The limping child by dr issam saif
- 1. BBYY DDRR.. EESSSSAAMM HHOOZZAAYYEENN SSAAIIFF oorrtthhooppeeddiicc ssppeecciiaalliisstt AALLDDHHAAIIDD HHOOSSPPIITTAALL
- 2. DDeeffiinniittiioonn ’ü« LLiimmpp iiss ddeeffiinneedd aass aann uunneevveenn,, jjeerrkkyy ggaaiitt,, uussuuaallllyy ccaauusseedd bbyy ppaaiinn,, wweeaakknneessss,, oorr ddeeffoorrmmiittyy .. ’ü« LLiimmpp ccaann bbee ccaauusseedd bbyy bbootthh bbeenniiggnn aanndd lliiffee-- tthhrreeaatteenniinngg ccoonnddiittiioonnss,, tthhee mmaannaaggeemmeenntt vvaarriieess ffrroomm rreeaassssuurraannccee ttoo mmaajjoorr ssuurrggeerryy ddeeppeennddiinngg uuppoonn tthhee ccaauussee ..
- 3. DDIIFFFFEERREENNTTIIAALL DDIIAAGGNNOOSSIISS ’ü«BBoonneess.. ’ü«JJooiinnttss.. ’ü«SSoofftt ttiissssuuee.. ’ü«NNeeuurroollooggiiccaall..
- 4. ’ü«BBoonnee:: FFrraaccttuurreess.. LLeegggg--CCaallvv├®├® --PPeerrtthh''ss.. SSlliippppeedd ccaappiittaall ffeemmoorraall eeppiipphhyyssiiss.. TTuummoorrss.. VVaassoooocccclluussiivvee ccrriissiiss ooff ssiicckkllee cceellll ddiisseeaassee (( tthhee ppaaiinn iiss sseevveerr,, ssoommee ttiimmeess eeqquuaall ttoo ccaanncceerr ppaaiinn))
- 5. ’ü«JJooiinnttss:: TTrraannssiieenntt ssyynnoovviittiiss SSeeppttiicc aarrtthhrriittiiss AAccuuttee rrhheeuummaattiicc ffeevveerr JJuuvveenniillee rrhheeuummaattooiidd aarrtthhrriittiiss DDeevveellooppmmeennttaall ddyyssppllaassiiaa ooff tthhee hhiipp HHeemmaarrtthhrroossiiss:: ttrraauummaattiicc,, hheemmoopphhiilliiaa SSyysstteemmiicc lluuppuuss eerryytthheemmaattoossiiss..
- 6. ’ü«SSoofftt ttiissssuuee:: VViirraall mmyyoossiittiiss..(( hhiigghh lleevveell ooff sseerruumm ccrreeaattiinniinnee kkiinnaass )) IInnttrraammuussccuullaarr vvaacccciinnaattiioonn.. CCeelllluulliittiiss..
- 7. ’ü«NNeeuurroollooggiiccaall:: CCeerreebbrraall ppaallssyy PPeerriipphheerraall nneeuurrooppaatthhyy MMeenniinnggiittiiss.. EEppiidduurraall aabbsscceessss ooff tthhee ssppiinnee..
- 8. ’ü«IInnffeeccttiioouuss:: ’ü« SSeeppttiicc aarrtthhrriittiiss ’ü« OOsstteeoommyylliittiiss ’ü« ddeesscciittiiss ’ü«NNoonn--IInnffeeccttiioouuss ’ü« IInnffllaammmmaattiioonn ’ü« TTrraauummaa ’ü« TTuummoorr ’ü« BBoonnyy ddeeffoorrmmiittyy ’ü« AAsseeppttiicc nneeccrroossiiss
- 9. Age ŌĆō specified conditions that cause a limp 1-3 years DDH Child abuse Neuromuscular disease Leg length discrepancy Infections 4-10 years Transient synovitis Perth's disease Infections leg length discrepancy >10 years SCFE OVERUSE SYNDROME all age groups Trauma Tumors
- 10. 8.5% 5.3% 2.8% 6.0% 77.4% Transient synovitis SCFE Infection Perthes' disease Other The Limping Child
- 11. Physical examination should started with observation of the gait *Gait is a repeated cycle of limb motion controlled by muscle activity that carries the body forward *The gait cycle is traditionally described as starting when one heel strikes the ground and ending when it strikes the ground again *There is two phases of the gait cycle (60% stance phase and 40% swing phase) *The progress of gait as following: initial contact---loading response---mid stance---terminal stance---preswing ŌĆöinitial swing---mid swing---terminal swing.
