Steps of spermatogenesis powerpoint presentation
- 2. Learning Objectives ÔÇó Define the processes of spermatogenesis and spermiogenesis. ÔÇó Describe the stages of spermatogenesis in the seminiferous tubule, including the roles of the sustentacular and Sertoli cells and interstitial cells of Leydig. ÔÇó Describe hormonal regulation of spermatogenesis.
- 3. Spermatogenesis is the process by which male primary sperm cells undergo meiosis and produce a number of cells calls spermatogonia, from which the primary spermatocytes are derived. Each primary spermatocyte divides into two secondary spermatocytes and each secondary spermatocyte into two spermatids or young spermatozoa. These develop into mature spermatozoa, also known as sperm cells. Thus, the primary spermatocyte gives rise to two cells, the secondary spermatocytes, which in turn produce four spermatozoa. Spermatogenesis is the male version of gametogenesis and results in the formation of spermatocytes possessing half the normal complement of genetic material.
- 4. Spermatogenesis ÔÇó Haploid cells produced via spermatogenesis. ÔÇó Diploid spermatogonium in seminiferous tubules. (mitosis ´âá 2 diploid primary spermatocytes). ÔÇó Primary spermatocyte ´âá meiosis I ´âá 2 haploid secondary spermatocytes. ÔÇó Haploid secondary spermatocytes ´âá meiosis II ´âá 4 haploid spermatids. ÔÇó Each spermatid grows a tail and a mitochondrial-filled midpiece, ÔÇó Chromatin is tightly packaged into an acrosome at the head. ÔÇó Maturation removes excess cellular material, ÔÇó Spermatids ´âá inactive, sterile spermatozoa that are transported via peristalis to the epididymus. ÔÇó The spermatozoa gain motility in the epididymus, but do not use that ability until they are ejaculated into the vagina. ÔÇó Spermatogenesis requires optimal environmental conditions.
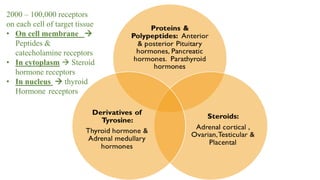
- 5. 2000 ÔÇô 100,000 receptors on each cell of target tissue ÔÇó On cell membrane ´âá Peptides & catecholamine receptors ÔÇó In cytoplasm ´âá Steroid hormone receptors ÔÇó In nucleus ´âá thyroid Hormone receptors
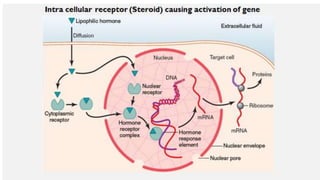
- 6. Cont.  bind to specific receptors at the target cell  initiates a cascade of reactions in the cell.  Receptor proteins are inactivated / destroyed or reactivated on demand.  different functions are elicited in different target cells  adrenal , gonadal steroid hormones, thyroid hormones, retinoid hormones, and vitamin D.  Activated hormone receptor complex binds with a specific regulatory (promoter) sequence of the DNA (hormone response element),  activates or represses transcription of specific genes and formation of messenger RNA (mRNA)  May take minutes, hours, or even days after the hormone has entered the cell due to genetic involvement.
- 7. ÔÇó Steroid Hormones Increase Protein Synthesis, activates cells functions. ÔÇó hormone enters cytoplasm , binds with receptor protein ÔÇó combined receptor proteinÔÇôhormone diffuses into nucleus. ÔÇó Binds at specific points on DNA strands in chromosomes ÔÇó activates transcription of specific genes to form mRNA. ÔÇó mRNA diffuses into the cytoplasm ÔÇó promotes translation at ribosomes to form new proteins. E.g;, aldosterone
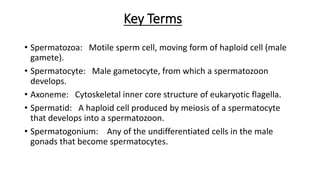
- 10. Key Terms ÔÇó Spermatozoa: Motile sperm cell, moving form of haploid cell (male gamete). ÔÇó Spermatocyte: Male gametocyte, from which a spermatozoon develops. ÔÇó Axoneme: Cytoskeletal inner core structure of eukaryotic flagella. ÔÇó Spermatid: A haploid cell produced by meiosis of a spermatocyte that develops into a spermatozoon. ÔÇó Spermatogonium: Any of the undifferentiated cells in the male gonads that become spermatocytes.
