Syphilis new.pptx [repaired]
- 1. A 29 year old man came to the STD clinic complaining of multiple papules in his gentials. These papules quickly eroded and become tough. He later admitted to having unprotected sex with as ex worker
- 2. âĒThere was regional lymphadenopathy with moderately enlarged, firm, non suppurative, painless lymph nodes or satellite buboes. O/E we noticed papules which were indurated. It was painless.
- 3. âĒSo from the above case what can we assume âĒIts an STD
- 4. âĒThere after various tests âĒIt was found to be a case of Primary Syphilis âĒSyphilis comes under
- 5. Treponema-I Dr Ashish Jitendranath Associate Professor, Dept of Microbiology
- 7. Organism
- 8. Ultrastructure âĒLipid rich outer membrane- Increased susceptibility to detergents âĒShow hardly any antigenic variations âĒSaprophytic spirochetes are generally coarser. Endoflagella lie inside outer membrane and inserted at tapering portion
- 10. Motility
- 11. âĒCannot be grown in artificial culture media âĒCannot determine metabolic, physical and pathogenic features. âĒNon pathogenic trep is Reiter strain and Noguchi strain. âĒVirulent strains(eg. Nicholâs strain) has been maintained by serial passages in rabbit testicles âĒRecently grown in tissue cultures of rabbit epithelial cells
- 12. Epidemiology âĒModes of transmission âSexual contact âPlacenta âKissing âClose contact âContaminated fresh blood âĒFantastic history of syphilis with exact source not known. âĒAll known contacts post diagnosis needs to be considered.
- 13. Blood vessel and lymphatics Enters blood and dissipates to various organs in the body Pathogenesis Untreated Syphilis- Progress from 1. Primary 2. Secondary 3. Latent 4. Tertiary stages
- 14. Clinical features ( contd ) Veneral syphilis âĒOrganism divides 30-33 hours. âĒGenerally incubation period a month. âĒEarly spirochetemia inevitably develops during this phase âĒLeft untreated at least 2/3 spontaneously clear âĒ1/3 progress
- 15. Those that progress after 3 weeks Bacteria multiply at initial entry site and progress to form a chancre on the genital. Painless chancre Usually single except immunocompromised patients Superficial Ulcer has clean appearance and no exudate. Painless or slightly tender to touch
- 16. Primary syphilis âĒIndurated and superficially ulcerated âĒBase usually smooth, borders raised and firm and cartilaginous consistency. âĒKnown as Hard chancre âĒMost common site penis, cervix or labia and anal canal, rectum or mouth âĒRegional lymphadenopathy consisting of enlarged, firm, non suppurative, painless lymph nodes or satellite buboes accompanies primary lesion âĒChancre heals within 3-6 weeks and 2-12 weeks later the symptoms of secondary syphilis develops
- 17. Secondary syphilis âĒClinically most florid stage of infection âĒInvolves skin âĒMultiplication and wide dissemination of spirochete and last until sufficient host response develops to exert some immune control. âĒBegins 2-8 weeks after appearance of chancre.
- 18. Secondary syphilis âĒNonpruritic macular, maculopapular, papular or pustular lesions. Begin on the trunk and proximal extremities. Any surface area becomes involved. âĒMacules evolve to papules. Other sites palms, soles, hair follicles.
- 19. Secondary syphilis âĒWarm, moist intertriginous areas ( perianal area, vulva, scrotum, inner aspects of thigh, skin under breast) papules enlarge, coalesce and erode to produce painless, broad, moist, gray- white to erythematous highly infectious plaques termed condylomata lata
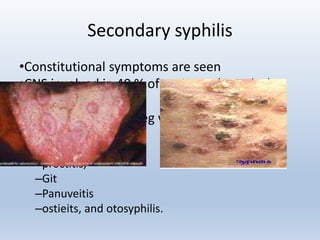
- 21. Secondary syphilis âĒConstitutional symptoms are seen âĒCNS involved in 40 % of patients. ( Headache and meningismus). âĒAny organ involved, eg with âRenal involements, âsyphilitis hepatis âproctitis, âGit âPanuveitis âostieits, and otosyphilis.
- 22. Latent syphilis âĒPeriod of quiescence. âĒNo clinical manifestation âĒSerological tests. âĒIndividuals with late latent syphilis are not considered infectious. âĒMay still transmit infection. âĒEarly latent syphlis is when clinical relapse occurs. âĒDiagnosis during this period using serological tests.