- 13. Prior to the heel strikeŌĆ”relaxation of the hamstrings ms & contraction of quadriceps ms >>>>straightening of knee joint>>>>contraction of the dorsiflexors of the ankle & foot >>>>heel strike. which followed by flat foot ( loading response)>>>>motion of the body forward over the foot ( mid stance )>>>> contraction of the calf ms >>>>planter flexion( heel off)>>>>knee flexion >>>>toe off & beginning of the swing phase by contraction of the iliopsoas ms >>>> flexion of the hip>>>> knee flexion & contraction of the ankle dorsiflexors ( acceleration or preswing phase)>>>>midswing phase =midstance phase of the other limb (moving of the body with ipsilateral limb forward >>>>deceleration occur to start new heel strike ( by contraction of Q.ms & hamstring ms relaxation to make the knee straight >>>> new heel strike
- 14. Other components of the gait: 1- pelvic tilt during normal gait , the pelvis dropped at the side of swing limb by 5 degrees below the horizontal plane 2- pelvic rotation during swing phase the pelvis rotates anteriorley by 4 degrees & on the stance side the pelvis rotates posteriorely by 4 degrees 3- lateral shift during the stance phase the pelvis & trunk shifted laterally toward the stance limb by one inch N.BŌĆ”. Pelvic tilt ,pelvic rotation , lateral shift, knee flexion,, knee -ankle ŌĆōfoot motion >>>>minimize the shift of the gravity body centre in both vertical & horizontal axis's 4- width of the base by the examiner behind the pt.= distance between both foot during double support= 2-4 inches 5- stride length the distance between the heel strike of limb & the next heel strike of the same limb 6- step length The distance between heel strike of one limb & heel strike of the other limb
- 15. PATHOLOGICAL GAIT Child limp may be caused by pain, structural changes, weakness or a combination of these. Most of abnormalities occur at the stance phase. For example: 1-antalgic gait (anti-pain) in which the child limits the time spent on the painful leg in stance phase 2-leg length discrepancy gait the pt. can compensate by walking on tip-toe on the short side and with slight hip and knee flexion on the long side 3-trendelenburg gait is a painless limp in a pt. with weakened hip abductor muscles the pt. leans over the affected side. bilateral involvement causes waddling gait 4-gait in cerebral palsy there is brain lesion with secondary muscle contracture and compensatory movements.
- 16. 5- foot slap gait: due to weakness of the ankle & foot dorsiflexors=drop foot during the swing phase 6- G. maximums gait: during midstance >>>the ipsilateral hip must be maintained in extension or the trunk falls forward .if there is weakness of the G.M >>the pt. push his trunk posteriorly resulting in extension lurch or G.M. gait. 7- calceneal gait: weakness of calf ms or flat foot( loss of planter flexion >>> loss of heel off) 8- hip ŌĆōhike gait: pt. with stiff knee >>> may elevate the ipsilateral pelvis to hold the foot up. = circumduction gait 9- wide based gait: the width of the base is more than 4 inches ==( cerebellar lesion ) >>> loss of coordination >>> execive shift of the gravity centre
- 17. HHIISSTTOORRYY ’ü« DDuurraattiioonn aanndd ccoouurrssee ooff tthhee lliimmpp?? ’ü« HHiissttoorryy ooff ttrraauummaa ?? ’ü« AAssssoocciiaatteedd ssyymmppttoommss ((ee..gg..,, ffeevveerr,, wweeiigghhtt lloossss,, aannoorreexxiiaa,, bbaacckk ppaaiinn,, aarrtthhrraallggiiaa,, vvooiiddiinngg oorr ssttoooolliinngg pprroobblleemmss)) ’ü« IIff ppaaiinn iiss pprreesseenntt,, wwhheerree iiss iitt llooccaatteedd,, wwhheenn ddooeess iitt ooccccuurr,, aanndd wwhhaatt iittss sseevveerriittyy?? ’ü« DDooeess tthhee lliimmpp iimmpprroovvee oorr wwoorrsseenn wwiitthh aaccttiivviittyy??
