Sterilisation & disinfection
- 1. Moderator: Dr.K.S.Dhillon HOD, Dept. of Gen. Surgery Max super speciality Hospital, Mohali, Punjab Presenter : Dr. Asif Mian Ansari DNB resident Dept. of General Surgery Max hospital, Mohali
- 2. ’éĪ Terminology ’éĪ Introduction ’éĪ Levels of disinfection ’éĪ Types of items/devices ’éĪ Common methods of cleaning, disinfection & sterilization ’éĪ Factors affecting steriization
- 3. ’éĪ Sterilization: ’é¦ Destroys all forms of microbial life + bacterial spores ’éĪ Disinfection: ’é¦ Destroys many or all pathogenic microorganisms- except bacterial spores ’éĪ Cleaning: ’é¦ Removal of visible soil from objects and surfaces ’éĪ Antisepsis: ’é¦ Prevent sepsis (infection) by killing infectious microorganisms ’éĪ Sanitize: ’é¦ Reduce the number of micoorganisms
- 4. ’éĪ Surgical/medical procedure ’āĀ instrument contact with patientŌĆÖs tissues ’āĀ risk of pathogen transfer ’éĪ Failure to sterilize/disinfect instrument ’āĀ pathogen entry to patient or transfer of infection ’éĪ Sterilization is not required for all instruments as Disinfection or cleaning is sufficient for them ’éĪ Instruments classification according to risk of infection (Spaulding classification)
- 6. Resistance to biocides MOST RESISTANT LEAST RESISTANT Bacterial spores Sterilization Mycobacteria High level disinfection Non-lipid or small virus (poliovirus) Intermediate disinfection Fungi Low level disinfection Lipid or medium sized virus (HIV) Vegetative bacteria
- 7. ’éĪ Cleaning ’éĪ Disinfection ’éĪ Sterilization
- 8. ’éĪ Removal of foreign material (soil/organic material) ’éĪ Water with detergents ’éĪ Enzymatic methods ’éĪ Mandatory before disinfection or sterilization ’éĪ Friction : rubbing/scrubbing the soiled area with a brush ’éĪ Fluidics : fluids under pressure is used to remove soil / debris ’éĪ Neutral or near neutral pH solution with detergent is used ’éĪ Enzymes : proteases/lipases/amylases some times added to neutral pH solutions
- 9. ’éĪ Destruction of many or all pathogenic microorganisms - except bacterial spores ’éĪ Required for non-critical and semi-critical items ’éĪ Chemicals or combination of chemicals registered with EPA (environmental protection agency) or FDA (food and drug administration) ’éĪ Used in standard concentration
- 10. ’é¦ Ethyle alcohol and iso-propyle alcohol ’é¦ Kill all microbes except bacterial spores ’é¦ MOA: protein denaturation ’é¦ Ethyle alcohol (30 ŌĆō 100%): bactericidal & virucidal in 10-15 sec including tubercle bacilli ’é¦ Iso propyle alcohol is more potent and used in less concentrations ’é¦ Uses : disinfection of thermometers, stethoscopes, USG probes, medication preparation areas ’é¦ Limitations : damage to shellac mountings of lens, tend to harder rubber tubings after prolonged use, damage tonometer tips. It is flammable ’é¦ Chlorhexidine (2.5 %) + alcohol combination (70 %)
- 11. ’éĪ Sodium hypochlorite (5.25 - 6.15% ) : household bleech ’éĪ Remove dried or fixed organisms and biofilms from surfaces ’éĪ Superoxide water : hypochlorous acid + chlorine ’éĪ Others : chlorine dioxide, sodium dichloroisocyanurate, and chloramine-T ’éĪ MOA : active component is HOCl > OCl- ’é¦ oxidation of sulfhydryl enzymes and amino acids ’é¦ inhibition of protein synthesis ’é¦ decreased oxygen uptake ’é¦ decreased ATP production ’é¦ depressed DNA synthesis
- 12. ’éĪ Uses: ’é¦ A 1:10ŌĆō1:100 dilution of 5.25%ŌĆō6.15% sodium hypochlorite solution for decontaminating blood spills ’é¦ Chlorine tablets have been used as the disinfectant of water ’éĪ Adverse effects: ’é¦ Can produce ocular irritation or oropharyngeal, esophageal, and gastric burns ’é¦ Corrosiveness to metals ’é¦ Carcinogenic : chloromethyl and trihalomethane
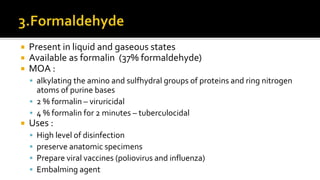
- 13. ’éĪ Present in liquid and gaseous states ’éĪ Available as formalin (37% formaldehyde) ’éĪ MOA : ’é¦ alkylating the amino and sulfhydral groups of proteins and ring nitrogen atoms of purine bases ’é¦ 2 % formalin ŌĆō viruricidal ’é¦ 4 % formalin for 2 minutes ŌĆō tuberculocidal ’éĪ Uses : ’é¦ High level of disinfection ’é¦ preserve anatomic specimens ’é¦ Prepare viral vaccines (poliovirus and influenza) ’é¦ Embalming agent