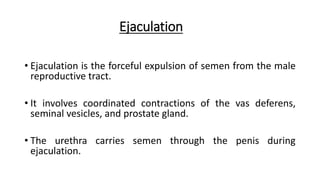
- 11. Ejaculation ÔÇó Ejaculation is the forceful expulsion of semen from the male reproductive tract. ÔÇó It involves coordinated contractions of the vas deferens, seminal vesicles, and prostate gland. ÔÇó The urethra carries semen through the penis during ejaculation.
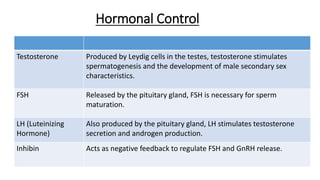
- 12. Hormonal Control Testosterone Produced by Leydig cells in the testes, testosterone stimulates spermatogenesis and the development of male secondary sex characteristics. FSH Released by the pituitary gland, FSH is necessary for sperm maturation. LH (Luteinizing Hormone) Also produced by the pituitary gland, LH stimulates testosterone secretion and androgen production. Inhibin Acts as negative feedback to regulate FSH and GnRH release.
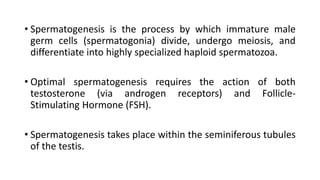
- 13. ÔÇó Spermatogenesis is the process by which immature male germ cells (spermatogonia) divide, undergo meiosis, and differentiate into highly specialized haploid spermatozoa. ÔÇó Optimal spermatogenesis requires the action of both testosterone (via androgen receptors) and Follicle- Stimulating Hormone (FSH). ÔÇó Spermatogenesis takes place within the seminiferous tubules of the testis.
- 14. Transport of Sperm ÔÇó Spermatozoa mature in the epididymis, where they gain motility and the ability to fertilize an egg. ÔÇó During ejaculation, sperm travel through the vas deferens to mix with seminal fluid.
- 15. ÔÇó Spermatozoa (mature male gametes) formed. ÔÇó In testes and epididymis (approximately 64 days). ÔÇó Essential for sexual reproduction. ÔÇó Dependent upon optimal conditions to occur correctly. ÔÇó Starts at puberty ,continues till death, declines with age.
- 16. ÔÇó of the steps of spermatocytogenesis, including type Ad spermatogonium, type Ap Spermatogonium, type B spermatogonium, primary spermatocyte, and secondary spermatocyte. ÔÇó Mitotic division of a diploid spermatogonium that resides in the basal compartment of the seminiferous tubules, resulting in two diploid intermediate cells called primary spermatocytes. ÔÇó Each primary spermatocyte then moves into the adluminal compartment of the seminiferous tubules, duplicates its DNA, and subsequently undergoes meiosis I to produce two haploid secondary spermatocytes. .
- 17. ÔÇó Secondary spermatocytes later divide into haploid spermatids. During this division, random inclusion of either parental chromosome and chromosomal crossover both increase the genetic variability of the gamete. ÔÇó Each cell division from a spermatogonium to a spermatid is incomplete; the cells remain connected to one another by bridges of cytoplasm to allow synchronous development. Not all spermatogonia divide to produce spermatocytes; otherwise, the supply would run out. Instead, certain types of spermatogonia divide to produce copies of themselves, thereby ensuring a constant supply of gametogonia to fuel spermatogenesis
- 18. ÔÇó Steps in Spermatogenesis ÔÇó Step 1: Spermatocytogenesis ÔÇó Step 2: Spermatidogenesis ÔÇó The creation of spermatids from secondary spermatocytes. Secondary spermatocytes produced earlier rapidly enter meiosis II and divide to produce haploid spermatids. The brevity of this stage means that secondary spermatocytes are rarely seen in histological preparations.
- 19. ÔÇó Step 3: Spermiogenesis ÔÇó At this stage, each spermatid begins to grow a tail and develop a thickened midpiece where the mitochondria gather and form an axoneme. Spermatid DNA also undergoes packaging, becoming highly condensed. The DNA is packaged with specific nuclear basic proteins, which are subsequently replaced with protamines during spermatid elongation. The resultant tightly packed chromatin is transcriptionally inactive. The Golgi apparatus surrounds the now condensed nucleus, becoming the acrosome. One of the centrioles of the cell elongates to become the tail of the sperm.
