Stoma care basics n
- 2. Two basic types of diversions ïŪ Urinary ïŪ Fecal
- 4. Reasons for diversions ïŪ Removal of bladder from cancer ïŪ Neurogenic bladder, congenital anomalies, strictures, trauma to the bladder, and chronic infections with deterioration of renal function
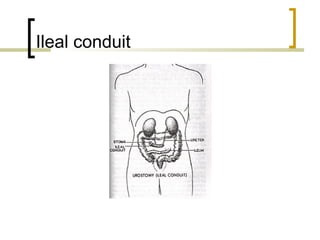
- 5. Types of diversions ïŪ Incontinent ïĄ Ileal conduit ïĄ Cutaneous ureterostomy ïĄ Nephrostomy
- 6. Ileal Conduit ïŪ Most common type ïŪ Ureters are implanted into a segment of the ileum that has been resected. Ureters are anastomosed into one end of the conduit and the other end is brought out through the abdominal wall to form a stoma. ïŪ There is no valve or voluntary control. ïŪ Advantages: good urine flow with few physiologic alterations. ïŪ Disadvantages: surgical procedure is complex. Must wear an external collecting device. Must care for stoma and drainage bag.
- 8. Cutaneous ureterostomy ïŪ Ureters are excised from the bladder and brought through the abdominal wall to form stoma. ïŪ Advantages: Not considered major surgery ïŪ Disadvantages: External collecting device must be worn. Possibility of stricture or stenosis of small stoma.
- 10. Nephrostomy ïŪ Catheter is inserted into the pelvis of the kidney. May be done ot one or both kidneys and may be temporary or permanent. Most frequently done in advanced disease as a palliative measure. ïŪ Advantage: No need for major surgery ïŪ Disadvantage: High risk of renal infection. Predisposition to calculus formation from catheter. May have to be changed every month. Catheter should not be clamped, should remain open.
- 12. Continent Diversions ïŪ Kock Pouch-loops of intestine are anastomosed together and then connected to the abdomen via the stomal segment. Ureters are attached to the pouch above a valve, which prevents reflux of urine to the kidney. A second valve is placed in the intestinal segment leading to the stoma.
- 13. Kock Pouch
- 14. Indiana Pouch ïŪ Ureters are anastomosed to the colon portion of the reservoir in a manner to prevent reflux. The ileocecal valve is used to provide continence and the section of ileum that extends from the intestinal reservoir to the skin is made narrower to prevent urine leakage.
- 15. Indiana Pouch
- 16. Continent urinary diversions ïŪ The stoma is usually flush with the skin and placed lower on the abdomen than the ileal conduit stoma. ïŪ Patient will need to self-catheterize every 4-6 hours and will need to irrigate the internal reservoir to remove mucus, but will not have to wear an external collection device.
- 17. Complications ïŪ Breakdown of the anastomoses in the GI tract. ïŪ Leakage from the ureteroileal or ureterosigmoid anastomosis ïŪ Paralytic ileus ïŪ Obstruction of ureters ïŪ Wound infection ïŪ Mucocutaneous separation ïŪ Stomal necrosis
- 18. Wound infection
- 20. Stomal necrosis
- 21. Nursing Management ïŪ Pre-op Care ïĄ Assess ability and readiness to learn before initiating a teaching program ïĄ Involve the patientâs family in the teaching process ïĄ Teach the patient who will have a continent diversion how to catheterize and irrigate and adhere to a strict schedule ïĄ Arrange pre-op meetings for patient with WOC (ET) nurse and with volunteer from United Ostomy Association ïĄ Patient will require complete bowel clean-out. Assist as needed with bowel prep as ordered. ïĄ Allow patient/family opportunity to explore feelings and begin to cope with changes.
- 22. Remember ïŪ Patients who have been well informed about the surgical procedure, post- operative period and long-term management goals are better able to adjust to the entire experience than those who have not.
- 23. Postoperative Care ïŪ Stents placed in ileal conduit for 7-10 days to promote urinary drainage. If continent urostomy, will have catheter or stent in stoma (sutured in place) to allow drainage from reservoir. ïŪ Drain tube in pelvic area for drainage of blood and surgical fluids. ïŪ May have NG tube until effective intestinal peristalsis returned. May then start on clear liquids to advance as tolerated.
- 24. Postoperative care ïŪ With ileal conduit, clear pouch placed over stoma so that it can be easily assessed. ïŪ Careful visualization of stoma in contact with catheter. ïŪ Monitor urine output carefully. ïŪ Blood in urine is expected in immediate postop period with gradual clearing. ïŪ Mucus is present in urine because it is secreted by the intestines as a result of the irritating effect of the urine.
