Horizontal midline incision
- 51. Clinical presentation ŌĆó Most common symptoms ŌĆō Sore throat ŌĆō Odynophagia ŌĆō Neck swelling ŌĆō Neck Pain ŌĆó Pediatric ŌĆō Fever ŌĆō Decreased apetite ŌĆō Odynophagia ŌĆō Malaise ŌĆō Torticollis ŌĆō Neck pain ŌĆō Otalgia ŌĆō Trismus ŌĆō Neck swelling ŌĆō Vocal quality change ŌĆō Worsening of snoring, sleep apnea
- 52. FEVER ŌĆó Represents systemic involvement ŌĆó Due to Interleukin 1 ŌĆó < 102 0 -----’āĀ enhance phagocytic activity ŌĆó > 102 0 ----’āĀ sign of toxemia/ sepsis
- 53. BLOOD INVESTIGATIONS ŌĆó Screening Hemogram ’āĀLEUCOCYTOSIS 1. Lack of Leucocytosis ŌĆō tumour / Immunodeficiency status 2. Daily monitoring of response to the antibiotic / surgical drainage ŌĆó S. Creat / RBS/ B.urea - hydration status - Renal assessment
- 54. IMAGING - RADIOGRAPHY ŌĆó OPG( Orthopantogram) ŌĆō to r/o dental sources of infection ŌĆó STN - space involvement - status of airway - air-fluid level ’āĀ anaerobic org ŌĆó CXR - to r/o mediastinitis/ aspiration
- 55. IMAGING - USG ŌĆó Easy availability in emergency departments ŌĆó No radiation ŌĆó Cost effective
- 56. IMAGING -CECT ŌĆó CT is mandatory in all cases of deep neck infections 1. cellulitis/ frank abscess - Cellulitis ’āĀ intravenous antibiotics - Abscess ’āĀ Incision & drainage ŌĆ” Mc clay LE & Murray A, Booth. IV antibiotic therapy for DNSA defined by CT. Arch Otorhinolaryngology HNS 129; 1207-1212. 2003.
- 57. Cellulitis ŌĆō uniform heterogenous enhancement Abscess- peripheral rim enhancement
- 58. IMAGING- CT/ MRI ŌĆó CT with contrast ŌĆō Pros ŌĆó Widely available ŌĆó Faster ŌĆó Abscess vs cellulitis ŌĆó Less expensive ŌĆō Cons ŌĆó Contrast ŌĆó Radiation ŌĆó Uniplanar ŌĆó Dental artifacts ŌĆó MRI ŌĆō Pros ŌĆó MRI superior to CT in initial assessment ŌĆó More precise identification of space involvement (multiplanar) ŌĆó Better detection of underlying lesion ŌĆó Less dental artifact ŌĆó Better for floor of mouth ŌĆó No radiation ŌĆó Non iodine contrast ŌĆō Cons ŌĆó Cost ŌĆó Pt cooperation ŌĆó Slower
- 59. TREATMENT ŌĆó MEDICAL 1. AIRWAY 2. FLUID 3. ANTIBIOTIC ŌĆó SURGICAL 1. NEEDLE ASPIRATION 2. INCISION & DRAINAGE
- 61. AIRWAY Assessed by 1. Fibreoptic laryngoscope 2. Pulse oximetry ( not ideal ) Intervention by No obstruction :- Oxygen with face mask, humid air, steroid and epinephrine nebulization < 50 % obstruction : Medical Mx with observation in ICU > 50% obstruction : Intervention ŌĆó Fibreoptic intubation ŌĆó Oro tracheal intubation ŌĆó Tracheostomy Airway compromise is a major cause for mortality in Ludwigs angina, Parapharyngeal and retropharyngeal abscess
- 62. INDICATIONS FOR TRACHEOSTOMY ŌĆó Stridor / Stertor ŌĆó Aspiration- Inability to handle secretions
- 64. ODONTOGENIC ŌĆó The drug of choice for odontogenic infections continues to be parenteral penicillin. Even for serious fascial space infections, including Ludwig's angina, penicillin is preferred. Large doses of up to 20 million units daily for intravenous penicillin may be required for serious infections. ( with metronidazole ) ŌĆ”ŌĆ”Greenberg SL, et al: Surgical management of Ludwig's angina. Aust N Z J Surg 2007; 77:540-543. ŌĆó In the penicillin-allergic patient, clindamycin is the second drug of choice