- 20. ÔÇó The non-motile spermatozoa are transported to the epididymis in testicular fluid secreted by the Sertoli cells with the aid of peristaltic contraction. While in the epididymis, the spermatozoa gain motility and become capable of fertilization. However, transport of the mature spermatozoa through the remainder of the male reproductive system is achieved via muscle contraction rather than the spermatozoonÔÇÖs recently acquired motility.
- 21. Physiology of Spermatogenesis ÔÇó Seminiferous Tubule ÔÇó Seminiferous Tubule: Micrograph showing seminiferous tubule with maturing sperm. ÔÇó Maturation takes place under the influence of testosterone, which removes the remaining unnecessary cytoplasm and organelles. The excess cytoplasm, known as residual bodies, is phagocytosed by surrounding Sertoli cells in the testes. The resulting spermatozoa are now mature but lack motility, rendering them sterile. The mature spermatozoa are released from the protective Sertoli cells into the lumen of the seminiferous tubule in a process called spermiation.
- 22. ÔÇó Spermatogenesis is highly sensitive to fluctuations in the environment, particularly hormones and temperature. Seminiferous epithelium is sensitive to elevated temperature in humans and is adversely affected by temperatures as high as normal body temperature. Consequently, the testes are located outside the body in a sack of skin called the scrotum. The optimal temperature is maintained at 2 ┬░C below body temperature in human males. This is achieved by regulation of blood flow and positioning towards and away from the heat of the body by the cremaster muscle and the dartos smooth muscle in the scrotum. Dietary deficiencies (such as vitamins B, E, and A), anabolic steroids, metals (cadmium and lead), x-ray exposure, dioxin, alcohol, and infectious diseases will also adversely affect the rate of spermatogenesis.
- 24. ÔÇó Male sexual response is demonstrated by vasodilation and blood engorgement of the penis, leading to an erection. ÔÇó The testes rise and grow larger and warmer as blood pressure rises. ÔÇó The muscles of the pelvic floor, the vesicles, and the prostrate contract, injecting sperm into the urethra of the penis and resulting in the onset of orgasm. ÔÇó Ejaculation continues with orgasm. ÔÇó Following orgasm, there is a gradual loss of erection and a feeling of relaxation known as the refractory period. ÔÇó Cognitive factors involving visual stimuli and high levels of activity in the amygdala and hypothalamus contribute to sexual arousal and sexual response in males.
- 25. ÔÇó erection: The physiological process by which a penis becomes engorged with blood. ÔÇó sexual arousal: Changes that occur during or in anticipation of sexual activity. ÔÇó refractory period: The period after excitation, during which a membrane recovers its polarization and is not able to respond to a second stimulus. ÔÇó sex flush: Increased blood flow leading to reddening of the skin in response to sexual arousal or orgasm. ÔÇó tumescence: The normal engorgement of the erectile tissue with blood. ÔÇó genitalia: Sex organs.
- 26. Sperm Physiology and Function ÔÇó In animals, most of the energy (ATP) for sperm motility is derived from the metabolism of fructose carried in the seminal fluid. This takes place in the mitochondria located in the spermÔÇÖs midpiece. This energy is used for the journey through the female cervix, uterus, and uterine tubes. ÔÇó Motile sperm cells typically move via flagella and require a water medium in order to swim toward the egg for fertilization.These cells cannot swim backwards due to the nature of their propulsion. The uniflagellated sperm cells (with one flagellum) of animals are referred to as spermatozoa.
- 27. ÔÇó This sperm diagram indicates the acrosome, plasma membrane, nucleus, centriole, mitochondria, terminal disc, axial filament, head, midpiece, tail, endpiece, periacrosomal space, cell membrane, acrosome, nuclear vacuoles, nucleus, nuclear envelope, subacrosomal space, outer acrosome membrane, ecuatorial segment, postacrosomal region, postacrosomal sheet, posterior ring, connecting piece, redundant nuclear envelope, mitochondrial sheath, outer dense fibers, central pair, and axoneme.