- 18. ’ü« Recent history of viral iillllnneessss oorr ssttrreeppttooccooccccaall iinnffeeccttiioonn ((ppoosstt iinnffeeccttiioouuss aarrtthhrriittiiss)).. ’ü« RReecceenntt hhiissttoorryy ooff nneeww oorr iinnccrreeaasseedd ssppoorrttss aaccttiivviittyy ’ü« RReecceenntt hhiissttoorryy ooff iinnttrraammuussccuullaarr iinnjjeeccttiioonn ((ccaann ccaauussee mmuussccllee iinnffllaammmmaattiioonn oorr sstteerriillee aabbsscceessss)) ’ü« HHiissttoorryy ooff eennddooccrriinnee ddyyssffuunnccttiioonn ((mmaayy pprreeddiissppoossee ttoo sslliippppeedd ccaappiittaall ffeemmoorraall eeppiipphhyyssiiss)) ’ü« FFaammiillyy hhiissttoorryy ooff ccoonnnneeccttiivvee ttiissssuuee ddiissoorrddeerr,, iinnffllaammmmaattoorryy bboowweell ddiisseeaassee,, hheemmoogglloobbiinnooppaatthhyy,, bblleeeeddiinngg ddiissoorrddeerr,, oorr nneeuurroommuussccuullaarr ddiissoorrddeerr
- 19. Physical examination Standing: * back should be examined for scoliosis ,local tenderness, range of motion. *if there is pelvic tilt is present , it can be measured by placing blocks under the shorter leg until the pelvis in level (horizontal) . *trendelenburg test *skin dimples ,hairy patches over lumbar spine Supine: * each joint should be examined separately *look for swelling, feel for tenderness, assess the ROM *for hip flexion contracture --------Thomas test *abdomen should always examined ------may be appendicitis *neurological examination should be performed *check for leg length discrepancy , the short leg must be differentiated from apparent shortening that is caused by scoliosis or pelvic obliquity or joint contracture. Prone: *hip rotation * femoral anteversion
- 20. HHiipp rroottaattiioonn ’ü« IInntteerrnnaall rroottaattiioonn ooff tthhee hhiippss :: iiss ppeerrffoorrmmeedd wwiitthh tthhee cchhiilldd iinn tthhee pprroonnee ppoossiittiioonn wwiitthh tthhee kknneeeess fflleexxeedd;; tthhee aannkklleess aanndd ffeeeett aarree tthheenn rroottaatteedd aawwaayy ffrroomm tthhee bbooddyy ttoo ccoommppaarree tthhee aammoouunntt ooff iinntteerrnnaall rroottaattiioonn iinn tthhee ssyymmppttoommaattiicc vveerrssuuss tthhee aassyymmppttoommaattiicc hhiipp..
- 22. GGaalleeaazzzzii tteesstt :: TThhee GGaalleeaazzzzii tteesstt iiss uusseeffuull iinn ddiiaaggnnoossiinngg ddeevveellooppmmeennttaall hhiipp ddyyssppllaassiiaa oorr lleegg lleennggtthh ddiissccrreeppaannccyy.. TThhiiss tteesstt iiss ppeerrffoorrmmeedd bbyy ppuuttttiinngg tthhee cchhiilldd iinn aa ssuuppiinnee ppoossiittiioonn aanndd tthheenn fflleexxiinngg tthhee hhiippss aanndd kknneeeess bbyy bbrriinnggiinngg tthhee aannkklleess ttoo tthhee bbuuttttoocckkss .. TThhee tteesstt iiss ppoossiittiivvee wwhheenn tthhee kknneeeess aarree ooff ddiiffffeerreenntt hheeiigghhttss.. AAbbnnoorrmmaall sshhoorrtteenniinngg ooff tthhee lleegg ccaann bbee ccaauusseedd bbyy DDDDHH,, PPeerrtthh''ss ddiisseeaassee..
- 24. TTrreennddeelleennbbuurrgg tteesstt :: ’ü« AAsskkiinngg tthhee cchhiilldd ttoo ssttaanndd oonn tthhee aaffffeecctteedd lleegg,, ccaauusseess aa ppeellvviicc ttiilltt ((tthhee uunnaaffffeecctteedd hhiipp iiss lloowweerr))..
