Tb,typhoid
- 1. ULCERS OF INTESTINE INTESTINAL TYPHOID AND TUBERCULOSIS DR SRABANI CHAKRABARTI ASSOCIATE PROFESSOR DEPT OF PATHOLOGY , CNMC
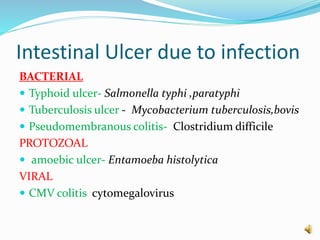
- 5. Intestinal Ulcer due to infection BACTERIAL ÔÇó Typhoid ulcer- Salmonella typhi ,paratyphi ÔÇó Tuberculosis ulcer - Mycobacterium tuberculosis,bovis ÔÇó Pseudomembranous colitis- Clostridium difficile PROTOZOAL ÔÇó amoebic ulcer- Entamoeba histolytica VIRAL ÔÇó CMV colitis cytomegalovirus
- 6. Topics ÔÇóTB of intestine ÔÇóTyphoid of intestine
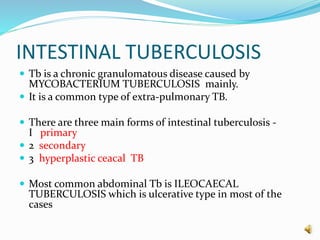
- 7. INTESTINAL TUBERCULOSIS ÔÇó Tb is a chronic granulomatous disease caused by MYCOBACTERIUM TUBERCULOSIS mainly. ÔÇó It is a common type of extra-pulmonary TB. ÔÇó There are three main forms of intestinal tuberculosis - I primary ÔÇó 2 secondary ÔÇó 3 hyperplastic ceacal TB ÔÇó Most common abdominal Tb is ILEOCAECAL TUBERCULOSIS which is ulcerative type in most of the cases
- 8. Primary intestinal TB  MODE OF INFECTION  In pre- pasturisation era, ingestion of unpasturised cow’s milk infected with MYCOBACTERIUM BOVIS.  Due to pasturisation of milk and after eradication of tuberculosis in cattle nowadays primary intestinal TB is caused by MYCOBACTERIUM HOMINIS.
- 9. Primary Intestinal Tb ÔÇó In primary TB predominant change is in regional mesenteric lymph node without any significant intestinal lesion. GROSS ÔÇó the lymph nodes are enlarged, matted and caseous. H/P MICROSCOPY ÔÇó Tuberculous granuloma with caseation necrosis.
- 10. SECONDARY TUBERCULOSIS ÔÇó Secondary TB occurs in a patient of active pulmonary TB who swallows the sputum and the lesion develops in intestine. ÔÇó Most common site of intestinal TB is terminal ileum. ÔÇó Hyperplastic caecal TB is a type of secondary TB where lesion is in caecum and ascending colon clinically the lesion presents as palpable mass.
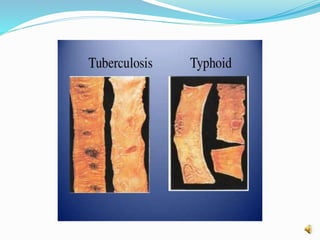
- 11. Secondary tuberculosis MACROSCOPIC ÔÇó Lesions of intestine are prominent than lymph node. ÔÇó Large ulcer that is transverse to the long axis of bowel ÔÇó serous surface may show visible tubercle. ÔÇó Healed lesion may form transverse fibrous stricture and obstruction. H/P MICROSCOPY ÔÇó mucosa and submucosa show ulceration and typical granuloma of TB.
- 13. Gross appearance of TB intestine tubercle on serosal surface
- 14. microscopy of TB intestine
- 15. Typhoid fever Typhoid fever or enteric fever is an acute systemic disease caused by S . typhi and S. paratyphi. MODE OF TRANSMISSION ÔÇó Salmonella is ingested through contaminated food or water ÔÇó Finger to mouth contact with faeces, urine or other secretion.
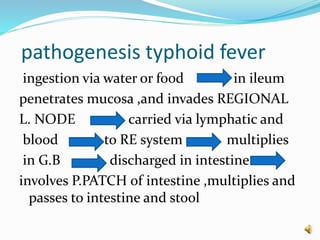
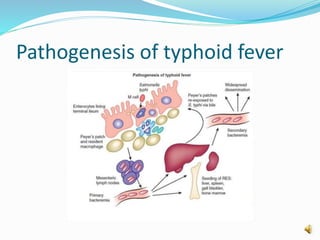
- 16. pathogenesis typhoid fever ingestion via water or food in ileum penetrates mucosa ,and invades REGIONAL L. NODE carried via lymphatic and blood to RE system - multiplies in G.B discharged in intestine involves P.PATCH of intestine ,multiplies and passes to intestine and stool
- 17. Pathogenesis of typhoid fever
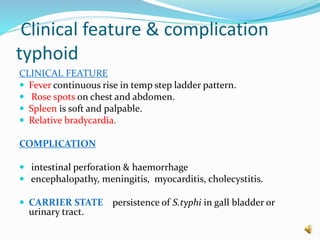
- 19. Clinical feature & complication typhoid CLINICAL FEATURE ÔÇó Fever continuous rise in temp step ladder pattern. ÔÇó Rose spots on chest and abdomen. ÔÇó Spleen is soft and palpable. ÔÇó Relative bradycardia. COMPLICATION ÔÇó intestinal perforation & haemorrhage ÔÇó encephalopathy, meningitis, myocarditis, cholecystitis. ÔÇó CARRIER STATE persistence of S.typhi in gall bladder or urinary tract.
- 20. TYPHOID INTESTINE MACROSCOPY OF INTESTINAL LESION  most commonly in terminal ileum.  Peyer’s patches in the terminal ileum enlarges and shedding of mucosa produces TYPHOID ULCER which are oval ulcer with their long axis along the long axis of bowel.  Base of the ulcer is black due to sloughed mucosa.  the margins of the ulcer are slightly raised.  Fibrosis is not significant.
- 21. Typhoid intestine MICROSCOPY  mucosa - oval ulcer over peyer’s patch  Lamina propria -macrophage containing bacteria RBC lymphocyte , plasma cell ,neutrophil
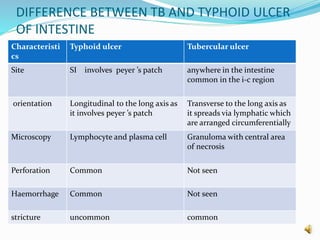
- 23. DIFFERENCE BETWEEN TB AND TYPHOID ULCER OF INTESTINE Characteristi cs Typhoid ulcer Tubercular ulcer Site SI involves peyer ’s patch anywhere in the intestine common in the i-c region orientation Longitudinal to the long axis as it involves peyer ’s patch Transverse to the long axis as it spreads via lymphatic which are arranged circumferentially Microscopy Lymphocyte and plasma cell Granuloma with central area of necrosis Perforation Common Not seen Haemorrhage Common Not seen stricture uncommon common