- 14. ’éĪ Aqueous solutions of glutaraldehyde are acidic ’āĀ not sporicidal ’éĪ Activated solution (made alkaline) at pH 7.5ŌĆō8.5 ’āĀ sporicidal ’éĪ Activated solution half life is 14 days ’éĪ MOA : Alkylation of sulfhydryl, hydroxyl, carboxyl groups, which alters RNA, DNA, and protein synthesis ’éĪ Minimum effective concentration ’āĀ 1.0%ŌĆō1.5% ’éĪ >2% glutaraldehyde solution as a high-level disinfectant ’éĪ Uses : ’é¦ As a high-level disinfectant for endoscopes, spirometry tubing, dialyzers, transducers, anesthesia and respiratory therapy equipments
- 15. ’é¦ As a high-level disinfectant for reuse of laparoscopic disposable plastic trocars ’é¦ Noncorrosive to metal ’é¦ Does not damage lensed instruments, rubber or plastics ’é¦ Too toxic and expensive ’āĀ Should not be used for cleaning noncritical surfaces
- 16. ’éĪ FDA listed it as a sterilant & high-level disinfectant ’éĪ MOA : producing destructive hydroxyl free radicals which attacks membrane lipids, DNA, and other essential cell components & destroys cell ’éĪ Uses : ’é¦ 3% to 6% for disinfecting soft contact lenses, tonometer, biprisms, ventilators, fabrics and endoscopes
- 17. ’éĪ Iodine solutions or tinctures used by health professionals primarily as antiseptics or disinfectant ’éĪ MOA : iodophors ’āĀ Iodine ’āĀ penetrate the cell wall of microorganisms quickly ’āĀ disruption of protein and nucleic acid ’éĪ Povidone iodine ’éĪ Uses : ’é¦ As an antiseptic ’é¦ As a disinfectant for blood culture bottles, thermometers & endoscopes
- 18. ’éĪ It contains 0.55% 1,2-benzenedicarboxaldehyde (OPA) ’éĪ Is a high-level disinfectant ’éĪ MOA : ’é¦ Interact with amino acids & proteins ’é¦ Kills spores by blocking the spore germination process ’éĪ Advantages over glutaraldehyde : Not irritant to the eyes and nasal, has a barely perceptible odor and requires no activation ’éĪ Disadvantage of OPA is that it stains proteins gray including skin
- 19. ’éĪ Peracetic acid is characterized by rapid action against all microorganisms ’éĪ It is an oxidizing agent ’éĪ Uses : ’é¦ chemically sterilize medical, surgical, and dental instruments ’é¦ Peracitic acid with hydrogen peroxide (0.23 % with 7.35%) kills all microorganisms except bacterial spores within 20 minutes and used for disinfecting hemodialyzers
- 20. ’éĪ Two phenol derivatives commonly used as hospital disinfectants ’āĀ ortho-phenylphenol and ortho-benzyl-para- chlorophenol ’éĪ MOA : In high concentrations, phenol acts as a protoplasmic poison, penetrating and disrupting the cell wall ’éĪ Uses : As disinfectants for bedside tables, bedrails, and laboratory surfaces and noncritical medical devices
- 21. ’éĪ Fungicidal, bactericidal, and virucidal against lipophilic (enveloped) viruses but not sporicidal, tuberculocidal or virucidal against hydrophilic (nonenveloped) viruses ’éĪ MOA : Inactivation of energy-producing enzymes ’éĪ Uses : environmental sanitation of noncritical surfaces, such as floors, furniture, and walls ’éĪ Benzalkonium chloride
- 23. ’éĪ Sterilization destroys all microorganisms on the surface of an article ’éĪ All critical items require sterilization before use ’éĪ Most medical and surgical devices are heat stable and undergo heat sterilization ’éĪ Now, increase in medical devices and instruments made of materials that are heat labile & require low-temperature sterilization
- 24. ’éĪ Steam under pressure ’āĀ most widely used ’éĪ Nontoxic, inexpensive, rapidly microbicidal & sporicidal ’éĪ Principle : four parameters : steam, pressure, temperature, and time ’éĪ Two common steam-sterilizing temperatures ’é¦ 121┬░C + 15 psi for 30 minutes ’é¦ 132┬░C + 30 psi for 4 minutes ’éĪ The two basic types of steam sterilizers (autoclaves) ’é¦ Gravity displacement autoclave ’é¦ High-speed prevacuum sterilizer
- 25. ’éĪ The effectiveness of steam sterilization is monitored with a biological indicator containing spores of Geobacillus stearothermophilus ’éĪ MOA : irreversible coagulation and denaturation of enzymes and structural proteins ’éĪ Uses : used whenever possible on all critical and semicritical items that are heat and moisture resistant