- 23. Late syphilis âĒSlowly progressive destructive inflammatory disease that can affect any organ in body to produce clinical illness 5-30 or more years after initial infection. âNeurosyphilis âCardiovascular syphilis âGummatous- rare granulomatous lesion of skeleton, skin and mucocutaneous tissues
- 24. Congenital syphilis âĒWomen with early syphilis can infect her fetus much more commonly(75-90%) than with syphilis over 2yrs duration(35%) âĒLesions of congenital- develop 4th month of gestation when fetal immune competence starts appearing (suggests pathogenesis requires immune response from fetus) âĒCongenital syphilis prevent if given adequate treatment âĒAbortions normal.
- 25. NON-VENEREAL SYPHILIS âĒOccupationally in doctors or nurses the natural evolution is as in venereal syphilis, except that the chancre is extragenital, usually on fingers âĒIn syphilis transmitted by blood transfusion,1 Ė chancre does not occur âĒTransplacental transmission-any stage of pregnancy
- 26. Lab Diagnosis
- 27. Specimen âĒCollected with care. âĒLesion cleared with a guaze soaked in warm saline & the margins gently scraped âĒGentle pressure applied to the base of lesion & serum that exudes is collected âĒBlood also is taken âĒSerous transudate from moist lesions- Primary chancre, condyloma latum or mucous patch
- 28. Direct examination âĒPrimary, secondary and early congenital syphilis- Immunostaining, PCR, darkfield examination âĒWet film prepared by exudate examined under dark ground microscope âĒNeeds to be differentiated from saprophytes âĒNot specific and requires 104 per ml of spirochetes.
- 29. âĒIn case lesions is cleaned with antiseptic-Direct immunofluorescent antibody staining and immunohistochemical staining better. âĒBest observed from chancre, condyloma and mucous patches. âĒ3 negatives before final.
- 30. Biopsy specimen âĒWarthin starry stain. âĒLevaditi and Fontaina method are silver staining methods. âĒPreferred methods of staining is immunohistochemical staining.
- 31. MAJOR SEROLOGICAL TESTS FOR SYPHILIS A.Non-specific(Reagin Ab) tests using cardiolipin Ag (STANDARD TESTS FOR SYPHILIS) oWasserman complement fixation reaction oKahn flocculation test oVDRL test oRapid plasma reagin(RPR) oAutomated RPR oVDRL-ELISA test B. Group specific test using cultivable treponemal(Reiter strain) Ag oReiter protein complement fixation(RPCF) test
- 32. C.Specific tests using pathogenic treponemes(T. Pallidum) Treponema pallidum Immobilisation(TPI) test Fluorescent Treponemal Antibody-Absorption(FTA-ABS) Treponema Pallidum Haemagglutination Assay(TPHA) Treponema Pallidum Enzyme Immunoassay(TP-EIA)
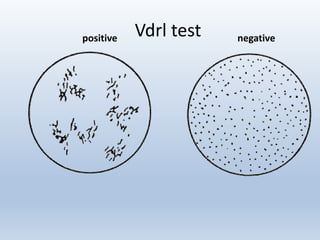
- 33. VDRL TEST FOR SYPHILIS âĒType of slide flocculation test âĒIn this inactivated serum(heated at 56Ëc for 30 mins) is mixed with cardiolipin Ag on a special slide & rotated for 4 mins âĒCardiolipin forms visible clumps on combining with reagin Ab âĒReaction read under low power microscope as reactive, weak or non. âĒMonitor patients response to therapy
- 34. RPR âĒCommon test in labs now. âĒEmploys carbon particles and read macroscopically. âĒBlack carbon particles are bound to caridolipin, when mixed with positive serum on disposable card. âĒAgglutination is easily observed. âĒProzone phenomenon in upto 2% of cases especially in secondary and pregnancy
- 36. RPR âĒAdvantages âEnables the result to be read by eye âUseful in field studies âRPR done with unheated serum or plasma âFingerprick sample is sufficient âĒDis advantages âCant test CSF
- 37. âĒTrust-Toloudine red unheated serum test. âĒInstead of carbon particle we use toloudine red âĒAutomated reagin antibody test-
- 38. âĒ4 fold change in titre important. âĒHighest prevalence during secondary syphilis. âĒQuantitative test should become non reactive 1 year after treatment in primary and 5 years in secondary.