- 25. Postoperative care ïŪ High fluid intake is encouraged to flush the ileal conduit or continent diversion. ïŪ Be aware that patient is at greater risk for UTI. ïŪ Stomal or loop stenosis may result in urine being retained in the conduit with subsequent electrolyte imbalances.
- 26. Postoperative care ïŪ Strive to keep urine acidic. Alkaline urine promotes encrustation and stone formation. ïŪ Ileal conduit stoma edema will begin to subside within 7 days after surgery and continue to decrease in size gradually for the next 6 to 8 weeks.
- 27. Postoperative care ïŪ Elderly and patients with limited manual dexterity may need special assistance. ïŪ Patients need to know where to purchase supplies, emergency telephone numbers, ostomy support group contact information, follow-up appointments with nurse and doctor. ïŪ Problems with the stoma may include bleeding, stenosis or prolapse.
- 28. Stomal prolapse
- 29. Bowel Diversions ïŪ Incontinent types of diversions: Colostomy-opening between the colon and the abdominal wall. ïŪ Ascending colostomy: semi-liquid stool consistency, increased fluid requirements, needs appliance and skin barriers, cannot be irrigated. Indications for surgery: perforating diverticulitis in lower colon, trauma, inoperable tumors of colon, rectum or pelvis, rectovaginal fistula.
- 30. Colostomies Transverse colostomy: Semi-formed stool consistency, possibly increased fluid requirement, uncommon bowel regulation, requires appliance and skin barrier, cannot irrigate. Indications for surgery: Same as for ascending colostomy. May also be performed in children who are born with imperforate anus
- 31. Colostomies ïŪ Sigmoid colostomy-Formed stool consistency, no change in fluid requirements, bowel regulation possible with irrigations and/or diet; need for appliances and barriers dependent on regulation. ïŪ Indications for surgery: cancer of the rectum or rectosigmoid area, perforating diverticulum, trauma.
- 32. Ileostomy ïŪ Opening from the ileum or small intestine through the abdominal wall. Bypasses the entire large intestine. Stool is liquid to semiliquid consistency and contains proteolytic enzymes, Increased fluid requirement. No bowel regulation or irrigation. Requires wearing an appliance and skin barrier. ïŪ Indications for surgery: ulcerative colitis, Crohnâs disease, trauma, cancer, birth defect, familial polyposis.
- 33. Surgical interventions ïŪ Loop stoma-Closure of colostomy is anticipated. Temporary large stoma where loop of bowel is brought to abdominal surface and opening created in anterior wall of bowel to provide fecal diversion. One stoma with a proximal (drains stool) and distal (drains mucus) opening and an intact posterior wall that separates the two openings. The loop is sutured to the abdominal wall and held in place with a plastic rod for 7-10 days.
- 34. Loop stoma
- 35. End Stoma ïŪ One stoma formed from the proximal end of the bowel with the portion of the GI tract either removed (permanent) or sewn closed (Hartmannâs pouch) and left in the abdominal cavity.
- 36. End stoma with Hartmannâs pouch
- 37. Double-barrel stoma ïŪ Bowel is surgically severed and two ends are brought out onto the abdomen as two separate stomas. The proximal end is the functional stoma. The distal end is nonfunctioning, called a mucus fistula. Intended as a temporary diversion in cases where resection is required due to perforation or necrosis.
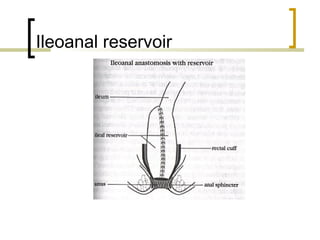
- 39. Continent fecal diversions ïŪ Ileoanal pull-through-The colon is removed and ileum is anastomosed or connected to an intact anal sphincter. ïŪ Ileoanal reservoir-Internal pouch created from ileum. End of pouch sewn or anastomosed to the anus. Surgery is done in several stages and patient may have a temporary colostomy (6-12 weeks) until ileal pouch is healed.
- 41. Kock Pouch ïŪ Internal pouch created from a segment of the ileum. Part of the pouch is brought out low onto the abdomen as the external stoma. A one-way nipple valve allows fecal contents to drain when a catheter is intermittently inserted in the stoma. No external collecting device is required. Immediately after surgery, a drainage catheter is left in place for 2-4 weeks. This catheter is irrigated with 20 ml of NS every 3-4 hours. Patients are taught to catheterize intermittently with 28fr. Catheter.