- 26. ’éĪ Sterilization of an unwrapped objects to allow for rapid penetration of steam ’éĪ In gravity displacement or prevacuum autoclave non porous items to be kept at 132┬░C for 3 minutes ’éĪ For porous items duration is 10 & 4 minutes respectively in In gravity displacement & prevacuum autoclave ’éĪ Used when items need rapidly to be sterilized ’éĪ Risk of contamination is more during transportation
- 28. ’éĪ Used for Heat & moisture sensitive items ’éĪ Temperature < 60┬░C
- 29. ’éĪ Colorless, flammable and explosive gas ’éĪ Requirements : ’é¦ gas concentration (450 to 1200 mg/l); ’é¦ temperature (37 to 63┬░C); ’é¦ relative humidity (40 to 80%) ’é¦ exposure time (1 to 6 hours) ’éĪ ETO sterilization cycle consists of five stages : preconditioning and humidification, gas introduction, exposure, evacuation, and air washes ’éĪ MOA: alkylation of protein, DNA, and RNA
- 30. ’éĪ Uses: ETO is used to sterilize moisture or heat sensitive critical items and sometimes semicritical items ’éĪ Disadvantage: ’é¦ lengthy cycle time ’é¦ Cost ’é¦ potential hazards to patients and staff (acute inhalation causes irritation of mucus membranes & Chronic inhalation has been linked to the formation of cataracts, cognitive impairment, neurologic dysfunction, and disabling polyneuropathies and cancers)
- 31. ’éĪ Gas plasma is the fourth state of matter ’éĪ Charged gas particles ’éĪ Hydrogen Peroxide Gas vapors at 6 mg/l concentration is diffused in an evacuated chamber.An electrical field created by a radio frequency is applied to the chamber to create a gas plasma and inactivation of microbes starts ’éĪ Takes around 50 minutes (28-38 minutes in newest version) ’éĪ MOA: free radicals injury and hydrogen peroxide gas activity ’éĪ Indicator : Bacillus atrophaeus spores ’éĪ Use : plastics, electrical devices, and corrosion-susceptible metal alloys
- 32. ’éĪ Highly biocidal oxidizer that maintains its efficacy in the presence of organic soil ’éĪ This microprocessor-controlled, low-temperature (50┬░C) sterilization method is commonly used for sterilization of endoscopes, arthroscopes and bronchoscopes ’éĪ 35% peracetic acid, and an anticorrosive agent are supplied in a single-dose container ’āĀ container is punctured at the time of use, immediately prior to closing the lid and initiating the cycle ’éĪ Indicator : G. stearothermophilus spore strips
- 33. ’éĪ MOA: oxidize & denatures proteins, disrupts cell wall permeability ’éĪ Uses: ’é¦ endoscopes, bronchoscopes sterilizaton ’é¦ Peracitic acid with hydrogen peroxide : disinfection of hemodialysers
- 34. ’éĪ Ionizing Radiation: ’é¦ by cobalt 60 gamma rays or electron accelerators ’éĪ Dry-Heat Sterilizers: ’é¦ Only for materials that might be damaged by moist heat or that are impenetrable to moist heat (e.g., powders, petroleum products, sharp instruments) ’é¦ 170┬░C for 60 minutes, 160┬░C for 120 minutes, and 150┬░C for 150 minutes. ’é¦ B. atrophaeus spores used as indicator
- 35. ’éĪ Performic Acid: fast-acting sporicide that is used in an automated endoscope reprocessing system. Not currently FDA cleared. ’éĪ Filtration: used to remove bacteria from thermolabile fluids that cannot be purified by any other means. Standard membrane pore size is 0.22 ╬╝m. Not currently FDA cleared. ’éĪ Microwave: used for disinfection of soft contact lenses, dental instruments, dentures, milk etc.
- 36. ’éĪ Ozone : ozone as the sterilant, was cleared by FDA in August 2003. duration of cycle is about 4 h and 15 m, and it occurs at 30-35┬░C. Can be used for stainless steel, titanium, anodized aluminum, ceramic, glass, silica, PVC,Teflon, silicone, polypropylene, polyethylene and acrylic ’éĪ Formaldehyde Steam: A formaldehyde concentration of 8-16 mg/l is generated at an operating temperature of 70-75┬░C. Initial vacuum ’āĀ steam admission ’āĀ series of pulses of formaldehyde gas ’āĀ followed by steam & air flushing pulses. Not FDA cleared
- 37. ’éĪ Cleaning ’éĪ Bioburden ’éĪ Pathogen type ’éĪ Protein & salt ’éĪ Biofilm accumulation ’éĪ Restricted flow ’éĪ Device design and construction
- 38. ’éĪ Not all instruments need sterilization ’éĪ In some situation semi-critical items may work as critical items ’āĀ should be sterilized ’éĪ Autoclaving & ETO are most widely used methods ’éĪ Cleaning is essential part before disinfection or sterilization