- 26. RRAADDIIOOLLOOGGIICC EEVVAALLUUAATTIIOONN ’ü« PPllaaiinn rraaddiiooggrraapphhss :: MMoosstt cchhiillddrreenn wwhhoo lliimmpp rreeqquuiirree rraaddiiooggrraapphhiicc eevvaalluuaattiioonn.. BBootthh aanntteerrooppoosstteerriioorr aanndd llaatteerraall vviieewwss sshhoouulldd bbee oobbttaaiinneedd.. TThhee ffrroogg-lleegg vviieeww ooff tthhee ppeellvviiss pprroovviiddeess tthhee llaatteerraall vviieeww ooff tthhee ffeemmoorraall hheeaaddss..
- 27. ’ü« UUllttrraassoonnooggrraapphhyy :: UUllttrraassoonnooggrraapphhyy iiss aann eexxcceelllleenntt tteecchhnniiqquuee ffoorr iiddeennttiiffyyiinngg ssmmaallll jjooiinntt eeffffuussiioonnss ooff tthhee hhiipp aanndd sshhoouulldd bbee uusseedd wwhheenn ppllaaiinn rraaddiiooggrraapphhss aarree nnoorrmmaall bbuutt tthhee ssuussppiicciioonn ooff sseeppttiicc aarrtthhrriittiiss rreemmaaiinnss hhiigghh.. ’ü« AA ddiiffffeerreennccee ooff mmoorree tthhaann 22 mmmm bbeettwweeeenn tthhee aanntteerriioorr jjooiinntt ccaappssuullee aanndd tthhee ffeemmoorraall nneecckk iiss ccoonnssiiddeerreedd ssiiggnniiffiiccaanntt..
- 28. ’ü« al Ultrasonography alssoo mmaayy bbee uusseedd ttoo gguuiiddee aassppiirraattiioonn ooff tthhee hhiipp ((ee..gg..,, iissoollaatteedd uunniillaatteerraall hhiipp eeffffuussiioonn iinn aa ffeebbrriillee cchhiilldd)).. ’ü« BBiillaatteerraall eeffffuussiioonnss ssuuggggeesstt aa ssyysstteemmiicc aarrtthhrriittiicc ddiissoorrddeerr oorr ttrraannssiieenntt ssyynnoovviittiiss bbeeccaauussee aass mmaannyy aass oonnee-qquuaarrtteerr ooff ppaattiieennttss wwiitthh ssyymmppttoommaattiiccaallllyy uunniillaatteerraall ttrraannssiieenntt ssyynnoovviittiiss hhaavvee bbiillaatteerraall eeffffuussiioonnss..
- 29. ’ü« RRaaddiioonnuucclliiddee ssccaannss :: BBoonnee sscciinnttiiggrraapphhyy iiss aa sseennssiittiivvee mmeeaannss ooff ddeetteeccttiinngg aalltteerraattiioonnss iinn tthhee mmeettaabboolliicc rraattee ooff bboonnee aanndd tthhuuss aa sseennssiittiivvee mmeeaannss ooff llooccaalliizziinngg ppaatthhoollooggyy.. ’ü« HHoowweevveerr,, bboonnee sscciinnttiiggrraapphhyy llaacckkss ssppeecciiffiicciittyy bbeeccaauussee ssuucchh aalltteerraattiioonnss iinn bboonnee mmeettaabboolliissmm ccaann ooccccuurr iinn LLeegggg- CCaallvv├®├®-PPeerrtthheess ddiisseeaassee,, oosstteeoommyyeelliittiiss,, oosstteeooiidd oosstteeoommaa,, aanndd mmaalliiggnnaanntt bboonnee ttuummoorrss..