- 65. ŌĆó Pennicillin ŌĆó 1st gen cephalosporins ŌĆó 2nd gen cephalosporins ŌĆó 3rd gen cephalosporins Anti streptolytic activity Anaerobic activity
- 66. FLUID RESUSCITATION ŌĆó ISOTONIC FLUIDS ŌĆō RL/NS/DNS ŌĆó MAINTENCE REGIMEN 4ml/kg/hr ’āĀ first 10 kgs 2ml/kg/hr ’āĀ next 5 kgs 1ml/kg/hr ’āĀ next subsequent kg
- 67. SURGERY INDICATIONS: 1. Air-fluid level in the neck or evidence of gas-producing organisms 2. abscess visualized in the fascial spaces of the head and neck 3. threatened airway compromise from abscess or phlegmon 4. failure to respond to 48 to 72 hours of empiric intravenous antibiotic therapy GOALS : - Tissue/ fluid for Grams staining & Culture sensitivity - therapeutic irrigation of the infected body cavity - stable external drainage pathway to prevent the reaccumulation of abscess
- 69. COMPLICATIONS ŌĆó LemierreŌĆÖs syndrome ŌĆó Cavernous sinus thrombosis ŌĆó Carotid artery pseudoaneurysm ŌĆó Mediastinitis ŌĆó Necrotizing fascitis
- 70. LemmiereŌĆÖs syndrome Tonsillar vein Bacteria spreads to IJV Toxin induces platelet aggregation Septic thrombi in IJV Lungs Joints- arthritis
- 71. ŌĆó MC organism ŌĆō Fusobacterium ŌĆó Inv ŌĆō CT neck with contrast ŌĆó Treatment : 1. Antibiotics 2. Heparin Anti-coagulation
- 72. Cavernous sinus Thrombosis Para nasal Sinus Facial planes Upper dention Ophthalmic Vn CST
- 73. Carotid Artery Pseudoaneurysm / rupture ŌĆó Pulsatile neck mass ŌĆó Horners syndrome ŌĆó Lower cranial nerve palsies ŌĆó Echymosis of neck ŌĆó If rupture ’āĀ bright red blood from mouth and nose
- 74. Necrotizing Fascitis ŌĆó More common in Diabetics and immunocompromised * ŌĆó Rapidly progressing cellulitis with ptting neck edema and orange peel appearance of skin ŌĆó No frank pus ŌĆó Foul smelling grey-brown tissue fluid with necrotic tissue ( Liquefactive necrosis ) ŌĆó Necrotic tissue must be debrided ŌĆó Wound should be left open ŌĆó May require repeated debridement ( rule rather than exception ) ŌĆó Hyperbaric oxygen may help *Tung-Yiu W, Jehn-Shyun H, Ching-Hung C, et al: Cervical necrotizing fasciitis of odontogenic origin: a report of 11 cases. J Oral Maxillofac Surg 2000; 58:1347-1352.
- 75. Mediastinitis ŌĆó Etio :- retropharyngeal & parapharyngeal infections ŌĆó C/F :- Diffuse neck edema Dyspnea Pleuritic chest pain , inc. on breathing Tachycardia & hypoxia Interscapular pain ŌĆó CT Thorax ŌĆó Broad spectrum antibiotic ŌĆó Thoracotomy sos
- 76. ŌĆ£Pus in the neck calls for the surgeons best judgement, his best skill and often for all his courageŌĆØ ŌĆ”ŌĆ”ŌĆ”ŌĆ”ŌĆ”.. Mosher on Deep Neck Infections References: 1. Cummings Otorhinolaryngology & HNS 5th edition. 2. Scott brownŌĆÖs Otorhinolarynogoly & HNS 6th Edition 3. Eugene MyerŌĆÖs Operative