- 39. BIOLOGICAL FALSE POSITIVE(BFP) REACTIONS âĒAs cardiolipin Ag is present both in T.Pallidum and in mammalian tissues, reagin Abs may be induced by treponemal or host tissue antigens which accounts for BIOLOGICAL FALSE POSITIVE(BFP) âĒBFP defined as âpositive reactionsâ obtained in cardiolipin tests, with negative results in specific treponemal tests, in the absence of past or present treponemal infections and not by technical faults âĒThey represent non-treponemal cardiolipin antibody responses
- 40. ïą BFP Ab is usually IgM while Reagin Ab in syphilis is IgG ïąRepresent non treponemal cardiolipin Ab responses ïąClinically BFP reactions classified as acute & chronic ïąAcute BFP-last only for weeks or months, associated Ä acute infections, injuries or inflammatory conditions ïąChronic BFP-persist longer than 6 months, seen in SLE & other collagen diseases Other conditions associated Ä BFP reactions r leprosy, malaria, relapsing fever, infectious mononucleosis, hepatitis & tropical eosinophilia
- 41. âĒTo avoid BFP reactions, tests using cultivable treponemes(REITER STRAIN) as Ags were developed âĒMost common-Reiter Protein Complement Fixation(RPCF) using lipopolysaccharide-protein complex Ag derived fron treponeme âĒSensitivity & specificity- lower than tests using T. Pallidum âĒRPCF-generally free from BFP but gave false positive reactions GROUP SPECIFIC TREPONEMAL TESTS
- 42. Specific test- Nichols strain âĒTPI- âHistorical concept âAbility of Antibody + complement to immobilize live T. pallidum visualized under darkground microscope. âĒFlurescent treponemal antibody- âIndirect Immunofluorescence test using smears prepared on slides with Nicholâs strain of T.Pallidum
- 43. âĒFTA- Absorption- Patients serum first absorbed with non pathogenic trep antigen ( sorbent ) to remove low titer, natural cross reacting antibodies âĒDifficult to standardize hence Particulate agglutination test is preferred.
- 45. T.PALLIDUM HAEMAGGLUTINATION ASSAY(TPHA) âĒUses tanned ethrocytes sensitized with a sonicated extact of T.Pallidum as Ag âĒTest sera for TPHA are absorbed with a diluent containing components of the Reiter treponeme,rabbit testis & sheep erythrocytes âĒSera screened at initial dilution of 1:80 but titres of 5120 or more-common in 2Ëstage âĒTPHA-as specific as FTA-ABS, almost sensitive except in 1Ë âĒThese advantages have made TPHA-Standard Confirmatory Test
- 46. FREQUENCY OF REACTIVE SEROLOGICAL TESTS IN UNTREATED SYPHILIS(%) Stage VDRL/RPR FTA-ABS TPHA Primary 70-80 85-100 65-85 Secondary 100 100 100 Latent/Late 60-70 95-100 95-100
- 47. Other tests âĒEnzyme immunoassays âĒRapid agglutinationa test âĒWestern blotting
- 48. Congenital syphilis âĒIgM immunoblotting- presence of IgM in neonates confirm diagnosis. âĒBest way of monitoring is with serial quantitative non treponemal tests. âĒMost reliable is test mother at time of birth
- 49. Neurosyphilis âĒVDRL is preferred reagin test âĒConfirmed with TPHA
- 50. Molecular techniques âĒNew age treatment with molecular techniques like PCR have made it more specific.