- 30. CCTT aanndd MMRRII ’ü« CCTT ssccaannnniinngg iiss uusseeffuull iinn tthhee ddiiaaggnnoossiiss ooff ddeeeepp ssoofftt ttiissssuuee iinnffeeccttiioonnss ooff tthhee PPaarraa ssppiinnaall aanndd rreettrrooppeerriittoonneeaall rreeggiioonnss.. ’ü« MMRRII iiss uusseeffuull iinn tthhee eevvaalluuaattiioonn ooff tthhee ssppiinnee ((ffoorr ddiisscciittiiss oorr ssppiinnaall ttuummoorrss)),, ssoofftt ttiissssuuee ttuummoorrss aanndd aabbsscceesssseess iinn tthhee PPaarraa ssppiinnaall aanndd rreettrrooppeerriittoonneeaall rreeggiioonnss,, oosstteeoommyyeelliittiiss ooff tthhee ppeellvviiss aanndd lloonngg bboonneess,, aanndd iinn LLeegggg-CCaallvv├®├®-PPeerrtthheess ddiisseeaassee
- 31. LLAABBOORRAATTOORRYY EEVVAALLUUAATTIIOONN ’ü« CCoommpplleettee bblloooodd ccoouunntt ((CCBBCC)),, EESSRR oorr CCRRPP,, aanndd bblloooodd ccuullttuurree aarree uusseeffuull iinn tthhee eevvaalluuaattiioonn ooff ffeebbrriillee ppaattiieennttss aanndd tthhoossee iinn wwhhoomm iinnffeeccttiioonn iiss bbeeiinngg ccoonnssiiddeerreedd ’ü« .. CCBBCC aanndd EESSRR oorr CCRRPP aallssoo sshhoouulldd bbee ccoonnssiiddeerreedd iinn tthhee eevvaalluuaattiioonn ooff tthhee aaffeebbrriillee cchhiilldd wwiitthh aa sseevveerraall ddaayy hhiissttoorryy ooff lliimmpp aanndd nnoo aabbnnoorrmmaalliittiieess oonn ppllaaiinn rraaddiiooggrraapphhyy..
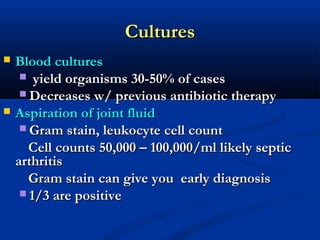
- 32. CCuullttuurreess ’ü« BBlloooodd ccuullttuurreess ’ü« yyiieelldd oorrggaanniissmmss 3300--5500%% ooff ccaasseess ’ü«DDeeccrreeaasseess ww// pprreevviioouuss aannttiibbiioottiicc tthheerraappyy ’ü« AAssppiirraattiioonn ooff jjooiinntt fflluuiidd ’ü«GGrraamm ssttaaiinn,, lleeuukkooccyyttee cceellll ccoouunntt CCeellll ccoouunnttss 5500,,000000 ŌĆōŌĆō 10000,,000000//mmll lliikkeellyy sseeppttiicc aarrtthhrriittiiss GGrraamm ssttaaiinn ccaann ggiivvee yyoouu eeaarrllyy ddiiaaggnnoossiiss ’ü« 1//33 aarree ppoossiittiivvee
- 33. THE BLOOD SUPPLY OF FEMORAL HEAD: The main sources of blood supply to the proximal femur from medial and lateral circumflex vs.each of which arise from the profunda femoris artery. Additional supply from: superior gluteal artery artery of ligamentum teres
- 35. ’ü«DDDDHH TThhee LLiimmppiinngg CChhiilldd:: AAggee 1 ŌĆōŌĆō 33 ’ü«DDeevveellooppmmeennttaall DDyyssppllaassiiaa ooff tthhee HHiipp
- 36. Pathological changes in DDH : * Acetabulum shallowŌĆöthe roof sloops too steeply * Femoral head dislocated superiorly and posteriorŌĆödelayed ossific centre * femoral neck anteverted * capsule stretched hourglass appearance by iliopsoas tendon * limbus superiorly the acetabular labrum and its capsular edge may be pushed into the socket by the dislocated head , this fibrocartilage structure may obstruct closed reduction * ligamentum teres elongated and hypertrophied which may obstruct the reduction
- 39. Imaging studies * before age of 6 months diagnosis can be done by U/S * plain x-ray is more helpful after age of 6 months ( appearance of the ossific nucleus of the head *HilgenreinerŌĆÖs line *PerkinsŌĆÖs line Position of the femoral head in relation to this two lines *Acetabular index Is the angle between hilgenreiner line & the roof of the acetabulum, it should be below 30 degree by the age of one year & below 25 degree by 2 years age *Center edge angle is the angle between the Perkins line & line pass through the edge of the acetabulum & the center of the head . It becomes smaller as the hip subluxated. normally is 20 degree or greater.