- 42. Special considerations for patients who have ileoanal reservoirs ïŪ Kegel exercises will help them to strengthen the pelvic floor and provide muscle control for continence. ïŪ May have mucus discharge from rectum. ïŪ May have frequent stools. Must be meticulous with perianal skin care and use barrier (zinc oxide) consistently. ïŪ Eliminate foods known to increase bowel activity and add foods that slow activity. ïŪ Increase fiber, decrease sugars. ïŪ May need Metamucil, antidiarrheals. ïŪ May have night incontinence and have to wear a pad to bed. ïŪ Should not respond to every urge to defecate to help increase pouch capacity.
- 43. Nursing Management- preoperative ïŪ Focus on patient teaching ïŪ Introduce WOC(ET) nurse to patient ïŪ Determine patientâs ability to perform self care, identify support systems ïŪ Identify potential problems that could be modified to facilitate learning
- 44. More to consider pre-op ïŪ United Ostomy Association (UOA) can send a trained ostomy visitor to talk with the patient. This can help by providing psychological support. ïŪ Nurse will be administering osmotic lavage (Go-Lytely) and giving IV and oral antibiotics. Neomycin and erythromycin are given orally to decrease the number of intracolonic bacteria.
- 45. Nursing Management- postoperative ïŪ Focus on assessing the stoma, protecting the skin, selecting the pouch and assisting the patient to adapt psychologically to the body change. ïŪ Observe for the type of stoma, color, size, location of stoma, and peristomal skin.
- 46. More post op considerations: Stomal characteristics Mucosa is rose to brick red Pale may indicate anemia Blanching, dark red or purple indicates inadequate blood supply to the stoma or bowel from adhesions, low flow states, or excessive tension on the bowel at the time of construction. Black indicates necrosis. Stoma should be assessed and color documented every 8 hours.
- 47. Good stoma Bad stoma
- 48. What else should you expect to see when you examine the stoma? ïŪ There should be mild to moderate edema in the first 5-7 days post-op. Severe edema may indicate obstruction of the stoma, allergic reaction to food or gastroenteritis. ïŪ Blood oozing from the stomal mucosa when touched is normal because it is so vascular.
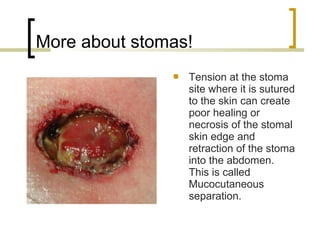
- 49. More about stomas! ïŪ Tension at the stoma site where it is sutured to the skin can create poor healing or necrosis of the stomal skin edge and retraction of the stoma into the abdomen. This is called Mucocutaneous separation.
- 50. What about pouching? ïŪ Pouch is first applied in surgery, but the stoma doesnât function for 2-4 days post-op. At first stomal drainage consists of mucus and serosanguinous fluid. As peristalsis returns, flatus and fecal drainage returns, usually in 2-4 days.
- 51. What do we need to observe and document? ïŪ Volume ïŪ Color ïŪ consistency
- 52. What about eating? ïŪ For the colostomy patient there are essentially no restrictions, but for the ileostomy patient it is important for some foods to be avoided to prevent an intestinal blockage.
- 53. What to avoid ïŪ Stringy, high fiber foods like celery, coconut, corn, coleslaw, the membranes on citrus fruits, peas, popcorn, spinach, dried fruits, nuts, pineapple, seeds, and fruit and vegetable skins.
- 54. Other food issues you need to know about ïŪ Fish, eggs, beer, and carbonated beverages can cause excessive foul odor. ïŪ Encourage your patients to eat at regular intervals, chew food well and drink adequate fluids. Avoid overeating and excessive weight gain.
- 55. What about the pouch? ïŪ The opening should be about 1/8 inch larger than the stoma. ïŪ Teach your patient to empty the pouch when it is no more than 1/3 full and to cleanse the pouch from the bottom with a squeeze bottle filled with water (one piece unit). The two piece unit can be snapped off, washed and snapped back on. ïŪ Change the entire unit (one or two piece) every 4-7 days depending on stability of seal.
- 56. Management options for permanent descending colostomy ïŪ Wearing a drainable pouch at all times ïŪ Colostomy irrigation to establish regularity and relieve constipation. Candidates for this option are assessed for past bowel habits and frequency of stools, location of colostomy, age, independence, dexterity, general health and personal preference.
- 57. One and two piece units #ffffff3trebuchet#ff0000#ff0000on
- 58. Ileostomy care ïŪ Why is ileostomy care so different from colostomy care? The drainage from the ileostomy contains proteolytic enzymes that literally digest the skin. That is why skin care is so important for your ileostomy patient.
- 59. Ileostomy care ïŪ The drainage is liquid in consistency, constant and extremely irritating to the skin. It is a dark green color initially that progresses to yellowish brown when the patient begins to eat.
