SUFE presentation to upload 2
- 2. General Details Name : K. H. Age : 12 yrs Sex : Male Address : Strathbogie, Savanna-la-mar P.O
- 3. Private Practitioner PC; pain to left thigh x 5/7 HPC; no h/o trauma, unable to weight bear on left Rx. Diclofenac + Referral to OOPD
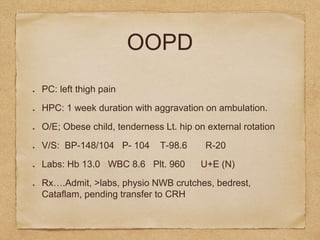
- 4. OOPD PC: left thigh pain HPC: 1 week duration with aggravation on ambulation. O/E; Obese child, tenderness Lt. hip on external rotation V/S: BP-148/104 P- 104 T-98.6 R-20 Labs: Hb 13.0 WBC 8.6 Plt. 960 U+E (N) RxŌĆ”.Admit, >labs, physio NWB crutches, bedrest, Cataflam, pending transfer to CRH
- 6. SUFEDr. E. M. Regis Jr. Dept. of Orthopaedics SPGH 14/12/15
- 8. Definition Slipped Upper Femoral Epiphysis (SUFE), aka Skiffy and SCFE is a unique type of instability of the proximal femoral growth plate due to weakness which involves the femoral head slipping off in a posterior direction. It usually develops shortly after puberty or periods of accelerated growth.
- 9. Anatomy The epiphysis is the rounded end of a long bone, at its joint with adjacent bone(s).
- 10. Anatomy (continued) Pressure epiphysis; region of long bone that forms the joint. eg. head of femur, part of the hip joint complex. assist in transmitting weight of human body and are regions of bone that are under pressure during movement and locomotion.
- 11. Incidence Most common in adolescent (10-16yrs) Overall US data. ..10.8 cases per 100,000. Black > Hispanic > White Male > Female {3:1) Left hip > Right hip 20% have bilateral involvement at time of presentation.
- 12. Aetiology Obesity (major risk factor) (more shear forces around proximal growth plate in hip) Genetics; - 5-7% familial involvement - metabolic endocrine disorders (hypothyroidism, hypogonadism, growth hormone abnormalities)
- 13. Pathophysiology unusually widened epiphyseal growth plate due to expansion of ŌĆ£zone of hypertrophyŌĆØ NORMAL PHYSIS ŌĆ”hypertrophic zone 15-30% SUFE PatientŌĆ”..hypertrophic zone 80%
- 14. Histologically abnormal cartilage maturation, endochondral ossification & perichondral ring instability occur, resulting in less organisation of normal cartilaginous columnar architecture. Slippage occurs through this weakened areas.
- 15. Position of proximal physis changes from horizontal to oblique during preadolescence and adolescence, redirecting hip forces from compression to shear. Also there is an association between femoral neck retroversion and reduced neck shaft angles with SUFE. These changes increase shear forces across hip, leading to SUFE.
- 16. Signs/Symptoms hip and/or knee pain intermittent limp/ unable to weight bear (antalgic) external rotation of limb (out toeing) apparent shortening limited R.O.M of hip loss of complete hip flexion + ability to fully rotate hip inward (painful internal rotation) involuntary guarding + spasm
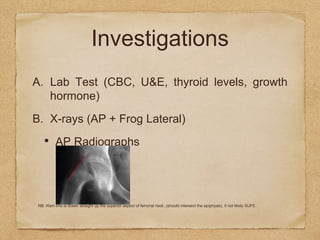
- 17. Investigations A. Lab Test (CBC, U&E, thyroid levels, growth hormone) B. X-rays (AP + Frog Lateral) ŌĆó AP Radiographs NB. Klein line is drawn straight up the superior aspect of femoral neck. (should intersect the epiphysis), if not likely SUFE.
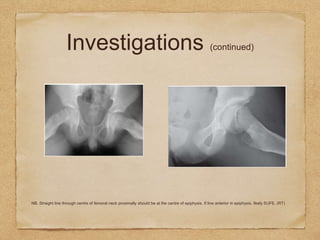
- 19. Investigations (continued) ŌĆó Frog Leg NB. Straight line through centre of femoral neck proximally should be at the centre of epiphysis. If line anterior in epiphysis, likely SUFE. (RT)
- 20. Investigations (continued) C. MRI D. CT SCAN E. Bone Scanning
- 21. Diagnosis Detailed History + Complete Physical Examination + Investigation Findings Classification Acute (<3 wks) Chronic (>3 wks) Acute on Chronic (3+ wks of symptoms with acute exacerbation/ change) Stable (weight bearing) Unstable (non weight bearing) Radiological (displacement of hip in relation to femoral neck) Type 1 < 33% Type 11 33-50% Type 111 >50%
- 22. Differential Diagnosis Femoral Head Avascular Necrosis Femoral Neck Fracture Femoral Neck Stress Fracture Femur Injuries + Fractures Groin Injury Osteitis Pubis (inflammation of pubis symphysis + surrounding muscle insertions)
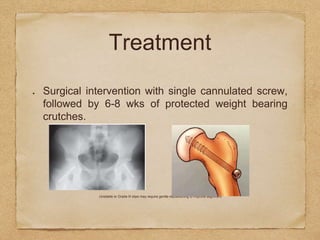
- 23. Treatment Surgical intervention with single cannulated screw, followed by 6-8 wks of protected weight bearing crutches. Unstable or Grade III slips may require gentle repositioning to improve alignment
- 24. Osteotomy of proximal femur as a secondary procedure may be indicated for repositioning of femoral head to improve functional R.O.M.
- 25. Wensaas et al study proved that routine prophylactic fixation of the contralateral hip is not indicated.
- 26. Prognosis Single screw in situ fixation in (stable) mild to moderate cases has good to excellent outcomes. Patients can resume contact sports & running after closure of growth plate. 20-50% rate of osteonecrosis in (unstable) severe cases.
- 27. Complications Avascular Necrosis Chondrolysis Degenerative Osteoarthritis Hardware Failure Post Op Infection Leg Length Inequality
- 28. Conclusion Early diagnosis is paramount taking into consideration high index of suspicion based on history and physical examination. X-ray findings are usually classic (klein line). Immediate surgical intervention should follow diagnosis and work up to aid in prevention of complications. (eg. AVN) Prognosis is usually good
- 29. References ApleyŌĆÖs System of Orthopaedics and Fractures, 9th Edition http://www.aafp.org/afp/2010/0801/p258.html http://orthoinfo.aaos.org/topic.cfm?topic=a00052 http://emedicine.medscape.com/article/91596-treatment www.google.com/images J Maheshwari (1997), Essential Orthopaedics 2nd Edn. New Delhi, Interprint www.orthobullets.com Savanna-la-mar General Public Hospital (SGPH) Docket Office