- 40. Imaging findings
- 42. Treatment of DDH At age of 0---6 ms: pavlik harness Age of 6---15 ms: gentle closed reduction under G.A. & maintenance of a located position for 2ŌĆö3 ms in a spica cast usually stabilize the joint , any residual dysplasia must treated by bracing or surgery. Age of 15---2yrs: *open reduction *femoral shortening osteotomy ; may be needed at time of open reduction to reduce tension on the soft tissue & reduce the risk of AVN of the femoral head . *Capsulorrhaphy * cast spica Age above 2 yrs Significant residual dysplasia is present so the surgical correction is needed to creates a stable mechanical environment that permits remodeling to normal joint during growth * femoral osteotomy to correct the ant version and valgus deformity to be done before age of 4 yrs to stimulate normal growth of the acetabulum * pelvic osteotomy to increase the femoral head covering needed by the acetabulum examples innominate osteotomyŌĆöpemberton acetabuloplastyŌĆöDega osteotomyŌĆō chiari osteotomy (medial displacement osteotomy)
- 43. TThhee LLiimmppiinngg CChhiilldd:: AAggee 33 ŌĆōŌĆō 66 TTrraannssiieenntt ssyynnoovviittiiss ’ü« CChhiilldd rreeffuusseess ttoo wwaallkk ’ü« MMoovveemmeenntt ooff hhiipp iiss ppaaiinnffuull ’ü« MMaayy hhaavvee ffeevveerr ’ü« MMooddeerraatteellyy eelleevvaatteedd WWBBCC ’ü« LLaassttss aa ffeeww ddaayyss ’ü« DDiissaappppeeaarrss wwiitthhoouutt ttrreeaattmmeenntt
- 44. TTrraannssiieenntt ssyynnoovviittiiss ’ü« CCoommmmoonnllyy ooccccuurrss aafftteerr aa rreessppiirraattoorryy iillllnneessss.. ’ü« XX rraayy iimmaaggee mmaayy bbee nnoorrmmaall ’ü« UUllttrraassoouunndd mmaayy sshhooww eeffffuussiioonn ’ü« MMaaiinn ttrreeaattmmeenntt iiss bbeedd rreesstt aanndd pphhyyssiiootthheerraappyy.. ’ü« NNoonn--sstteerrooiiddaall aannttii--iinnffllaammmmaattoorryy ddrruuggss aarree uusseeffuull ffoorr ttrreeaattmmeenntt aanndd ccaann sshhoorrtteenn tthhee dduurraattiioonn ooff ssyymmppttoommss iinn cchhiillddrreenn
- 45. D.D. : the most difficult and important differential diagnosis is septic arthritis of the hip: The clinical finding are similar but there is high temperature in septic arthritis. In a recent study , four independent parameters were used to distinguish the two entities: fever (more than 38.5). CRP more than 20 mgL. ESR greater than 40 mm/h. serum white blood count more than 12000 cells. non wt bearing.
- 46. SSeeppttiicc aarrtthhrriittiiss oorr oosstteeoommyyeelliittiiss ’ü« BBlloooodd ccuullttuurreess aarree ccoommmmoonnllyy ppoossiittiivvee ’ü« RRaaiisseedd wwhhiittee cceellll ccoouunntt aanndd CC rreeaaccttiivvee pprrootteeiinn,, wwhhiicchh nnoorrmmaalliizzeess mmoorree rraappiiddllyy tthhaann eerryytthhrrooccyyttee sseeddiimmeennttaattiioonn rraattee oonnccee iinnffeeccttiioonn iiss bbrroouugghhtt uunnddeerr ccoonnttrrooll ’ü« XX rraayy iimmaaggeess sshhooww ddeellaayyeedd cchhaannggeess.. RRaaddiiooggrraapphhiicc eevviiddeennccee ooff aaccuuttee oosstteeoommyyeelliittiiss ffiirrsstt iiss ssuuggggeesstteedd bbyy oovveerrllyyiinngg ssoofftt ttiissssuuee ooeeddeemmaa aatt 33--55 ddaayyss aafftteerr iinnffeeccttiioonn.. BBoonnyy cchhaannggeess aarree nnoott eevviiddeenntt ffoorr 1144--2211 ddaayyss aanndd iinniittiiaallllyy mmaanniiffeesstt aass ppeerriioosstteeaall eelleevvaattiioonn ffoolllloowweedd bbyy ccoorrttiiccaall oorr mmeedduullllaarryy lluucceenncciieess.. ’ü« BByy 2288 ddaayyss,, 9900%% ooff ppaattiieennttss sshhooww ssoommee aabbnnoorrmmaalliittyy..