- 60. Ileostomy care continued ïŪ Pay attention to fluid and electrolyte balance, especially potassium, sodium and fluid deficits!!!! ïŪ Fecal output can range from 1000- 1500ml every 24 hours. It should begin to decrease slightly within 10-15 days to an average of about 800 ml per day.
- 61. Ileostomy care continued ïŪ Careful I & O is essential ïŪ Instruct your patient to drink at least 1- 2 liters of fluid per day, more if they have diarrhea and in the summer when they are perspiring. ïŪ Encourage them to drink fluids rich in electrolytes.
- 62. Ileostomy care continued ïŪ Begin on low roughage diet. Chew food completely, avoid stringy, fiber foods to prevent blockage. ïŪ Ileal stoma also bleeds easily when touched.
- 63. Protect the skin! ïŪ Pouch with skin-protective barrier, adhesive backing, and pouch with opening cut no more than 1/8 inch larger than the stoma. ïŪ Empty the pouch when it is 1/3 full and change it immediately if it has begun to leak.
- 64. Important to know ïŪ If the terminal ileum is removed, your patient may need Vitamin B12 injections every 3 months. ïŪ Enteric-coated, time-released meds or hard tablets may not be absorbed in the patient who has had an ileostomy. Liquid or chewable meds are preferred.
- 65. More to know ïŪ Patients need vitamins A, D, E & K supplemented since colon absorption and synthesis are eliminated.
- 66. What if my ileostomy patient develops a food blockage? ïŪ Have them get into the knee-chest position and gently massage the area below the stoma. ïŪ Try a warm tub bath to help relax abdominal muscles. ïŪ Remove pouch and replace it with one that has a larger opening. ïŪ May take fluids only as long as not vomiting and passing some stool. If vomiting or not passing stool, take nothing by mouth and contact WOC(ET)N or MD.
- 67. Patient Teaching ïŪ The first step is looking at the stoma, progressing to assisting with emptying and cleaning, and then to changing the pouch. ïŪ If the patient cannot progress to the point of willingness to learn, a caregiver must be taught pouch change procedure and care until the patient is ready to learn
- 68. More teachingâĶâĶ ïŪ Pouch change is best performed before eating because the stoma is less active. ïŪ Ideally, the pouch should be changed every 5 to 7 days, but if it leaks it must be changed immediately.
- 69. Managing odor ïŪ Pouches are made of odorproof plastic, but if the bag is not cleaned adequately when emptied or if a leak has developed, there will be an odor. ïŪ There are products on the market to eliminate odorâĶdrops that can be put in the bag at changing or cleaning, odor neutralizing sprays when the pouch is changed, or bags with built in charcoal filters.
- 70. ïŪ There are also tablets that your patient can take by mouth that will eliminate the odor: Activated Charcoal Chlorophyllin Copper Bismuth Subgallate
- 71. When you teach ostomy care ïŪ Remind your patient how important it is to have them examine the peristomal skin for any sign of breakdown. It is so much easier to prevent this rather than heal the skin! ïŪ Patients may bathe or shower with or without the pouch. Patients may swim with the pouch in place as well.
- 72. Routine Skin Care ïŪ Proper method for pouch removal Gently peel pouch away from the skin while pressing down on or supporting the skin Avoid wiping the area with paper towels or toilet paper that leave a lot of lint behind.
- 73. Cleansing ïŪ Routinely wash with warm water. Soap is likely to leave a residue that can cause dermatitis and decrease the adhesiveness of the pouch. If soap is used be sure to avoid ones with oils and rinse thoroughly. ïŪ Commercial cleansing wipes are convenient when away from home as long as they donât contain lanolin or emollients. Tucks works well.
- 74. Shaving ïŪ Should be done routinely if peristomal skin is hairy to prevent folliculitis and pain with pouch removal.
- 75. More considerations ïŪ Remind your patients to not lift anything over 10 pounds for the first 6 to 8 weeks after surgery, otherwise they may resume normal activities.
- 76. And Finally ïŪ Before your patient is discharged they should be able to ïĄ Demonstrate cleaning and changing the pouch ïĄ Verbalize where to obtain supplies ïĄ Know how to contact a resource person for problems ïĄ Know how/when to follow up with physicians, WOCN, and support group.
- 77. Adaptation to a stoma ïŪ It is a gradual process because the patient experiences grief over the loss of a body part and an alteration in body image. ïŪ Adjustment period is individualized. ïŪ Patients are concerned about body image, sexual activity, family responsibilities and changes in lifestyle.
- 78. This concludes stoma care basics