- 51. Treatment
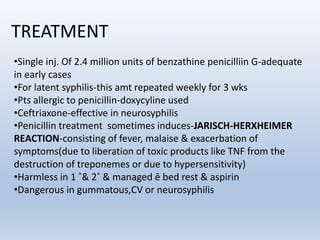
- 52. TREATMENT âĒSingle inj. Of 2.4 million units of benzathine penicilliin G-adequate in early cases âĒFor latent syphilis-this amt repeated weekly for 3 wks âĒPts allergic to penicillin-doxycyline used âĒCeftriaxone-effective in neurosyphilis âĒPenicillin treatment sometimes induces-JARISCH-HERXHEIMER REACTION-consisting of fever, malaise & exacerbation of symptoms(due to liberation of toxic products like TNF from the destruction of treponemes or due to hypersensitivity) âĒHarmless in 1 Ë& 2Ë & managed Ä bed rest & aspirin âĒDangerous in gummatous,CV or neurosyphilis
- 53. Nonvenereal treponematoses ENDEMIC SYPHILIS ïąCommon in young children ïąPrimary chancre is not seen, except sometimes on nipples of mothers infected by their children ïąUsually seen with manifestation of secondary syphilis ,such as mucous patches &skin eruptions ïąDisease progresses to tertiary lesions ,particularly gummatous ïąLab diagnosis &treatment same as venereal syphilis
- 54. Yaws âĒCausative agent is T.pallidum subspecies pertenue âĒThe primary lesion(mother jaw) is an extra genital papule which enlarges & breaks down to form ulcerating granuloma âĒAs in syphilis 2Ë & 3Ë manifestations follow âĒDestructive gummatous lesions of the bones are common âĒInfection by direct contact, flies may act as mechanical vectors âĒLab diagnosis & treatment are same as for venereal syphilis
- 55. PINTA âĒCausative agent is T.carateum âĒThe primary lesion is an extra genital papule which does not ulcerate but develops into a lichenoid/psoriaform patch âĒSecondary skin lesions are charecterized by hyperpigmentation/hypopigmentation âĒTissues other than skin are seldom effected
Editor's Notes
- First case 1905 John Hunterâs unfortunate self-inoculation with urethral pus containing both Neisseria gonorrhoeae and T. pallidum only served to prolong misconception s, because the two diseases were considered the same for some time thereafter. However, by the mid-19th century, the cause, epidemiology, and clinical manifestations of syphilis were well known
- Outer membrane is lipid rich This has led to the hypothesis that this microorganism acts as a âstealthâ organism by minimizing the number of surface membraneâbound targets for the hostâs immune system to recognize until a sufficient number of spirochetes are present.
- The genome consists of a single circular chromosome of approximately 1,138,006 base pairs, which places it close to the lowest end of the range for bacteria. Unlike most pathogenic bacteria, its genome lacks apparent transposable elements, suggesting that the genome is extremely conserved and stable
- 11
- 14
- Unless secondarilyinfected, the ulcer has a clean appearance and no exudate; it is painless or slightly tender to the touch, a conspicuous aspect of the ulcerative
- The secondary or disseminated stage becomes evident 2 to 12 weeks (mean, 6 weeks) after contact. This generalized condition with parenchymal, constitutional, and mucocutaneous manifestations occurs when the greatest number of treponemes (high antigen load) is present in the body, particularly in the bloodstream The classic and most commonly recognized lesions involve the skin. Nonpruritic macular, maculopapular, papular, or pustular lesions, and combinations and variations thereof, all occur.
- After the secondary stage subsides, the untreated patient enters a latent period, during which the diagnosis can be made only by obtaining a positive serologic test response for syphilis. Because relapses of secondary syphilis in immunocompetent persons can occur up to 4 years after contracting syphilis, this period is divided into early latent (relapses possible) and late latent (relapses very unlikely) stages; 75% of relapses occur within the frst year and are likely a consequence of waning immunity.
- 21
- 22
- Cardiovascular syphilis Consist of lesions including aneurysms, chronic granulomata and meningovascular manifestation. Gummatous syphis Rare granulomatous lesion of skeleton, skin or mucocutaneous tissues. Neurosyphilis Neurological manifestation such as tabes dorsalis or general paralysis
- 24
- Direct diagnostic methods include the detection of T pallidum by microscopic examination of fluid or smears from lesions, histological examination of tissues or nucleic acid amplification methods such as polymerase chain reaction (PCR). Indirect diagnosis is based on serological tests for the detection of antibodies. Serological tests fall into two categories: nontreponemal tests for screening, and treponemal tests for confirmation
- 29







![Syphilis new.pptx [repaired]](https://image.slidesharecdn.com/syphilisnew-190407075658/85/Syphilis-new-pptx-repaired-9-320.jpg)








![Syphilis new.pptx [repaired]](https://image.slidesharecdn.com/syphilisnew-190407075658/85/Syphilis-new-pptx-repaired-20-320.jpg)


















![Syphilis new.pptx [repaired]](https://image.slidesharecdn.com/syphilisnew-190407075658/85/Syphilis-new-pptx-repaired-44-320.jpg)