- 47. SSeeppttiicc aarrtthhrriittiiss WIDENED JOINT SPACE
- 48. ’ü« Joint aspiration iiss tthhee ddeeffiinniittiivvee ddiiaaggnnoossttiicc pprroocceedduurree aanndd tthhee mmoosstt ccoommmmoonn ppaatthhooggeenn iissoollaatteedd iiss SSttaapphhyyllooccooccccuuss aauurreeuuss
- 49. Perth's disease: Is a serious but ŌĆō limited pediatric hip disorder , more common in boys, It affects age 4ŌĆö10 years old. Is generally unilateral. Pathological changes: initially , the AVN episodes are silent and asymptomatic ,as the bone of the proximal femoral epiphysis dies, it is revascularized---osteoclast remove dead bone while osteoblast simultaneously lay down new bone on a dead trabeculas ( during this phase the femoral head is mechanically weak) which lead to fragmentation and collapse of the bony structure causing flattening and deformity of the ossific nucleus and femoral head . The newly formed bone has the shape of the collapsed head. The symptomatic collapse phase rarely exceeds 1-1 ┬Į years but full revascularization and remodeling may continue silently for several years. C/P : painless limp ,if pain is presents , it may be mild and referred to the thigh or knee. atrophy of the thigh ms limited ROM ŌĆōtypically pt has a flexion contracture of 0-30 degree, loss of abduction and loss of internal rotation of the hip.
- 50. Radiological study: early by plain x-ray ------NAD but can be diagnosed early by MRI late by plain x-ray-----deformed head ( flattened ŌĆō fragmented ) Treatment : no treatment for children less than 5 yrs old----with less than ┬Į of the head involvement (why ?) most of the head is cartilaginous------and there is good time for remodeling. Non-operative: most experts agree that children who maintain excellent motion ( particularly abduction greater than 30 degree in absence of flexion contracture ) may not require intervention. (abduction bracing ) Operative : varus femoral osteotomy Salter osteotomy
- 52. TThhee LLiimmppiinngg CChhiilldd:: AAggee 1100 ŌĆōŌĆō 1144 SSCCFFEE ’ü« Risk factors: Obesity, inflammatory (neglected septic arthritis), hypothyroidism, hypopituitarism. Clinical presentation: Pain-limping ŌĆō discomfort in the hip , groin, medial thigh, is accentuated by running , jumping . Antalgic gait , out toeing . Preslipage: slight discomfort Acute slip : sever painŌĆödeformity (external rotation, adduction)ŌĆö limited ROM (internal rotation and abduction) Acute on chronic: pain ,limp over several months which is suddenly becomes very painful Chronic : mild symptoms ,pain , limp, external rotation during walking, mild to moderate shortening of the affected leg, atrophy of the thigh muscles
- 53. TThhee LLiimmppiinngg CChhiilldd:: AAggee 1100 ŌĆōŌĆō 1144 SSCCFFEE Always get a frog lateral view Always check the other side
- 55. Treatment : *avoid moving or rotating the leg, the patient should not allow to walk . *analgesia *determine if it is acute (less than 3 weeks) or chronic (+ 3weeks) *determine whether stable( able to weight bearing) or unstable (non-weight bearing) *determine the radiological type of the SCFE ***Surgical intervention by immediate internal fixation using a single cannulated screw is the treatment of choice . ***Femoral osteotomy is a secondary procedure to relocate the head within the acetabulum to improve the ROM ***Bone graft epiphysiodesis follow up : non-weight bearing for at least 6-8 weeks then start physiotherapy
- 56. Child abuse An important cause of limping or fracture in a child,particulary in those younger than 2 years . It is important to look for skin manifestations such as bruises , burns . Metaphyseal corner fracture are typical of child abuse, as pull and twist that create these fracture are rarely accidental. Overuse syndrome Children who have very recently undergone a significant growth spurt have less joint flexibility and are more prone to injury : Spondylolysis (common in female gymnasts) Iliac apophysitis ( seen in adolescent runner) Osgood- Sclutters disease ( the most common condition around the knee) Severs disease ( it is characterized by pain at the calcaneal apophysis )
- 59. TTHHAANNKKSS FFOORR The Limping Child YYOOUURR AATTTTEENNSSIIOONN